Simultaneous Liver and Colorectal Resections Are Safe for
advertisement

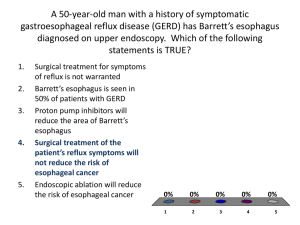
Barrett’s Esophagus SLR Grand Rounds May 30, 2007 Norman Barrett (1903-1979) Born in Australia Moved to UK in 1913 Nicknamed “Pasty” Spent most of career at St. Thomas Hospital in London Norman Barrett (1903-1979) 1950: defined the esophagus as lined by squamous epithelium. Proposed that columnarlined distal esophagus was actually a part of the stomach tethered to an shortened esophagus Norman Barrett (1903-1979) 1953: Allison and Johnstone proposed that the columnar epithelium was actually abnormal esophagus and called it “Barrett’s ulcers” 1957: Barrett finally agreed that it was esophagus and not stomach Barrett’s Esophagus Definition: Esophagus in which normal squamous epithelium changed to columnar epithelium – Intestinal epithelium: Goblet cells Most commonly arises in the setting of GERD – Most commonly found on screening EGDs done for GERD Epidemiology Incidence: – Need endoscopy for diagnosis – 20% of US population has reflux symptoms at least once per week – 10-15% of patients with GERD may have Barrett’s – Estimated that 25% of people with Barrett’s have no reflux symptoms Epidemiology Premalignant condition – Metaplasia to Dysplasia to Adenocarcinoma Presence of Barrett’s: 30-125 increase in risk of esophageal adenoca. – 0.5% chance per year of developing adenoca Incidence of esophageal adenoca has increased by 350% for white males in US over the past 30 years Genetics Multi-hit model from metaplasia to cancer – APC – DCC – BMP4 – p16 – p53 Normal GEJ Detection Endoscopy – Pink columnar epithelium in contrast to pale squamous Long segment – >3 cm from GEJ Short segment – <3cm from GEJ Histology Normal GEJ QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Histology Barrett’s Esophagus QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Guidelines American College of Gastroenterology PPI Intestinal Metaplasia without dysplasia – EGD every 3 years Low Grade Dysplasia – EGD every year until no dysplasia x2 then every 3 years High Grade Dysplasia – EGD every 3 months Guidelines Surgical Guidelines: not officially set Intestinal Metaplasia without dysplasia – Surveillance +/- anti-reflux surgery Low Grade Dysplasia – Surveillance +/- anti-reflux surgery High Grade Dysplasia – Esophagectomy Guidelines: Medical v. Surgical Pharmacologic v. Mechanical control of reflux Esophageal acidity can be corrected to normal levels (pH <4.0 for <5% of time) with varying doses of PPI for majority of patients (85%) Understanding the pathophysiology of reflux Biliary Reflux Bile salts refluxed into stomach and then into esophagus Rat models demonstrate esophageal exposure to duodenal contents leads to adenocarcinoma – Gastric acid inhibits formation of adenoca Biliary Reflux Bile salts deconjugated to bile acids in neutral pH and by bacteria - overgrown with reduced gastric acid – Unconjugated able to cause damage at pH 7 – Very few conjugated salts damaging at pH 2 Concentration v. Volume – Decreased acid production leads to decreased refluxed volume – Decreased acid production decreases the volume bile is diluted with Parrilla et al. Long-Term Results of a Randomized Prospective Study Comparing Medical and Surgical Treatment of Barrett’s Esophagus. Parrilla et al. Annals of Surgery. 2003. “There are no differences between the two types [medical v. surgical] of treatment in respect of preventing Barrett’s Esophagus from progressing to dysplasia and adenocarcinoma” Parrilla et al. High Grade Dysplasia Esophagectomy the gold standard Removes dysplastic regions and nodes with possible metastatic disease 5 year survival rates between 94-100% for dysplasia only – Drops to 80-85% when carcinoma found in surgical specimen Highly morbid – All comers, high volume centers: 5% mortality 50-60% peri-op complication rates Esophagectomy En Bloc: – Greatest chance of complete resection Transhiatal: – Good esophageal resection but limited nodal dissection Vagal-Sparing: – Patients end up with a highly selective vagotomy, reducing rates of dumping syndrome – Stripping of esophagus – No mediastinal dissection, minimal hiatal dissection Minimally Invasive Techniques Endoscopic Therapy for HG Dysplasia Ablation or resection of the mucosa +/submucosa in an effort to remove all disease For dysplasia only, not carcinoma Ablation or resection removes the columnar mucosa -> neosquamous overgrowth Danger of hidden columnar glands(0-70%) Endoscopic Therapy for HG Dysplasia All require multiple sessions per treatment – Usually 3-5 Combination with anti-reflux surgery Treatment before or after anti-reflux surgery? – RFA: orientation, correction of hiatal hernia Endoscopic Therapy for HG Dysplasia Photodynamic therapy (PDT) Laser Ablation Multipolar Electrocoagulation Argon Plasma Coagulation Endoscopic Mucosal Resection (EMR) Radiofrequency Ablation Photodynamic Therapy (PDT) Parenteral injection of porphyrin compunds Activation with endoscopic laser – Leads to oxygen free radicals -> cell death Porfimer sodium – – – – – – Downgrading of HGD to Barrett’s 90% Resolution of Barrett’s 40% Deep tissue penetration: 1cm Strictures 25-50% Needs 4-8 weeks of gradual exposure to light 13% rate of progression to carcinoma (no surgery) Photodynamic Therapy (PDT) ALA (aminolevulinic acid) – Downgrading of HGD to Barrett’s 100% – Resolution of Barrett’s 68% – Shallow tissue penetration - 2mm – No photosensitivity side effects – 6% rate of progression to carcinoma (no surgery) – No reported strictures Laser Ablation Argon, KTP, Nd:YAG lasers Availability sparse Most studies are small with n < 15 – Generally have a response rate of 80-100% – Complications of bleeding, pain, perforation, stricture Multipolar Electrocoagulation (MPEC) Electrocautery of Barrett’s Widely available One large study by Sampliner et al – 58 patients: 85% regression of Barrett’s metaplasia with 78% complete regression – No dysplastic lesions included – 43% morbidity rate: chest pain, odynophagia, bleeding nausea – 5% hidden gland rate Argon Plasma Coagulation (APC) Stream of argon gas that is ionized by electrocautery to ablate tissue Widely available Response rates vary with power used – 70% with 30W to 100% with 90W Return of Barrett’s in as high as 60% with low wattage protocols High power protocols carry morbidity rates of 4060% and stricture rates of 10% Hidden glands occurred at rate of 25-50% Radiofrequency Ablation HALO360 from BARRX Balloon dilatation of esophagus for uniform depth Circumferential ablation at depth of 1mm – Depth of Barrett’s ~500nm – Muscularis Mucosa ~1mm from surface Shallow penetration allows circumferential ablation without stricture Radiofrequency Ablation AIM I and II trials multi-center AIM II- 1st year results – – – – – 70 patients with metaplasia only 70% complete regression 25% partial regression 5% no regression No hidden glands in 3000 biopsy samples over first year of f/u – 23% had transient adverse events, mostly pain Endoscopic Mucosal Resection (EMR) Mimics surgical resection in that mucosa is removed and not ablated – Allows pathological analysis and improved staging Goal is not to remove all of Barrett’s regions Goal to remove suspicious lesions within Barrett’s areas – Chance of adenoca in otherwise non-descript Barrett’s region “rare” Remove focal adenoca while Barrett’s metaplasia controlled with ant-acid therapy Endoscopic Mucosal Resection (EMR) Saline injected into submucosa dissects it off lamina propria Tissue sucked into endoscopic cap Snare cautery excises the tissue Up to 1.5-2.0 cm sections can be removed Multiple specimens can be taken per session Extensive resection can lead to stricture Endoscopic Mucosal Resection (EMR) Endoscopic Mucosal Resection (EMR) Endoscopic Mucosal Resection (EMR) Endoscopic Mucosal Resection (EMR) Endoscopic Mucosal Resection (EMR) EMR as sole treatment for dysplasia 100 patients: 99% complete regression of dysplasia – Required multiple sessions (1-5, mean 1.5) – 11 patients developed metachronous lesions: all treated with resection PPI therapy to control acid reflux Total resection of Barrett’s EMR for Staging Stage 0 (in situ) v. Stage 1 (into but not through lamina propria) Invasion of muscularis mucosa important predictor of nodal mets – 4% if mucosa only – 30% if invasion into submucosa EUS good at determining invasion through submucosa and evaluating mediastinal nodes EMR of suspected lesions to determine invasion into submucosa – Directs esophagectomy method e.g. Vagal-Sparing EMR for Staging Plus Ablation EMR of suspected lesions to determine presence of adenoca No adenoca -> Complete RFA of Barrett’s Anti-reflux surgery to further increase chance of regression of abnormal tissue References Chandrasoma P. Controversies of the cardiac mucosa and Barrett's oesophagus.Histopathology. 2005 Apr;46(4):361-73. DeMeester SR. Adenocarcinoma of the esophagus and cardia: a review of the disease and its treatment.Ann Surg Oncol. 2006 Jan;13(1):12-30. DeMeester SR. EMR for intramucosal adenocarcinoma of the esophagus: does one size fit all?Gastrointest Endosc. 2007 Jan;65(1):14-5. Eickhoff,ハA.; Jakobs,ハR.; Weickert,ハU.; Hartmann,ハD.; Schilling,ハD.; Alsenbesy,ハM.; Eickhoff,ハJ. C.; Riemann,ハJ. F.Long-Segment early squamous cell carcinoma of the proximal esophagus: curative treatment and long-term follow-up after 5-aminolevulinic acid (5-ALA)-photodynamic therapy. Endoscopy. 2006 Jun;38(6):641-3. Ell C, May A, Pech O, Gossner L, Guenter E, Behrens A, Nachbar L, Huijsmans J, Vieth M, Stolte M. Curative endoscopic resection of early esophageal adenocarcinomas (Barrett's cancer).Gastrointest Endosc. 2007 Jan;65(1):3-10. Gerson LB, Shetler K, Triadafilopoulos G. Prevalence of Barrett's esophagus in asymptomatic individuals. Gastroenterology 2002;123:461-7. Kanne JP, Rohrmann CA, Lichtenstein JE. Eponyms in Radiology of the Digestive Tract: Historical Perspectives and Imaging AppearancesPart I. Pharynx, Esophagus, Stomach, and Intestine. RadioGraphics 2006;26:129-142 Liebwin Gossner, Manfred Stolte, Ronald Sroka, Kai Rick, Andrea May, Eckhard Gerhard Hahn and Christian Ell. Photodynamic ablation of high-grade dysplasia and early cancer in Barrett's esophagus by means of 5-aminolevulinic acid. Gastroenterology 1998; 114:448-455. Manner H, May A, Miehlke S, Dertinger S, Widdinghaus B, Schimming W, Kramer W, Niemann G, Stolte M, Ell C. Ablation of nonneoplastic Barrett's mucosa using argon plasma coagulation with concomitant esomeprazole therapy (APBANEX): a prospective multicenter evaluation.Am J Gastroenterol. 2006 Aug;101(8):1762-9. Oh DS, Hagen JA, Chandrasoma PT, Dunst CM, Demeester SR, Alavi M, Bremner CG, Lipham J, Rizzetto C, Cote R, Demeester TR. Clinical biology and surgical therapy of intramucosal adenocarcinoma of the esophagus.J Am Coll Surg. 2006 Aug;203(2):152-61. Overholt BF.Photodynamic therapy strictures: who is at risk?Gastrointest Endosc. 2007 Jan;65(1):67-9. Parrilla P, Martinez de Haro LF, Ortiz A, Munitiz V, Molina J, Bermejo J, Canteras M. Long-term results of a randomized prospective study comparing medical and surgical treatment of Barrett's esophagus.Ann Surg. 2003 Mar;237(3):291-8. Portale G, Hagen JA, Peters JH, Chan LS, DeMeester SR, Gandamihardja TA, DeMeester TR. Modern 5-year survival of resectable esophageal adenocarcinoma: single institution experience with 263 patients.J Am Coll Surg. 2006 Apr;202(4):58896. Prasad GA, Wang KK, Buttar NS, Wongkeesong LM, Lutzke LS, Borkenhagen LS. Predictors of stricture formation after photodynamic therapy for high-grade dysplasia in Barrett's esophagus.Gastrointest Endosc. 2007 Jan;65(1):60-6. Rastogi A, Sharma P. Barrett's esophagus.Endoscopy. 2006 Nov;38(11):1065-9. Rossi M, Barreca M, de Bortoli N, Renzi C, Santi S, Gennai A, Bellini M, Costa F, Conio M, Marchi S. Efficacy of Nissen fundoplication versus medical therapy in the regression of low-grade dysplasia in patients with Barrett esophagus: a prospective study.Ann Surg. 2006 Jan;243(1):58-63. Sampliner RE, Faigel D, Fennerty MB, Lieberman D, Ippoliti A, Lewin K, Weinstein WM. Effective and safe endoscopic reversal of nondysplastic Barrett's esophagus with thermal electrocoagulation combined with high-dose acid inhibition: a multicenter study.Gastrointest Endosc. 2001 May;53(6):554-8. Sampliner RE. Updated guidelines for the diagnosis, surveillance, and therapy of Barrett’s esophagus. Am J Gastroenterol. 2002 Aug;97(8):1888-95. Schuchert MJ, Luketich JD. Barrett's esophagus-emerging concepts and controversies.J Surg Oncol. 2007 Mar 1;95(3):185-9. ShalautaMD , Saad R. Barrett's Esophagus. Am Fam Physician 2004;69: 21138,2120. Sharma VK, Wang KK, Overholt BF, Lightdale CJ, Fennerty MB, Dean PJ, Pleskow DK, Chuttani R, Reymunde A, Santiago N, Chang KJ, Kimmey MB, Fleischer DE. Balloon-based, circumferential, endoscopic radiofrequency ablation of Barrett's esophagus: 1-year follow-up of 100 patients.Gastrointest Endosc. 2007 Feb;65(2):185-95. Sharma P, Jaffe PE, Bhattacharyya A, Sampliner RE. Laser and multipolar electrocoagulation ablation of early Barrett's adenocarcinoma: long-term follow-up. Gastrointest Endosc. 1999 Jan;49(4):442-446. Spechler SJ, Sharma P, Traxler B, Levine D, Falk GW. Gastric and esophageal pH in patients with Barrett's esophagus treated with three esomeprazole dosages: a randomized, double-blind, crossover trial.Am J Gastroenterol. 2006 Sep;101(9):1964-71. Todd JA, Basu KK, de Caestecker JS. Normalization of oesophageal pH does not guarantee control of duodenogastro-oesophageal reflux in Barrett's oesophagus.Aliment Pharmacol Ther. 2005 Apr 15;21(8):969-75. Wang KK, Sampliner RE. Mucosal ablation therapy of barrett esophagus. Mayo Clin Proc. 2001 Apr; 76(4):433-7.
![EOSINOPHILIC ESOPHAGITIS [EE]](http://s3.studylib.net/store/data/009399872_1-fb87975e549aa57f606b438a42821700-300x300.png)
