ST210_UrinaryCatheterization
advertisement

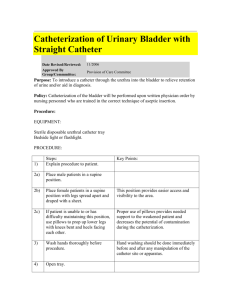
Surgical Technology Lecture Series 2000© Power-Point® Content Outline • • • • • • Laboratory Values of Urine Indications for Catheterization Catheterization Considerations Necessary Supplies Insertion Procedure Output Monitoring Quantity • Normal urine output per day – 1000 to 1500 ml – Approximately 95% is H2O – Output can vary greatly according to • • • • Intake of fluid Type and amount of food Exercise Kidney function Quantity (continued) • Abnormalities and indications – Polyuria: diabetes (mellitus or insipidus), nephritis, intake of diuretics such as caffeine – Oliguria: nephritis, heart disease, fever, diarrhea, vomiting, low fluid intake – Anuria: uremia, acute nephritis, complete obstruction of ureters or urethral opening from bladder Color • Normal: yellow to amber – Depends on concentration of the pigment urochrome • Abnormalities and indications – Milky or cloudy: pus or fat globules indicating a GU infection, bacterial sediment due to GU infection Color (continued) – Red: • Hematuria: urinary obstruction, renal calculi, tumor, renal failure • drugs or dyes used for x-ray purposes • food dyes – Pale: diabetes insipidus – Greenish-brown: bile pigment due to jaundice – Black: poisoning, hemorrhage Odor • Normal – Faintly sweet, but not too strong • Abnormalities and indications – Strong sweet smell: acetone present associated with diabetes mellitus – Unpleasant smell: ingestion of a drug or certain types of food Composition Proteinuria • Albumin and globulin – Normal: 10-100 mg excreted in the urine in each 24 hour period • Abnormalities and indications – Albumin: renal disease, diabetes mellitus – Globulin: renal disease, pyelonephritis Sugar • Normal –0 • Abnormalities and indications – Glycosuria: diabetes mellitus, high intake of sugar Ketones • Normal –0 • Abnormalities and indications – Ketonuria: diabetic ketoacidosis, starvation, eating disorders Red Blood Cells • Normal – 0-4 • Abnormalities and indications – Hematuria due to injury to kidney White Blood Cells • Normal – 0-5 • Abnormalities and indications – UTI Specific Gravity • Definition – Abbreviation sp gr – Weight of a substance as compared to the equal volume of water – Water is the standard and has a sp gr of 1 • Normal – 1.010 - 1.025 Specific Gravity (continued) • Abnormalities and indications – Low: dilution of urine, renal disease such as nephritis, pituitary disease is suspected due to decreased ADH – High: acute nephritis, diabetes mellitus if urine is light yellow in color pH • Review of pH scale – – – – Neutral: 7 Less than 7: acid More than 7: alkaline Maximum acidity (acidosis): 0 – Maximum alkalinity: 14 pH (continued) • Normal – 4.6 - 8.0 – average is 6.0 • Abnormalities and indications – High acidity: acidosis, diabetes mellitus, fever, starvation – Alkaline: vegetarian diet, infection, ingestion of alkaline compounds/products Indications for Catheterization • Specimen (typically done through clean catch) – A sterile specimen is needed for laboratory analysis • Decompression of bladder – Decompress bladder to avoid injury to the bladder during abdominal or pelvic surgery • Monitor output – Measure urine output pre-, intra-, and postoperatively Indications (continued) • Incontinence – Placed in surgical patient who has incontinence prior to surgical procedure – Placed in surgical patient who will possibly have temporary incontinence after surgical procedure – Placed in surgical patient who will possibly have permanent incontinence due to trauma Indications (continued) • Facilitate hemostasis – Large balloon on indwelling catheter compresses against bladder wall – Aids in hemostasis after a TURP or other surgery on GU tract structures • Facilitate output and healing – Facilitates output of urine after surgery on GU tract structures – Allows structures time to heal and regain strength Physician’s Order • Know the physician’s order • straight catheter vs. indwelling catheter • how long should catheter be left in place • size of catheter • type of catheter Know the Anatomy • Male anatomy – Due to length of urethra, it may curve on its path from the bladder to the urethral meatus • Curves may make catheter insertion difficult – Lift penis vertically and hold taught to straighten any curves when inserting catheter Know the Anatomy (continued) • Female anatomy – Urethra much shorter than male – Urethral meatus difficult to locate – Must retract labia to locate the urethra – Due to shorter urethra, females are more prone to contracting a UTI than a male Positioning • Male – Supine • Female – Frog-leg(modified recumbent) position – Place pillows under knees for support Note: Catheterization is accomplished before the patient is placed in the surgical position – Exception - lithotomy position Lighting • Recommended to have surgical lights turned on and in position before placement of catheter – Aids in visualization of urethra, especially the female Sterile Technique • Urinary catheterization is a sterile procedure • Strict sterile technique must be followed to prevent the patient from experiencing a UTI • Sterile gloves are worn • Sterile, disposable catheterization tray is used Size of Catheter • Review of French scale – Abbreviation Fr – System of measurement used to indicate the outer diameter of catheters, dilators, and sounds – Each unit of the Fr scale is equal to approximately 1/3 mm – Example: 21 Fr = 7 mm Size of Catheter (continued) • Adult – Female • Usually 14 Fr or 16 Fr – Male • Usually 16 Fr or 18 Fr • Pediatric – According to size of infant/child – Smallest size available is 8 Fr Types of Catheters • Robinson catheter – Also called red Robinson, red rob, or straight cath – Non-retaining – 1 or 2 holes at tip – May be lubricated (KY Jelly®) Types of Catheters (continued) • Foley catheter – Indwelling catheter • 5 ml or 30 ml balloon used to retain catheter in bladder – 5 ml used most frequently; 10 ml of sterile H20 required to inflate 5 ml balloon – 30 ml used postoperatively to aid in achieving bladder hemostasis Types of Catheters (continued) • Foley catheter (continued) – 2-way Foley • Lumen for filling and emptying the balloon • Lumen for drainage (outflow) – 3-way Foley • Lumen for filling and emptying the balloon • Lumen for drainage (outflow) • Lumen for irrigation (inflow) Foley Catheter Tray • Sterile Foley catheter kit may contain – Drapes – Gloves – Lubricant (K-Y Jelly®) may be in a small packet or syringe – Cotton balls or gauze – Forceps – Antiseptic solution (Betadine®) Foley Catheter Tray (continued) • Kit contents (continued) – Foley catheter – Drainage bag (may be pre-connected to catheter) – Sterile specimen cup with label – 10 cc syringe prefilled with water – Tape Coude Catheter • Non-retaining or ballooned style • Firm curved tip – Used when urethra is distorted (eg BPH) Insertion Procedure The following are the procedural steps for the placement of an indwelling catheter in a female • Wash hands • Position and expose patient • Provide illumination • Open catheter tray in a sterile manner – Tray may be placed between the patient’s legs Insertion Procedure (continued) • Don sterile gloves using the open glove technique • Organize supplies within sterile field – Attach syringe and inflate balloon with water to check the integrity of the balloon – Lubricate tip of catheter – Prepare antiseptic solution and applicators – Prepare specimen container (if needed) – Connect catheter to drainage bag (if needed) Insertion Procedure (continued) • Use nondominant hand to retract the labia • Cleanse meatus – Antiseptic soaked applicator is grasped with forceps in dominant hand – Meatus is cleaned in an anterior to posterior motion - applicator is discarded after use – Repeat x 2 Insertion Procedure (continued) • Insert catheter – Grasp lubricated catheter near tip – Insert catheter appropriate distance – Observe urine flow • May require application of external pressure Insertion Procedure (continued) • Inflate balloon – DO NOT INFLATE BALLOON UNTIL URINE FLOW IS CONFIRMED!!! • If balloon is inflated before urine flow is confirmed, it is possible that the catheter has not entered the bladder and the balloon may damage the urethra Insertion Procedure (continued) • Position catheter – Position catheter within bladder by gently retracting any redundant tubing – Position and secure the external tubing • Tape to inner aspect of patient’s thigh • Position drainage bag below the level of the bladder to facilitate drainage Insertion Procedure (continued) • Care for patient and supplies as needed – – – – – Dry patient Remove and discard unnecessary items Remove soiled gloves Reposition patient (if necessary) Care for specimen (if necessary) • Wash hands • Document procedure Insertion Procedure (continued) CAUTION • DO NOT raise the drainage bag above the level of the bladder – If drainage bag must be raised be sure to kink or clamp tubing to prevent retrograde flow of urine and prevent a UTI – Care must be taken when moving the patient to protect the catheter and drainage bag to avoid injury to the urethra and avoid retrograde flow Drainage Bag • Graduated in ml’s to estimate output – Empty urine from bag into graduated pitcher for more accurate measurement – Make sure all urine has passed from drainage tube into the bag prior to measurement Urometer® • Plastic container attached to bag – Graduated in ml’s – Allows for more accurate measurement than bag – Back of container has opening to allow excess urine to flow into the bag General Information • Urine collection unit is emptied as needed or just prior to transport to PACU • Amount of urine excreted during surgery is recorded prior to patient transported to PACU • Bag is again emptied and the amount recorded prior to transport from PACU