When policy says something like: For J0588, except under off
advertisement

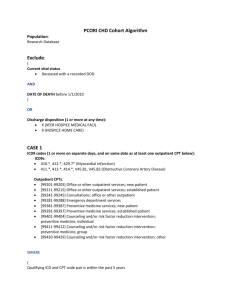
When policy says something like:
For J0588, except under off-label use circumstances outlined in Indications and Limitations
above, only ICD-9-CM codes 333.81 and 333.83 support medical necessity. (Make note in Note
box: J0588 only 333.81 and 333.83 support medical necessity. And remember to only include the
ICD’s under this CPT.)
The following CPT codes are not restricted by the ICD-9-CM codes listed in this policy: 31513,
31570, 31599, 43499, 53899 and 64640 or if it says: Diagnostic criteria do not apply to the
following CPT codes (Add CPTs to DB with ICD flag set at 0 and add in More Info box: See Policy
Documentation for information regarding this CPT Code.)
Under ICDs 378.71* Use for medial rectus weakness only and 478.79* Use only for
Dysphonia spastic. (Make note in Note Box: excluded ICD # – used in limited
situations. Key word is Only)
CPT code 98943, CMT, extraspinal, one or more regions, is not a Medicare benefit. (Add CPT
with a deny 3)
Under Utilization Guidelines (bottom of policy) CPT codes will be limited to once per
lifetime (Add Frequency 1/1/L with More Info Box: CPT Code will be limited to once
per lifetime.)
When policy is a split policy:
Usually, we split a policy because there are age restrictions for certain conditions. If it’s an IVIG policy,
for example, AIDS treatment is covered for children under 13, bone marrow transplant for people under
20, etc. (I might be wrong on those – but hopefully you get the idea!). So we split the policy so we can
enter the age restriction on the main policy tab. Then only the CPTs/ICDs that have that age restriction
are included in that version of the policy on Utility. The CPTs/ICDs that don’t have age restrictions will all
be in the general policy.
So, continuing with the IVIG example, we would have a general policy, an HIV policy (with only
the 042 ICD code any any CPTs that it applies to), a BMT policy (with only the BMT ICD (I forget
what it is) and any CPTs that it applies to), and then I think there’s sometimes one other one
(again, just with the applicable ICDs/CPTs). So you have to check all of them, but the general
policy will have the majority of the codes.
If you spend a few minutes reading over the policy you’ll notice the age restrictions, then you should be
able to match that up to how we have it setup in Utility.
When multiple revisions:
On the spreadsheet, enter ‘multiple’ under as the effective date, then copy both revisions into the
‘blurb’ column. As far as the doc, that can be dated with the current date.
If I were you, I would do the update in two steps - first pull up the policy effective dated 10/1/11
and do that update (per the note at the top of the policy, do not add 77425 or 77426), then do the
1/23/12 update. That way you’ll be sure you know what is effective with each update.
How to change a start date
If you accidentally save the CPT with the wrong start date, just go over to the CPTs tab in Utility,
select that CPT and click on ‘start date’ down at the bottom. You’ll get a warning about how the
request is weird or something, but you can just okay that and then enter the correct start date in
the little box that pops up. It will then change the CPT start date to whatever you entered.
If you saved the ICDs with the wrong date, you can then follow the same process to update them
in the Rules tab.
You can do the same thing with expiration dates – just always make sure to change the date for
the CPTs and the ICDs (Rules).
If you accidentally expire something, you can undo that, too. Just select the CPT (or ICD(s)) and
click on End Date. When the little box comes up, type ‘null’ and hit enter and it should delete the
expiration date you entered.
How to delete/change a primary/secondary codes entered in error
The only way to delete a secondary that was added in error is to delete the whole entry (primary
and secondary) and then re-add the primary by itself. It’s actually one of the harder things to
correct! If there’s just one and you’re comfortable doing it yourself, you just need to make a note
(to yourself) on the effective date, then delete it through the Rules tab, then just add it back
through the normal process on the ‘text to ICD’ tab.
No, you can delete from Rules tab. The secret password is "secret" - clever, no?
Example of added FR for CPT’s
Freq = number of times; FreqSpan = per, FreqUnit = Day/Month/etc
I added FR for the CPT. Not sure if right. - No, you entered 1/12/W which means 1 per every 12
weeks. The policy allows "weekly sessions for 12 weeks" so that would be 12/12/W or 12 per 12
weeks.
Administered up to 3 times per cord at approximately 4-week intervals should be entered as the
FR 3/c/w
Would only be deny flag = 3 if they are always denied. If they are not always denied then just
make the ICD flag = 0 and leave the deny flag alone.
Also, when a CPT changes from covered to non-covered, we can't just change the deny flag and
ICD code. It has to be expired as covered and then re-added (effective the following day) as
denied. In this case, however, as you noticed, they still list ICDs for 92582 (and they're not
screening), so we can leave it in as covered. The two CPTs that have ICD 0 and MoreInfo
instead of a deny 3 are setup that way because they aren't allowed for audiologists, but appear to
be allowed for physicians, so we didn't want to flat out deny them. Also, we updated 92579 from
deny 3 to ICD 0 because it appears as both covered and non-covered (for screening).
3 MEANS ALWAYS DENIED, 4 MEANS SPECIAL RESTRICTION. 4 IS FOR CPTS THAT ARE
LISTED IN THE POLICY BUT DO NOT HAVE ICDS THAT ARE ATTACHED TO THOSE CPTS.
For the most part, you should add the new CPTs with deny 3 because they are considered not
reasonable and necessary. The exceptions, which you would add with ICD 0 and MoreInfo, are
unlisted CPTs (like 53899 and 99199) and CPTs that aren’t always denied. The latter is the case
with 0256T-0259T. The policy says “Investigative Device Exemptions (IDEs) involving
codes 0256T-0259T must follow the usual procedures of the Contractor for IDEs.
When these procedures are provided outside the IDE setting, documentation must be
submitted for individual consideration. 0256T-0259T will be considered reasonable
and necessary if the services are provided in the context of an IDE.” So, those four
codes would have ICD 0 and MoreInfo (use the statement above for MoreInfo). Just
glancing through the list, the rest should be okay with a deny 3.
Deny flag = 3 is for when the policy specifies that the procedure is never covered /
always denied. Utility will automatically set the ICD flag to 0 when you set the deny flag
to 3 because if the procedure is never covered / always denied then it wouldn’t have any
ICDs to support it.
Once every six months = 1/6/M
ICD flag = 0 is for when a procedure is mentioned or listed in a policy but we don’t know
what ICDs support it because they don’t tell us in the policy.
We use the except flag to indicate that the ICDs we added to Utility DO NOT support
medical necessity - everything except the ICDs entered will pass. It doesn't come up too
often.
ICD flag = 1 --> We are adding ICDs for this CPT
Except flag = 1 --> The ICDs we are adding DO NOT support medical necessity
If revision specifies a change in FR, you only need to change the numbers (No need to
expire CPT and reenter with new FR). Per CMD, there’s a little flaw in Utility that FRs are
not tied to a date, so expiring and re-adding the CPT would not have made a difference. In fact,
it probably would have caused a problem because we would have two different FRs associated
with the same CPT.
Adding CPT’s with ‘99
Create the article/policy and add the CPT, but we wouldn’t add the ICDs since it’s an unlisted
code. Just go with ICD “0” and MoreInfo like you would in other policies.
J3490 is an unclassified code (as is J3590 and I believe there are a few others). It’s a general
code that they use when a specific CPT code has not been designated for a drug. We treat them
just like the other unlisted codes that end in 99 and that’s why Stephanie added it with ICD 0
rather than deny 3.
Attaching PDFs when creating docs
Just wanted to share a tip that might come in handy when you create docs. Sometimes,
contractors create PDFs and attach them to policies (as coding or billing guidelines, for
example). As I’m sure you’ve noticed, it can be a pain in the butt to copy them into Word when
you’re creating a new doc. For whatever reason, they don’t like to copy and paste nicely.
Stephanie clued me in to this little tip awhile back and we thought we should share it with you!
The great thing about this tip is that you don’t actually have to copy the PDF! Hurray! Instead,
create the doc without the PDF attachment (if you have other things that should be included that
aren’t PDFs, you should copy them in as usual). “Print” the doc as usual. Then, go to the PDF
attachment that you needed to include with the doc. “Print” that file and enter the same doc name
that you used for the policy. In Bullzip, the first option under the field for the name is “Append if
output exists” – check that box! Then Bullzip will create a new doc for you – the policy will be
first, followed by the attachment – all in one handy doc just like you need it. This works great for
coding or billing guideline docs that don’t have any of the header information that we have to
delete. If you have a PDF that does have stuff to be deleted, you’ll have to struggle through
copying it over just like you always have.
Unlisted Codes
If adding new policy/article and it has unlisted CPT/ICD codes, we should add with ICD flag at 0
and add generic More Info
"E" codes and codes like “A4220” or codes that end with “KD” - Those are like the "unlisted"
codes and should be added with ICD flag = 0. We only don't add E codes that are ICDs.
Linked Policies
If different policy/article number, you must create different doc for each link.
Please leave any bone mass or PET scan articles or policies for Stephanie.
OPPS vs NON OPPS
They are different types of facilities. We have a deny flag to indicate that a code is non-covered
for OPPS (1) only or for NON OPPS (2) only. Example: “LCD revised to clarify that 77261, 77262,
77263, 77427, and 77431 are not recognized for payment by OPPS” Highlight the code then
click on the “Deny” button as usual to see the options. We usually use “3” because that is
always denied but “1” would mean denied for OPPS only. We would still need ICDs attached
because those CPTs are covered for NON-OPPS.
Effective Dates
Generally speaking, in the absence of a specific effective date, we will use the effective date in the
header of the version of the policy in which we see the change.
I really can't remember if we've ever gone over this before, but if you see something like this:
Explanation of Revision: Added diagnosis codes V67.00 and V67.09 for CPT codes 93975 and
93976 to be consistent with Part B Duplex Scanning LCD. The effective date of this revision is for
claims processed on or after 04/16/2013 for dates of service on or Revision History Number: R3
after 07/26/04.
then we would use 7/26/04 for the effective date of the new ICDs, not 4/16/2013. We don't
really care what date a claim was processed. It's the date of service that is important.
It doesn’t hurt to enter them now. So if you have time, go ahead. The rule is that if it’s more than a
month out and we have a busy deadline, then it can be kicked to the next week so that we can get all of
the other updates entered on time.
When change is effective back to original effective date, should delete ICDs and change ICD flag to 0.
Add-On Procedure Codes
If policy says “Add-on codes and must be billed”:
Create split policy {Main policy (A), Split policy (B)}
Add “add-on” CPT with ICD’s to Split policy (B)
Type in “Associated Procedure Codes” box any add-on CPTs
The Split Policy (B) must always be updated when working on Main Policy (A).
It is not clearly spelled out in the policy that 78496 can only be used as an add-on to certain specific
CPTs. In my experience, we have only done splits where the language has very clearly stated something
like “Add-on CPT code 78496 may only be submitted with 78472”.
Leaving out ICDs
If policy says something like “Claims listing 784.0 (headache) as the only diagnosis justifying a CCT scan should
include additional justification for the scan in the remarks section of the claim (Form Locator 80). Records received without
additional justification may be selected for review”.
Should be left out b/c “it needs additional justification”.
Should make note in Note Box.
Wasn't sure if I should've added the new ICD V58.65 b/c note says "is a secondary diagnosis code and
should not be billed as the primary diagnosis" and Policy L28934 had the same note with ICD V58.69 and
it was not added to DB. I hope i was correct in not adding it. Although I feel it prob should be added as a
secondary diagnosis but not 100% sure. Added note in Note Box. ~ You were right not to add it since
they don't specify that it is required as a secondary. Because they don't say 'xxx.xx must be submitted
with V58.69', we believe the other ICDs can pass on their own. What we can do is add the note to
MoreInfo, which I did.
Did not add A4220 and "E" codes nor did I add codes that end with "KD". Those are like the "unlisted"
codes. I added them with ICD flag = 0. Wasn’t sure about those. - we only don't add E codes that are
ICDs. I added these. All of the ICDs apply to the E codes here.
Leaving out CPTs
The last paragraph under Coverage/Limitation... says: "Also, it is not necessary to use Troponin in
addition to Creatine Kinase (procedure codes 82550-82554) in the management of patients with
myocardial infarction." Should these CPTs be in DB maybe with ICD Flag 0? ~ I don't think it's necessary
since they just say it is 'not necessary' - as opposed to something like 'not payable when submitted with'
or something more definitive like that.
Adding V70.7 as secondary (even though not in policy) (see Cahaba Mac A 33070)
ICD-9-CM Code V70.7 is used by institutions to denote a clinical trial, and requires an additional ICD-9-CM
code to be used
How to copy a policy in Utility
From any policy in MH12A (or wherever you're copying from), go to "Tools" then select "Copy
Policy"
Once the "Copy Policy" screen opens up, click on "File" then "Find Policies". Click okay in the
little box that tells you how many policies were found.
(You can confirm you're in MH12A by checking the "Payor" box near the top of the screen.)
In the top section, click on "copy policy history docs"
In the policy list, find the policy you want to copy and check the box next to it.
Back up at the top of the screen, select "File" then "Copy Policy"
Follow the prompts - Payor would still be MH12A, enter the policy number for the new policy,
the policy start date should be correct.
Then you'll get the message "Action completed. Policy copy successful." Click okay, then select
"File" and "Close" to exit the "Copy Policy" screen - or make another copy if you need multiples!
When you close that screen, the policy will not be in the dropdown list yet. You have to switch
payors, then go back to MH12A to get the policy to show up.
That's all there is to it! When I did the MXHA version of the policy, I made one copy first (the B
policy). Then in that B policy, I deleted all the CPTs that were going to stay in the main policy so
I would have less to worry about in the copies. I then made copies of the B policy for C, D, and
E and had less to delete from each one.
Oh, and don't forget to delete the CPTs in the B-E policies from the main policy - I always almost
forget that!
When retiring a policy:
I attach the new doc, then save, then sync (if there’s a sync policy) . Then I click the expire button and
add the retirement date, then save, then sync again. Then I check the CPT tab to make sure the rules
were actually retired!
I think in the past I’ve found the policy hasn’t retired if I don’t save in between attaching the doc and
retiring, or if I don’t use the expire button and instead just fill in the date in the box.
Attachments:
Since they are all URLs and they’re all pretty general, I don’t think we need to include them. If a client is
interested in one of them, they can use the URL themselves!
Supplemental Instructions Article:
As a separate issue, when I saw this was a supplemental instructions article, I thought there was
probably an LCD it should be linked with – and there is! This article should be linked to L31792, but for
whatever reason Palmetto hasn’t done that. So, what we really need to do is combine them in Utility.
Stephanie and I have talked about this before and this is what we think makes the most sense –
Add a note to L31792 in Utility to include A51162 in the doc. Do it in all caps to make it more
obvious!
You can add A51162 to Utility, but don’t add any coding. Just setup the policy number and
name (actually, what you have right now is perfect!).
Then, you’ll need to uncheck the export flags to the right of the policy number field, so Justin
ignores the policy when he does the exports.
Finally, add a big note at the bottom to indicate this article should be included with L31792
and to update there.
Do a new doc for L31792 that includes the article! Since the most recent update is the article,
you can use its effective date for the doc effective date.
When ICDs change from passing on its own to require secondaries
This is a tough one to remember, but when an ICD has passed on it's own, but now requires
secondaries, we have to expire it as a standalone and then re-add it and add the secondaries. I
went in a fixed it and updated the effective date for the rules with the secondaries.