BEIs - ACGIH
advertisement
®
®
TLV and BEI Committees:
The Decision Making Process
Presented at AIHce
May 13, 2003, Dallas, TX
Bill Wells PhD, CIH, CSP, Moderator
Dennis Casserly, PhD, CIH & Marilyn Hallock, CIH Monitors
Forum Overview
•
•
•
•
•
Pat Breysse:
Introduction
Lisa Brosseau: TLV®-CS Committee
Larry Lowry:
BEI® Committee
Tom Bernard:
TLV®-PA Committee
Ken Martinez:
Bioaerosols Committee
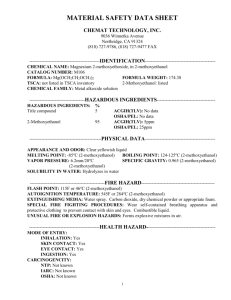
ACGIH,
the TLVs® and BEIs®
®
Patrick N. Breysse, PhD, CIH
Johns Hopkins University
Bloomberg School of Public Health
Chair, ACGIH®
What Is ACGIH®?
• Membership Society (founded in 1938)
• Not-for-profit, Non-governmental
Association (501(c)(6) organization)
• Multi-Disciplinary Membership
• Traditionally Neutral on Public Positions
Membership
April 2003
4%
3%
Government
& Academia
Private
Industry
& Others
48%
Regular
Associate
Student
Retired
45%
Membership by
Profession, 2003
Industrial Hygienist
39%
Administrator/Manager
12%
OH&S Professional
6%
Environmental Professional
4%
Safety Professional
3%
Other (Engineer, Scientist,
Toxicologist, Professor, etc.)
~36%
Technical
Committees
Committees provide the creativity,
initiative, and technical expertise that
has made ACGIH® what it is today and
what it will be tomorrow.
.
Core Mission
ACGIH Members
Board of Directors
Ex. Director
& Staff
Exposure
Assessment
Criteria
Assessment
& Control
Methodology
BEI
Air Sampling
Instruments
TLV-CS
Bioaerosols
TLV-PA
Industrial
Ventilation
Occupational
Sector
Applications
Professional
& Intersociety
Coordination
Administration
&
Governance
Taskforces
Agr S&H
Computer
Awards
Air Sampling
Procedures
Construction
International
Finance
AIHA/ACGIH
Outreach
Infectious
Agents
PCC
AIHA/ACGIH
Nominating
Public
Positions
Small
Business
ACGIH® Statement
of Position
®
ACGIH is not a standards setting body.
TLVs® and BEIs® –
• Are an expression of scientific opinion.
• Are not consensus standards.
• Are based solely on health factors; it may
not be economically or technically feasible
®
®
to meet established TLVs or BEIs .
ACGIH® Statement
of Position
TLVs and BEIs –
®
®
• Should NOT be adopted as standards
without an analysis of other factors
necessary to make appropriate risk
management decisions.
• Can provide valuable input into the risk
characterization process. The full written
®
Documentation for the numerical TLV or
BEI® should be reviewed.
Conflict of Interest
• Basis for Conflicts of Interest:
– Employment
– Financial benefit
– Personal
– Professional
• Avoid perceived as well as real conflict
of interest
Conflict of Interest
• Committee members serve as
individuals
– they do not represent organizations and/or
interest groups
• Members are selected based on
expertise, soundness of judgement, and
ability to contribute
Full disclosure of
possible conflicts of
interest
Committee
and
subcommittee
chairs
Discussion within full
committee and
subcommittees
Management of
perceived and
real COIs
Board of Directors Oversight
COI Process at ACGIH®
Today’s Roundtable
•
•
•
•
Chemical Substances - TLV
Biological Exposure Indices (BEI)
Physical Agents – TLV
Bioaerosols Committee
®
®
ACGIH TLVs for
Chemical Substances
Committee Update
Chair: Lisa M. Brosseau, ScD, CIH
Associate Professor
University of Minnesota
School of Public Health
Overview
• TLV®-CS Committee has 20 members
and 3 member-candidates, who
volunteer time towards developing
scientific guidelines and publications
– Primary goal is to serve the scientific
needs of industrial hygienists
– Committee expenses (travel) are
supported by ACGIH®
– Time is donated by the members
Committee Structure
• Chair and Vice Chair
• Three Subcommittees, Chair and Co-Chair
– Dusts & Inorganics (D&I)
– Hydrogen, Oxygen & Carbon Compounds (HOC)
– Miscellaneous Compounds (MISCO)
• Administrative Subcommittees
–
–
–
–
Communications and Outreach
Membership
Notations
Chemical Substance Selection
• Staff Support
– Liaison, Clerical, Literature Searching
Chemical Substance
Subcommittees
• Approximately 10 members on each
• Membership from academia, government,
unions, industry
• Membership represents four key
disciplines:
–
–
–
–
Industrial hygiene
Toxicology
Occupational Medicine
Occupational Epidemiology
®
Core TLV Principles
• Focus on airborne exposures in
occupational settings
• Utilize the “threshold” concept
• Primary users are industrial hygienists
• Goal is towards protection of “nearly all”
workers
Technical, economic, and analytic
feasibility are NOT considered
Committee Actions
in 2003
• Adopted TLVs® for 22 substances
• Proposed 6 new TLVs®
– (listed on the Notice of Intended Changes (NIC))
• Revised 7 adopted TLVs® (listed on the NIC)
• Proposed withdrawing TLVs® for methane,
ethane, propane, butane and liquified
petroleum gas. (Will also withdraw iso-butane.)
– All to be replaced with a proposal for Aliphatic
Hydrocarbon Gases, Alkane (C1-C4)
• Revised 3 proposals for TLVs® and retained on
the NIC
Committee Actions
in 2003 (Cont’d)
• Adopted a new Appendix E for Particulates
(Insoluble or Poorly Soluble) Not Otherwise
Specified (PNOS)
• Developed new Documentation for 2
substances (no change in values)
• Changed the name of one TLV® and kept on
the NIC with revised recommendations
• Retained 4 proposed TLVs® on the NIC
• Withdrew 2 proposed TLVs® from the NIC
Committee Actions
in 2003 (Cont’d)
• Proposed withdrawal of Appendix B:
Substances of Variable Composition
• Proposed revision of Appendix C:
Threshold Limit Values for Mixtures
• Proposed a new Appendix F:
Commercially Important Tree Species
Identified as Inducing Sensitization
Substances and Issues
Under Study in 2003
• 115 chemical substances currently under study
• Issues under study include:
–
–
–
–
Ceiling limits, excursions, and STELs
Notations for reproductive effects
Skin notation
Reciprocal Calculation Procedure, Group Guidance
Values for refined C5 - C15 aliphatic and aromatic
hydrocarbon solvents and constituent chemicals
Particulates
(Insoluble or Poorly Soluble)
Not Otherwise Specified
• The recommendations are guidelines (not TLVs®)
for limiting exposure to insoluble particles:
– 3 mg/m3 (respirable)
– 10 mg/m3 (inhalable)
• Apply to particles that:
–
–
–
–
Do not have a TLV®
Are insoluble or poorly soluble in water or lung fluid
Have low toxicity (not genotoxic, cytotoxic, etc.)
Only toxic effects are inflammation or “lung overload”
mechanisms
Proposed
New Appendix C:
TLVs® for Mixtures
• In the absence of other information, assume
additivity of substances having similar effects
– Same outcomes, same target organs or systems
If
C C
T T
1
2
1
2
C
...
T
n
1
n
the TLV® for the mixture has been exceeded.
Proposed
New Appendix C:
TLVs® for Mixtures
• Recommends using the TLV®
Documentation, as well as the TLV®
Basis information in the book
• Where possible, only combine TLVs®
having a similar time basis
– Table showing appropriate combinations of
different types of TLVs®
Proposed
New Appendix C:
TLVs® for Mixtures
• Limitations and Special Cases
– Do not use when suspect inhibition or
synergism
– Take care when considering mixtures of
A1, A2, or A3 carcinogens
– Not appropriate for complex mixtures with
many different components (e.g., gasoline,
diesel exhaust)
Committee Activities
• Notations
– Complete re-write of Introduction to the TLV®-CS section
of the book
– Improved definition and categorization of TLV® Basis
• Communications
– Symposia on substances under study
• Membership
– Recruitment, especially of physicians and
epidemiologists
– Bill Wagner Award & member recognition
• Chemical Substance Selection
– Refining the selection process
Committee Activities
• Sponsored symposium on TDI (Spring 2002)
• Attended ACGIH® symposium on oil mists
and metalworking fluids (Fall 2002)
• Plenary talk on TLVs® at AIOH in Australia
(Winter 2002)
• Co-sponsored a colloquium on Workplace
Chemical Exposure Standards with IRSST in
Montreal (Spring 2003)
Committee Plans
• Co-sponsor symposium on enzymes
(Spring 2004)
• Roundtables on TLVs® at other
professional meetings (SOT, ACOEM)
• Joint meetings with ACGIH® BEI® and
AIHA WEEL Committees
Questions?
Scheduled Break
Take a minute to stretch!
Biological Exposure Indices
®
(BEIs )
Process and Use
Larry K. Lowry, Ph.D.
Chair, ACGIH® BEI® Committee
The University of Texas Health Center at Tyler
Where are we going
today?
•
•
•
•
•
•
•
Current definitions of the BEI®, 2002
The development of BEIs®
The key – Documentation
Examples
Biomonitoring without limits
Current and future issues
Resources
Biological monitoring.
Why?
• Assess exposure and uptake by all routes
– TLV® not protective – skin
– Includes workload
– More closely related to systemic effects
• Assess effectiveness of PPE
• Legal or ethical drivers
– Regulations
– Control workers’ compensation costs
“Guidelines”
for
biological
monitoring –
®
The BEIs
The BEIs – 2003
®
BEIs® are intended for use in the
practice of industrial hygiene as
guidelines or recommendations to
assist in the control of potential
workplace health hazards and for
no other use.
The BEI – Definition
®
• Biological monitoring … entails
measurement of the concentration of a
chemical determinant in the biological
media of the exposed and is an indicator
of the uptake of the substance.
• The BEI® determinant can be the
chemical itself; one or more metabolites;
or a characteristic reversible biochemical
change induced by the chemical.
®
BEIs
• Represent levels of determinants that are
most likely to be observed in specimens
collected from a healthy worker who has
been exposed to chemicals to the same
extent as a worker with inhalation exposure
to the TLV®-TWA.
• Generally indicate a concentration below
which nearly all workers should not
experience adverse health effects.
Current basis for BEIs
• Bio-equivalent to TLV (traditional)
®
– “BEIs® represent levels of determinants
that are most likely to be observed in
specimens collected from a healthy worker
who has been exposed to chemicals to the
same extent as a worker with inhalation
exposure to the TLV®-TWA.”
• Most of the BEIs® are based on TLVs®
®
Current basis
• Indicators of early, reversible health effect
– Approach developed in late 80’s as
relationships did not always exist between
airborne exposure and biomonitoring
determinant.
• Examples:
– CO, Acetyl cholinesterase inhibiting
pesticides, Cd, Pb, Hg, Hexane-MnBK
®
The BEI Committee
Larry Lowry, Ph.D., U TX Health Center at
Tyler – Chair
•
•
•
•
•
•
•
•
•
•
Phil Edelman, MD, CDC – Vice Chair
Mike Morgan, Sc.D, CIH, U. of WA – Past Chair
Joe Saady, Ph.D., VA Division of Forensic Science
Leena Nylander-French, Ph.D, CIH, UNC, Chapel Hill
John Cocker, Ph.D., HSE, UK
K. H. Schaller, Dipl. Ing., Univ Erlangen, Germany
M. Ikeda, Ph.D., Kyoto Ind Health Assoc, Japan
Gary Spies, CIH, Pharmacia
Glenn Talaska, Ph.D., CIH, Univ of Cincinnati
Jan Yager, Ph.D., EPRI
®
BEI development
• Volunteer assigned document
• Prepares draft Documentation
• Sources of data
– Human laboratory & workplace data
• Limited use of animal data
– Simulation modeling with verification
– Published peer-reviewed data
• Draft Documentation discussed in committee
meetings, e-mail
Development Process
Select
Chemical
Review
Data
Assign
Author
Develop
Feasibility
BEI®?
Yes
Prepare
Draft
Review
Draft
Revise
No
Final
Document
Yes
Return to
Author
Discuss
Justification
Select
Determinant
No
How are chemicals
selected?
•
•
•
•
•
Chemicals with human data
Potential for dermal absorption
Availability of adequate lab methods
Recommendations by others
Interest/experience of committee
member
The Documentation
• Who is the audience?
– The practicing occupational hygienist or other
practicing occupational health professional
• What the Documentation is
– Justification supporting the BEI®
– Practical information on sampling, background, etc.
• What the Documentation is not
– An extensive review of toxicological data
– A novel research approach to setting guidelines
The Documentation –
contents
•
•
•
•
•
Basis of the BEI®
Uses and properties
Absorption
Elimination
Metabolic pathways & biochemical
interactions
• Possible non-occupational exposure
• Summary of toxicology
For each index
®
or BEI
•
•
•
•
Analytical methods, sampling, and storage
Levels without occupational exposure
Kinetics
Factors affecting interpretation
– Analytical procedures and sampling
– Exposure
– Population
• Justification – the key
• Current quality of database
• Recommendations and references
The notations
• B - Background levels expected
• Nq- Nonquantitative
– Biol. monitoring recommended, no BEI®
• Ns- Non-Specific
– Needs confirmation
• Sq Semiquantitative (but specific)
– Screening test
– Confirmatory tests
Practical applications
• Bioavailability of metals – Chromium
– Chromium VI (water soluble) fume
• Specificity and Sensitivity – Benzene
biomonitoring
– t,t-Muconic acid in urine (t,t-MA)
– S-Phenylmercapturic acid in urine (SPMA)
Bioavailability of
metals – Chromium
• Physical properties and solubility
– Cr (III), very insoluble particulates
– Cr (VI) insoluble particulate – the lung carcinogen
– Cr (VI) water soluble
• Fume as generated in MMA arc welding
• Mist as generated in electroplating
• Health effects of Cr (VI) water soluble
– Fume – lung irritant
– Mist – chrome ulcers on skin, mucus membranes
Biological monitoring
of Cr exposure
• Cr (III) inappropriate – not bioavailable
• Cr (VI) insoluble – not bioavailable
• Cr (VI) water soluble
– If fume, use BEI® based on welding studies
– If mist, bioavailability less
• See chrome ulcers at “acceptable” BEI® values
Biomonitoring of benzene
Biomonitoring at
®
the current TLV
• t,t-Muconic acid in urine (t,t-MA)
– Good sensitivity (to 0.1 ppm benzene)
– HPLC methodology
– Considerable variability in populations
• S-Phenylmercapturic acid in urine
(SPMA)
– Ultimate sensitivity (to 0.01 ppm benzene)
– GC/MS methodology
– Good data base, but expensive
Biological monitoring
without limits
• What about substances
absorbed through the skin
and with chronic systemic
health effects that occur after
a long lag time such as
cancer?
The traditional
approach
• Cannot relate to airborne limits, TLVs®
– Irrelevant
• Cannot relate to skin absorption
– Difficult to quantitate dermal dose
• Cannot relate to health effect
– Often wrong timeline
• What to do?
®
The BEI approach
• Rationale
– Biological monitoring is essential to assess
dermal exposure
– How do you correlate dermal dose with a
biomarker of exposure?
• Nq Approach
– “Biological monitoring should be considered
for this compound based on the review;
however, a specific BEI® could not be
determined due to insufficient data.”
Criteria for an Nq
• Dermal route of exposure significant
• Good measurement methods
• Good qualitative data on human exposure and
biomarker concentration
• Poor quantitative data relating exposure &
biomarker
• Long lag time, exposure to health outcome
• Low or no background in general population
If criteria are met,
then
•
•
•
•
•
•
•
Develop full Documentation
Describe sampling and analysis
Define background levels
Describe justification for biomonitoring
Note the lack of quantitative data
Cite guidance values from literature
Publish BEI® as Nq (no value)
Examples – MBOCA
• Principal route of exposure – dermal
• Alleged health effect in humans – cancer
• Good methods and human data on
exposure-response
• Industry practice guidance from the HSE
Health and Safety
Executive, UK
• Scientific basis to justify guidance values
• Use "yardstick or benchmark" approach
• Issues
– Results – no "safe" or "unsafe" exposure levels
– Results – estimates of exposure areas and allow
intervention to reduce exposures
– No legal status
• Examples – MBOCA and MDA
The “yardstick or
benchmark” approach
• Good analytical methods
• All specimens analyzed by one
laboratory or with a single method
• Establish "best industry practice" using
an upper 90% confidence limit of the
"best" industries
• Benchmarks – guidance value to provide
users with assessment of their results
Current issues
• Carcinogens?
– Is there a safe level of exposure?
– The German EKA approach
• Mixtures and interactions
– Metabolism/toxicokinetics on pure chemical
– Workers exposed to mixtures
– How does this effect BEI®?
• Biomarkers of effect – irreversible effects?
• Data gaps – lack of human data
• Animal data – should this be used?
Skin absorption
Justification for
®
BEI
– Existing BEIs® for substances with
substantial skin absorption
• MBOCA – Nq
• EGME/EGMEA – Nq
• EGEE/EGEEA – 100 mg/g creatinine
– (based on TLV® of 5 ppm)
– Is this a valid approach?
• Are Nq notations appropriate?
• Should a chemical without a “skin” notation
have a BEI®?
The future
• As TLVs® drop, BEIs® based on TLVs® drop
– Cannot distinguish exposure at TLV® from
background
• What do we do for substances that have no
human data?
• What is the future of modeling techniques?
– Can these modeling techniques be validated?
• Should animal data be used?
• What about mixtures?
Other guidelines
Germany
The
BATs
from the
DFG
The HSE –
UK
Biological
monitoring
guidelines
Guidance from WHO –
How to do biological
monitoring
Other
Guidelines
New edition,
2001
Thank you for your attention
Your questions please
Scheduled Break
Take a minute to stretch!
®
®
ACGIH TLVs for
Physical Agents
Committee Update
Vice-Chair: Thomas Bernard
University of South Florida
College of Public Health
TLV®
Physical Agents Committee
Process for Hazardous Agent Selection
and Decision Making
Mission
To foster, solicit, collect and evaluate data
on potential health hazards of exposures
to physical agents. When appropriate,
recommend ACGIH® Threshold Limit
®
Values for physical agents.
2002 PAC
Harry Mahar
Maurice Bitran
Thomas Bernard
Gerald Coles
Anthony Cullen
Daniel Johnson
John Leonowich
William Murray
Bhawani Pathak
Robert Patterson
Thomas Tenforde
Carla Treadwell
Consultants:
Thomas Adams
Thomas Armstrong
Gregory Lotz
Martin Mainster
Gary Myers
Overview
• Physical Agents
• Process
– Committee Activities
– TLV® Development
• Future
– Format
– Agents
Disclaimer
The opinions expressed here are those of
the author
and not of
his employer,
the Physical Agents Committee or
the ACGIH® Worldwide.
Physical Agents
It’s the Movement of Energy
Risk of Health
Effects
• What is the nature of the energy?
• How much energy?
• What is the interaction with tissue?
Nature of Energy
• Electric and Magnetic Fields
• Photons
• Kinetic Energy
– Pressure
– Vibration
– Mechanical
• Heat
Amount of Energy
• Total Amount of Energy Absorbed
– What does it take to raise water temperature?
• Rate of Absorption (Power or Intensity)
– How fast does the temperature rise?
• Normalized to Surface Area
(e.g., mJ/cm2, mW/cm2)
Interactions
• Electric and Magnetic Fields
– Induce Currents
– Align Molecules
– Vibrate Molecular Bonds
• Photons
– Vibrate Molecular Bonds
– Disrupt Molecular Bonds
More Interactions
• Mechanical Disruption of Tissue
– Pressure
– Vibration
– Force Applications
• Loss of Tissue Function
– Thermal: Gain or Loss of Heat
Bernard Watt-O-Meter
{Not Accepted, or Considered Acceptable, by Any Authority}
Power Limits for Various Exposures [mW/cm2]
Electric and Magnetic Fields
170,000
Radiofrequency/Microwave
1.0
Infrared Light
10
Blue Light
0.0001
Ultraviolet Light
0.0012
Ionizing Radiation
0.00000003
Noise
0.00003
Heat Stress
30
Exposure
• Energy Distribution in the Immediate
Environment
• The distribution is usually described as
Power or Intensity (directly or through a
surrogate) versus Frequency or
Wavelength in Bands
Exposure Threshold
• Total Energy
– Ability to Absorb Energy
• Rate of Energy (Power or Intensity)
– Ability to Dissipate Absorbed Energy
In a Band
Integrated Over All Bands
Process
Committee Activities
Development of TLVs®
Representation
• Usually one or two members with an
expertise for a particular agent (e.g., a small
portion of the electromagnetic spectrum)
• Small committee to maintain a working and
collegial group. We meet as a whole.
• Leverage with outside experts
Updating TLVs
®
• PAC meets with outside experts
• Members bring recommendations to the
PAC for discussion
• Consideration of actions taken by
national and international committees or
agencies
New TLVs
®
• Quintessential Example: Hand Activity
• Formed a cadre of consultants
• Convened a conference
• Developed recommendation and
Documentation
• Presented to PAC and discussed
• PAC voted after internal deliberations
Future
Format
Agents
Format
• TLV® Book
– Use of Flow Charts
– Evolving (see Heat Stress and RF/MW)
• Training
• Documentation
– Expanded and Focused (see HAL and Lifting)
– Health Effects and Exposure Indices
– Guidance (see Heat Stress)
Form
• Physical agents have their own history
and character with respect to
measurement and exposure
assessment
• There is an underlying similarity among
the physical agents that may be
introduced
Example Set
•
•
•
•
Radiofrequency / Microwave Radiation
Optical Radiation (IR, Visible and UV)
Vibration (Hand-Arm and Whole Body)
Noise
Energy Distribution
1000
Energy
100
10
1
0.1
0.01
0.001
0.01
0.1
1
Bands
10
100
1000
Energy Limits
Within Bands
1000000
Energy Limit
100000
10000
1000
Emin
100
10
1
0.001
0.01
0.1
1
Bands
10
100
1000
Limits by Band
Is the limit exceeded within one or more bands?
1000000
100000
Energy
10000
1000
100
10
1
0.1
0.01
0.001
PD
0.01
Exp Lmt
0.1
1
Bands
10
100
1000
Sensitivity Curve
Sensitivity = Energy Limit / Emin
1000
Sensitivity
100
10
1
0.1
0.001
0.01
0.1
1
Bands
10
100
1000
Hazard Function
Hazard Function = 1.0 / Sensitivity
Filter Multiplier
1
0.1
0.01
0.001
0.001
0.01
0.1
1
Bands
10
100
1000
Effective Exposure
Effective Exposure = Energy Distribution x Hazard Function
1000
100
Energy
10
1
0.1
0.01
ED
E-eff
0.001
0.0001
0.00001
0.001
0.01
0.1
1
Bands
10
100
1000
Total Energy
Multiplying
– Energy Limits by Band
– Hazard Function by Band
and Integrating (Summing)
Yields a Constant Value:
A Total Energy Limit
Limit by Total
Energy
Total Energy
– In One Band
– Under the Effective Energy Curve
Compared to
Total Energy Limit
In Summary
• TLVs®
– Limit Power (Ability to Dissipate)
– Limit Total Energy (Ability to Absorb)
• Limit by
– Band
– Total
Agents Under
Review
• Lasers
• Vibration
• Cold Stress
•
•
•
•
• Altitude
• Impulse Noise
• ELF H-Fields
HAL
Lifting
WMSDs
Wide-Band RF
Scheduled Break
Take a minute to stretch!
Biologically Derived Airborne
Contaminants:
Bioaerosols and TLVs
Kenneth F. Martinez, MSEE, CIH
Chair, ACGIH® Bioaerosols Committee
NIOSH
®
Where ?
Microorganisms
• Obligate parasites (must have a living host)
– viruses
– bacteria
– rickettsia
• Facultative saprophytes (will utilize dead
organic material)
– fungi
– bacteria
Size Ranges of
Microorganisms
1 µm
Fungal
Spore
Escherichia
coli
Rabies
Virus
Polio
Virus
Mechanisms for
Microbial Dispersal
Linear Distances
Microbiological
Concerns
• Infections
• Immunologic Reactions
• Toxic Effects
Infectious Disease
• Pathogenicity
• Virulence
• Relationship between virulence (V), numbers
of pathogens or dosage (D), and resistant
state of the host (RS)
V*D
Infectious Disease =
RS
• Colonization
• Invasiveness
Infectious Disease
Terminology
• Portal of entry
• Exposure vs. infection
• Clinical vs. subclinical or asymptomatic
infection
• Carrier state
• Opportunistic infection
• Human pathogen vs. virulence
• Immunosuppression
Infectious Disease
Pathways
•
•
•
•
•
Respiratory
Oral (via ingestion)
Contact
Penetration
Vectors (via insect bite)
Allergic Disease
• Allergic rhinitis
• Allergic asthma
• Allergic bronchopulmonary aspergillosis
• Extrinsic allergic alveolitis
(hypersensitivity pneumonitis)
U.S. Disease
Prevalence
Allergic
Rhinitis
Sinistitis
Asthma
Allergic
Dermititis
ABPA
HP
0%
10%
20%
Prevalence
Source: NHLBI, 1991
30%
• 1 of 5 Americans suffer
from allergic disease
• Indoor allergens
responsible for
significant share
• Environmental control
reduces disease
severity
Allergen Exposure
Dust Mites
Molds
Animal Dander
Pollen
Allergenic Chemicals
Genetic
Predisposition
Allergic
Disease
Immunologic
Sensitization
or
Susceptibility
Mild
Moderate
Severe
(Death)
Other Exposures
Viruses
Air Pollution
Tobacco Smoke
Source: Pope AM, et al., eds., 1993
Important Mycotoxins
Toxin
Fungal Species
Aspergillus
Aspergillus parasiticus
Aflatoxin
Aspergillus flavus
Aspergillus versicolor
Sterigmatocystin
Aspergillus terreus
Patulin
Citrinin
Fusarium
Fusarium moniliforme
Zearalenone
Fusarium spp.
Tricothecenes
Penicillium
Penicillium viridicatum
Ochratoxin
Penicillium spp.
Citrinin
Patulin
Stachybotrys
Stachybotrys chartarum (atra)
Tricothecenes
Where Are We?
In Transit
5%
Outdoors
2%
Indoors
93%
Classification of
Occupant Complaints
• Sick Building Syndrome
• Building-Related Disease
• Occupant Discomfort
Sick Building Syndrome
Non-specific Symptoms
•
•
•
•
•
•
•
•
Headache
Eye, nose, throat irritation
Sneezing
Fatigue and lethargy
Skin irritation
Dizziness and nausea
Cough
Chest tightness
Building-Related
Disease
• Known etiologies
• Related to identifiable exposure
Legionnaires Disease
Pontiac Fever
Humidifier Fever
Hypersensitivity Pneumonitis
Anthrax
Why Not Scientifically
Supportable?
Total Culturable or Countable
Bioaerosols
•
•
•
•
Not a single entity
Human responses cover wide range
No single sampling method exists
No exposure/response relationships
exist
Why Not Scientifically
Supportable?
Specific Culturable or Countable Bioaerosols
- other than infectious
• Data are derived from indicators rather
than actual effector agents
• Concentrations vary widely
• Low statistical power in cause-effect
relationship studies
Why Not Scientifically
Supportable?
Infectious Culturable or Countable
Bioaerosols
• Dose-response data limited to a few agents
• Air sampling limited to research
• Administrative and engineering controls
remain the primary defenses
Why Not Scientifically
Supportable?
Assayable biological contaminants
• Some dose-response relationship data
available
– Experimental studies
– Epidemiologic surveys
• Assay methods improving
• May be appropriate in the future
Questions?
•
•
•
•
•
Pat Breysse
Lisa Brosseau
Larry Lowry
Tom Bernard
Ken Martinez