What is Pain?
advertisement

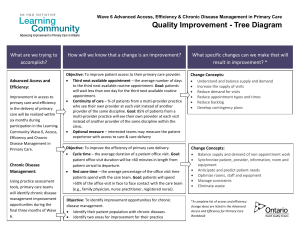
Chronic Pain Module MOA Breakout Adapted from Barb Aasen, David Jermey, and Josefa Kontogiannis, www.pspbc.ca Let’s recap what we heard today Definition of pain People in Pain Consequences of pain Other problems brought on by pain Types of pain What can MOAs do to help these patients when they come in for their appointments every 43,180 minutes? 2 Today we heard the definition of Pain Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage. - International Association for the Study of Pain(1979) A warning sign A potential lead to red flags It is costly if not caught, to the patient and to the system An experience created in our brain that is influenced by things other than tissue damage An experience not dependent on tissue damage 3 People in Pain ??!! There may be some patients that you have been thinking about today Diverse Population: › Chronic Disease eg Cardiac disease, Diabetes, Osteoarthritis › Chronic Post Surgical Pain › Chronic Pain Post Injury eg Whiplash, Spinal Cord Injury › Chronic Headaches eg Tension, Migraine, Cluster. › Neuropathic Pain eg Post Herpetic Neuralgia, Diabetic Neuropathy › Complex Regional pain Syndrome › Recurrent Abdominal pain / Visceral Pain › Fibromyalgia › Back Pain › Post trauma/burns/stroke › Cancer 4 Consequences This is what some of them are experiencing due to pain Person with pain: › Lowest Quality of Life scores of any chronic disease › Depression and anxiety (5X) › Suicide (2X) › Sleep disorder › Addiction/Substance abuse co-morbidity freedigitalimages.net › Job loss and financial stress 5 Consequences These are what they are now calling norms in their life Direct Healthcare Consumption • 4x GP visits • 2x hospital admissions and length of stay • Use Emergency for treatment (esp. no GP or marginalized) • Increased drug costs and surgeries/procedures Indirect Societal Costs • Lost productivity • Lost tax revenue • Increased benefit payments • Social issues: prescription diversion, homelessness, poverty 6 20 minutes a month with my healthcare provider leaves43,180 minutes before my next appointment So, the rest is down to me! What’s going on during the 43,180 minutes before they see you again? Hopelessness Stigma Mistrust Knowledge gap Lack of accountability Resource strain 8 Basic Science of Persistent Pain Vicious cycles develop between pain and its effects › Pain - shallow, tight, apical breathing - pain › Pain - altered body awareness - pain › Pain - muscle inhibition - pain › Pain - muscle tension - pain › Pain - altered body image - pain › Pain - anxiety - pain 9 MOA Role in Support for Patients with Chronic Pain Understanding the severity range of Chronic pain Being aware of what is needed for an appointment ie: › Time required › Tools needed › Follow up appointments/specialist appointments A good awareness of the screening tools, when they are used and needed Billing required Opioid management Diffusing difficult conversations Urine testing 10 Understanding Range and Severity People in pain may be….. Needing assistance Accompanied by someone Not feeling like engaging in conversation Slow moving Needing more time Unpleasant 11 Being aware of what is needed for an appointment Discuss with the doctor about the appointment logistics The length of the appointment/ how often this patient should be seen The screening tools/lab reqs required and who is to give them out Use the closest exam room if possible, less walking Whether this patient should come earlier for any prep or filling out of forms Empathy 12 A good awareness of the screening tools What they are used for When they are given Who gives them 13 Structured assessments Can be handed out by MOA Can be completed by patient prior to doctor-patient encounter Can be repeated each visit to assess progress Structured Assessments Pain diagrams Disability assessment tools Opioid Management/Urine testing When the patient comes in for a pain appointment, a random urine drug screen (RUDS) may be done to verify what drugs the patient is taking. Some physicians like this to be a witnessed collection at the clinic. There can be a narcotic contract between the physician and patient so that the agreement is clear on both sides of what is expected as far as compliance, early release etc. The physician can access PharmaNet to see what prescriptions the patient has had filled recently. 16 Tools Managing Pain Pain Diagram Name: ____________________________________________ Date: _____________________________ Please colour the areas where you experience pain. Use one of the five colouring pens to shade the specific type of pain that you are experiencing. Then circle with a pen all the areas of pain and starting with the worst, number the areas in order of severity. Red - Burning Green - Tingling Blue - Numbness If you have other pain sensations name them here and colour as yellow or black Yellow Black - It is the intention of the PSP that health educators and health providers only use this publication and its content for non- 17 Diffusing difficult conversations Communication is not just saying words; it is creating true understanding. Active listening is an important skill in the communication process “Listen Non-judgementally” 20 Tips to be a better Active Listener Don’t interrupt Silence is a powerful listening skill. Be quiet & give the person time to think, as well as talk Let the person finish what they are saying It’s not possible to talk & listen at the same time 21 Keep an open mind Listen, don’t judge. Jumping to conclusions & looking for the right or wrong in what is being said can prevent you from listening Think before you respond 22 Make listening a priority Stay focused on what is being said – don’t let your mind wander Stay in the present. Try not to think ahead of what you are going to say Let go of your agenda & listen & focus on theirs Show respect for the person & their feelings Show respect even if you disagree with what is being said 23 Avoid giving advice, even when asked Offer options & suggestions rather than advice. Give people the opportunity to discover their own best answer. Learn the art of asking good questions Open ended questions. These questions encourage people to go into more depth about the situation Closed ended questions. People usually answer these questions with short “yes/no” type responses 24 Listen with empathy This shows that you are trying to understand their situation. By paraphrasing, you show concern, interest & empathy. “ So you feel _____because_____” Let the person know you are listening with minimal prompts like “uh –huh” or “I see” 25 Watch non-verbal behaviour Pay attention to your non-verbal signals, as well as the other person’s Keep an open body posture to show you care & are listening Try to maintain eye contact 26