First 3 Weeks of Readings For Nursing III Fall 2013 These readings
advertisement

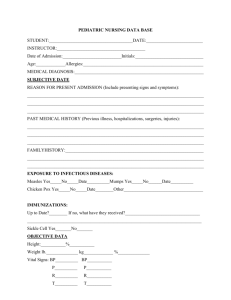
First 3 Weeks of Readings For Nursing III Fall 2013 These readings have been chosen to give you an overview of the scope and practice of caring for the growing family. NOTE: The Critical Concept review at the end of each chapter. INTRODUCTION - THE FAMILY: INTIMACY VS. ISOLATION (1/16) Week one. Readings: London Introduction to Maternity Nursing: Chapters 1; 2; 3; 5 (pgs. 104-105), chapter 10 (pgs. 200-213) * The understanding of key prenatal and labor and delivery concepts are necessary in order to facilitate postpartal family care. I. Baseline Data a. Definitions of terms 1) Antepartal 2) Intrapartal 3) Postpartal 4) Gravida 5) Parity 6) Gestation 7) Term b. Anatomy and Physiology (overview) 1) Internal and external reproductive organs a. breasts and nipples b. uterus c. perineum d. rectum II. Nursing process a. Assessment data 1) Client history/profile Maslow hierarchy of needs Risk assessment 2) Physical assessment 3) Pertinent prenatal lab tests and data 4) Determination of length of gestation 5) Labor data 6) Method of delivery Analgesia Anesthesia b. Data Analysis: Common Nursing diagnoses 1) Actual 2) Risk 3) Wellness c. Expected outcome statement for family d. Interventions with rationales 1) Evidence-based standards e. Evaluation -19- OUTLINE FOR INTRODUCTION TO THE CARE OF THE GROWING FAMILY: I. Baseline data A. Current issues in maternal-newborn care B. Statistics related to families/mortality and morbidity C. Social and cultural issues II. Nursing process A. Assessment: data collection - needs assessment associated with the following: 1. Social, cultural and religious influence on the child 2. Family structure 3. Major trends in growth and development 4. Communication with children 5. Overview of current perspectives in maternal-newborn nursing: a. Nursing roles and standards of care b. Legal and ethical aspects c. Biomedical technology B. Data analysis: 1. Ineffective coping R/T role change 2. Altered family processes R/T birth of newborn 3. Altered role performance R/T change in roles C. Expected outcomes D. Nursing interventions and rationale E. Evaluation THE POSTPARTAL FAMILY: NEEDS OF THE NEWBORN (1/16) Week one. Readings: London Chapters 24; 25; 26; 27; 34 (pgs. 895-901) Refer to appropriate drug classifications relative to this area. OUTLINE I. Baseline data A. Normal growth and development 1. Biologic 2. Psychosocial 3. Cognitive B. Physiological response to birth C. Psychosocial and cultural factors D. Terminology -20II. Nursing process A. Assessment: data collection 1. Diagnostic tests 2. Laboratory data 3. Needs assessment of the normal newborn: a. Apgar score b. Gestational age assessment c. Physiological adaptations (1) Vitamin K (2) Eye care (3) Cord care (4) Physiologic jaundice d. Neurological status e. Behavioral patterns f. Oxygenation g. Temperature control h. Sleep i. Nutrition j. Prevention of infection k. Newborn screening (PKU) l. Allergic response (1) Diaper rash (2) Cradle cap m. Parent education (1) Handling (2) Bathing (3) Wrapping (4) Dressing (5) Feeding (breast and bottle) (6) Elimination (7) Circumcision (8) Safety (9) Vaccines (10)When to call pediatrician (11)Cord care n. Maternal-infant interaction B. Data analysis: common nursing diagnoses 1. Ineffective airway clearance R/T mucus obstruction 2. Ineffective thermoregulation R/T hypothermia secondary to inadequate subcutaneous tissue 3. Risk for alteration in tissue perfusion R/T decreased body temperature 4. Ineffective feeding pattern R/T poor sucking reflex 5. Ineffective family coping R/T birth of potentially ill newborn C. Expected outcomes D. Nursing interventions and rationale E. Evaluation -21THE POSTPARTAL FAMILY: NEEDS OF THE POSTPARTAL CLIENT (1/16) week 1 Readings: London Chapters 22 (pgs. 518-522); 30; 31 Refer to appropriate drug classifications relative to this area. I. OUTLINE Baseline data A. Physiology (review) B. Psychosocial and cultural factors C. Terminology D. Risk factors II. Nursing process A. Assessment: data collection 1. Diagnostic tests 2. Laboratory data 3. Needs assessment of a postpartal client: a. Physiological needs (1) Oxygen (2) Fluids and electrolytes (3) Nutrition (4) Elimination (5) Activity and exercise (6) Comfort (NOTE: Drug Guide - Postpartum Epidural Morphine, p. 607) (7) Vaginal vs. Cesarean delivery b. Safety and security needs (1) Discharge teaching - self care, danger signs (2) Discharge teaching – parenting c. Love and belonging needs (1) Parent-infant bonding (2) Resumption of sexual activities/contraception (3) Role integration d. Self-esteem needs (1) Family wellness (2) Postpartum "blues" -22B. Data analysis: common nursing diagnoses 1. Self care deficit R/T knowledge deficit secondary to normal psychological changes in postpartal period 2. Altered comfort R/T to episiotomy, sore nipples, breast engorgement, hemorrhoids 3. Anxiety R/T change in role function C. Expected outcomes D. Nursing interventions and rationale E. Evaluation POSTPARTAL FAMILY AT RISK NEEDS OF THE POSTPARTAL CLIENT AT RISK week 2 Readings: London Chapter 23 (pgs. 521-527); 32 Vacarolis Chapter 18 (1/23) Refer to appropriate drug classifications relative to this area. OUTLINE I. Baseline data A. Physiology (review) B. Psychosocial and cultural factors C. Terminology D. Risk factors II. Nursing process A. Assessment: data collection 1. Diagnostic tests 2. Laboratory data 3. Needs assessment of a client with postpartal complications: a. Alterations in oxygenation (1) Hemorrhage (a) Uterine atony (b) Retained placenta (c) Hematomas/lacerations (d) Subinvolution (2) Thrombus formation b. Alterations in safety (1) Postpartum infections (2) Mastitis/Endometritis (3) Substance abuse (4) Postpartum depression (5) Postpartum psychosis B. Data analysis: common nursing diagnoses 1. Altered peripheral tissue perfusion R/T interrupted venous flow 2. Fluid volume deficit R/T excessive bleeding 3. High risk for infection R/T tissue trauma 4. Risk for altered parent-infant attachment R/T hormonal imbalances -23C. Expected outcomes D. Nursing interventions and rationale E. Evaluation THE POSTPARTAL FAMILY AT RISK NEEDS OF THE NEWBORN AT RISK (1/30) week 3 Readings: London Chapters 28; 29; 47 (pgs. 1278-1281) HIV: Vertical Transmission (p. 698) Refer to appropriate drug classifications relative to this area. OUTLINE I. Baseline data A. B. C. D. Physiology (review) Psychosocial and cultural factors Terminology Risk factors II. Nursing process A. Assessment: data collection 1. Diagnostic tests 2. Laboratory data 3. Needs assessment of the high risk newborn: a. b. c. d. e. f. g. h. Abnormal gestational age or size Nutrition Infant of a diabetic mother Respiratory distress syndrome, retinopathy of prematurity (ROP) Cold stress Hypoglycemia Hypocalcemia Jaundice/kernicterus/hemolytic dysfunction/RH sensitization i. Neonatal infections (1) Sepsis (2) TORCH infections j. Necrotizing enterocolitis. k. Newborn resuscitation l. Cardiac defects m. HIV in infants n. chemical dependence -24B. Data analysis: common nursing diagnoses 1. Impaired gas exchange R/T respiratory distress secondary to surfactant deficiency 2. Risk for alteration in nutrition, less than body requirements R/T limited intake 3. High risk for injury to CNS involvement R/T electrolyte imbalance C. Expected outcomes D. Nursing interventions and rationale E. Evaluation