The Pelvis (tutors)
advertisement

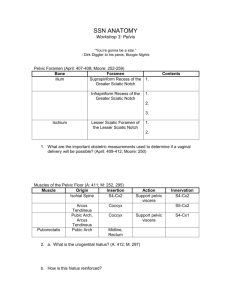
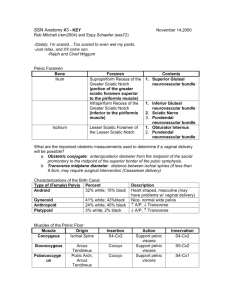
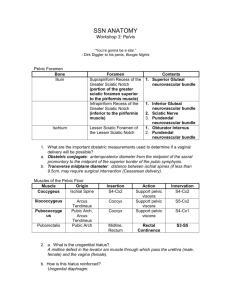
The Pelvis The pelvic cavity consists of the pelvic inlet, walls, and floor and contains elements of the urinary, gastrointestinal, and reproductive systems. - Inlet: S1, alae of sacrum, arcuate line, linea terminalis (pubic crest, pecten pubis, arcuate line), and pubic symphysis Walls: obturator internus, piriformis, sacrospinous and sacrotuberous ligaments, greater and lesser sciatic foramina, sacrum, coccyx, ischium, pubis Floor: levator ani (3 parts: iliococcygeus, pubococcygeus, and puborectalis), coccygeus, perineal membrane, muscles of deep perineal pouch Apertures of the Pelvis Aperture Greater Sciatic Foramen Lesser Sciatic Foramen Obturator Canal Boundaries Greater sciatic notch, sacrotuberous and sacrospinous ligaments, and the Ischial spine, it is divided into 2 parts by the piriformis Lesser sciatic notch, Ischial spine, sacrospinous and sacrotuberous ligaments Obturator membrane, obturator muscles, superior pubic ramus Gap between pubic symphysis and perineal membrane Pelvic Inlet Contents Above piriformis: superior gluteal nerves and vessels Below piriformis: inferior gluteal vessels and nerves, sciatic nerve, pudendal nerve, internal pudendal vessels, posterior femoral cutaneous nerves and the nerves to the obturator internus and quadrates femoris muscles Pudendal nerve and internal pudendal vessels, tendon of obturator internus Obturator nerve and vessels Dorsal vein of penis and clitoris S1, alae of sacrum, arcuate line, linea terminalis, and pubic symphysis Significance Communication between pelvic cavity and lower limb Above the pelvic floor Communication between gluteal region and perineum Below pelvic floor Communication between pelvic cavity and adductor region of thigh Communication between pelvic cavity and perineum Separates the true from the false pelvis, communication between the abdomen and the pelvic cavity Pelvic Outlet Pubic symphysis, bodies and inferior rami of pubis, rami of ischium, and the Ischial tuberosity, sacrotuberous ligament and coccyx Terminal parts of the urinary and GI tracts, and the vagina Area enclosed is the perineum Male vs. Female Pelvis: Characteristic Pelvic Inlet Male Heart-shaped, more distinct promontory of sacrum 50-60⁰ Prominent Female Circular, broader alae of sacrum Sacrospinous Connection Ischial spine and margins of sacrum and coccyx Sacrotuberous Ischial tuberosity to the PSIS and dorsolateral sacrum and coccyx Significance Create Sciatic Foramina and stabilize the sacrum by resisting upward tilting Create Sciatic Foramina and stabilize the sacrum by resisting upward tilting Stabilize lumbosacral joints Pubic Arch Ischial Spines 80-85⁰ Less prominent Ligaments of the Skeletal Pelvis: Ligament Iliolumbar Lumbosacral Anterior Sacro-iliac Interosseous Sacro-iliac Posterior Sacro-iliac Superior Pubic Inferior Pubic Transverse process of L5 to the ilium Transverse process of L5 to the sacrum Runs anteriorly and inferiorly to the sacro-iliac joint Immediately posterosuperior to the sacro-iliac joint and fills the gap between the ilium and sacrum Covers the interosseous sacroiliac ligament Above the pubic symphysis Below the pubic symphysis Stabilize lumbosacral joints Transmit forces from the lower limbs to the vertebral column Largest, strongest sacro-iliac ligament Transmit forces from the lower limbs to the vertebral column Transmit forces from the lower limbs to the vertebral column Muscles of the Pelvis: Muscle Obturator Internus Piriformis Levator Ani Coccygeus External Urethral Sphincter Deep Transverse Perineal Compressor Urethrae Sphincter Urethrovaginalis External Anal Sphincter Ischiocavernosus Bulbospongiosus Superficial Transverse Perineal Attachments Obturator membrane to greater trochanter Anterior sacrum to greater trochanter Posterior pubic bone, obturator internus, Ischial spine to perineal membrane, perineal body, around the anal canal, and anococcygeal ligament Ischial spine and sacrospinous ligament to coccyx and sacrum Inferior ramus of pubis and walls of deep perineal pouch to membranous part of urethra Ischial ramus to perineal body Ischiopubic ramus to its partner anterior to urethra Perineal body to its partner, surrounding the urethral and vaginal openings Anal canal and aperture to perineal body and anococcygeal body Ischial tuberosity and ramus to crus of penis or clitoris Perineal body to perineal membrane, corpus cavernosum, bulb of vestibule, body of clitoris, bulbospongiosus Ischial tuberosity and ramus to perineal body Innervation L5, S1: Nerve to obturator internus L5, S1, S2 Inferior rectal branch of pudendal nerve (S2-S4), and S4 ventral rami S3 and S4 anterior rami Perineal Branches of Pudendal Nerve (S2-S4) Perineal Branches of Pudendal Nerve (S2-S4) Perineal Branches of Pudendal Nerve (S2-S4) Perineal Branches of Pudendal Nerve (S2-S4) Pudendal Nerve (S2-S4) and branches directly from S4 Pudendal Nerve (S2-S4) Pudendal Nerve (S2-S4) Pudendal Nerve (S2-S4) Action Lateral rotation of extended hip, abduction of flexed hip Lateral rotation of extended hip, abduction of flexed hip Forms pelvic floor, supports pelvic viscera, maintains angle between rectum and anal canal, reinforces external anal sphincter, acts as vaginal sphincter Forms pelvic floor, supports pelvic viscera, pulls coccyx forward after defecation Compresses membranous urethra, relaxes during micturition Stabilizes perineal body Accessory sphincter of the urethra Accessory sphincter of urethra, may close the vagina Closes anal canal Retain blood in penis or clitoris Move blood into glans of penis or clitoris, in men: remove residual urine from urethra, pulsatile emission of semen Stabilize the perineal body Viscera of the Pelvis: - Rectum and Anal Canal: the rectum is continuous with the sigmoid colon at S3 and below at the anal canal as it penetrates the pelvic floor - Ureters: enter the pelvic cavity anterior to the bifurcation of the common iliac artery. They are crossed in the pelvis by the ductus deferens or uterine artery Bladder: most anterior pelvic viscera, expands into abdominal cavity when full. Consists of a apex (toward top of pubic symphysis, connected to median umbilical ligament [urachus]), base (faces posteroinferiorly, smooth mucosa, contains trigone), and the inferolateral surfaces (cradled between levator ani and obturator internus muscles). The neck of the bladder is the most inferior and fixed area anchored to the pubic bones by pubovesical or puboprostatic ligaments Urethra: begins at base of bladder and ends with external opening in perineum o Women: 4cm long and passes inferiorly through pelvic floor and into perineum, passing through deep perineal pouch and perineal membrane before opening into vestibule between labia minora. Skene’s glands are associated with the lower end of urethra. o Men: 20cm long and passes through prostate, deep perineal pouch, perineal membrane, and enters the root of the penis. The male urethra is divided into 4 parts: - Preprostatic: 1cm, internal urethral sphincter (prevents semen from flowing backward into bladder). -Prostatic: 3-4cm, contains urethral crest, prostatic sinus, seminal colliculus, and prostatic utricle. Connection between urinary and reproductive tracts occurs here. -Membranous: narrow, passes through the deep perineal pouch where it is surrounded by the external urethral sphincter (skeletal muscle). -Spongy: surrounded by erectile corpus spongiosum, forms a bulb at the end of the penis called the navicular fossa. The bulbourethral glands enter into the spongy urethra. Vulnerable to damage during catheterization. - - The Perineum: inferior to the floor of the pelvic cavity - - Contains: Terminal openings of the GI and urinary systems, External openings of reproductive tract, and Roots of the external genitalia Bounded by: the pubic symphysis, coccyx, ischiopubic rami (Anterolateral), and sacrotuberous ligaments (posteriorly), levator ani (roof) Pudendal nerve (S2-S4) and Pudendal artery are main nerve and artery of the region 2 Triangles: divided by imaginary line between the two Ischial tuberosities o Urogenital: anterior triangle, in the horizontal plane, contains openings of the urinary systems and reproductive systems (in the Urogenital hiatus), the perineal membrane anchored to the perineal body, the superficial perineal pouch (contains erectile fibers), and this triangle functions to anchor the external genitalia (via the perineal membrane and deep perineal pouch) o Anal : posterior triangle, faces posteriorly, contains the anus and the external anal sphincter (3 skeletal muscle parts: deep, superficial, and subcutaneous) Ischio-anal Fossae: Inverted wedge shaped gutters between the levator ani muscles, deep perineal pouch, and the adjacent pelvic walls (ischium, obturator internus, and sacrotuberous ligament). o The anterior recesses project into the Urogenital triangle superior to the deep perineal pouch o Allow movement of the pelvic diaphragm and expansion of the anal canal during defecation o Normally filled with fat Layers of Pelvic Floor: Deep to Superficial 1 2 3 Structure Levator ani and coccygeus muscles Superior fascia Deep Perineal Pouch 4 5 Perineal Membrane Superficial Perineal Pouch 6 Inferior (superficial) fascia Contents Skeletal muscle Ischio-anal fossae and recesses (fat) External urethral sphincter, sphincter urethrovaginalis, compressor urethrae, deep transverse perineal muscles, bulbourethral glands Fibrous membrane Erectile structures that form the penis or clitoris, bulbs of vestibule, glans clitoris, corpus spongiosum (proximal part is bulb of penis) skeletal muscles: ischiocavernosus, bulbospongiosus, superficial transverse perineal A membranous deep layer, Colles’ fascia , which is attached to the perineal membrane and ischiopubic rami (it does not extend into the anal triangle or into the thigh). It defines the external limits of superficial perineal pouch and enters the scrotum/labia and extends around the body if the penis/clitoris *Because this layer is continuous with the abdomen, infectious materials that accumulate in the superficial perineal pouch can track out of the perineum and enter the lower abdominal wall* Male Reproductive System: Structure Testis Epididymis Ductus Deferens Ejaculatory Duct Urethra Penis Prostate Gland Seminal Vesicles Bulbourethral Glands Location Inside scrotum, attached to abdominal wall by spermatic cords Function Produce sperm cells in seminiferous tubules Posterolateral side of testes Stores sperm as they mature before ejaculation Scrotum, inguinal canal, bends medially around inferior epigastric a., crosses external iliac v. and a. , pelvic cavity, crosses ureter, inferomedially along bladder, anterior to rectum, and enters duct of seminal vesicle Through prostate gland From neck of bladder to the external urethral opening in tip of penis Outside of body in pubic region, attached to the pubic arch and anchored to the perineal membrane Inferior to bladder, posterior to pubic symphysis, and anterior to rectum Between bladder and rectum Within deep perineal pouch, lateral to membranous urethra Transports sperm from the tail of the epididymis to the ejaculatory duct Carries secretions of ductus deferens and seminal vesicles into urethra Conducts urine from bladder to outside of body Conducts urine and semen Contributes secretions to semen Contributes significant secretions to semen Contribute to lubrication of the urethra and preejaculatory emissions Key Features Tunica vaginalis, tunica albuginea, rete testis, mediastinum testis Head (efferent ductules), (true epididymis) body and tail Very long Penetrates prostate to enter urethra 4 parts: preprostatic, prostatic, membranous, and spongy Copulatory organ Erectile tissue, composed of 2 corpora cavernosa and a corpus spongiosus. As a bulb, roots (crura), body , and glans Surrounds urethra Accessory gland Ducts open into spongy urethra at the root of the penis Female Reproductive System: Structure Ovaries Uterine Tubes Uterus Vagina Clitoris Greater Vestibular Glands Para-urethral Glands Location Adjacent to lateral pelvic wall just inferior to pelvic inlet Produce egg cells Project laterally from body of uterus, passing superiorly over ovaries Conduct egg cells into body of uterus Midline, between bladder and rectum Holds developing fetus during pregnancy Extends from cervix, through pelvic floor, and perineum to the outside of the body (introitus). Between bladder and rectum. Beneath pubic symphysis and the underside of the ischiopubic rami and anchored to the perineal membrane Located posterior to the bulbs of the vestibule on either side of the vaginal opening Located on either side of the urethra, its ducts open into the vestibule at the lateral margins of the urethral opening Function Accepts semen deposited during intercourse, serves as birth canal during childbirth Great sensitivity Produce lubricating secretions during arousal Produce lubricating secretions Key Features Suspended by mesovarium, connected to body wall by suspensory ligament and to uterus by ligament of ovary Enclosed by mesosalpinx, Have fimbriae, infundibulum, and ampulla (usual site of fertilization) Consists of a fundus, body, and cervix (canal forms external and internal os, and it forms fornix at junction with vaginal wall) Copulatory organ in women Composed of the glans and the corpora cavernosa: has a root and a body Also called Bartholin’s Glands, found in superficial perineal pouch Also called Skene’s Glands Erectile Tissues: - - Erection is a vascular event mediated by the parasympathetic fibers of the pelvic splanchnic nerves (anterior rami of S2-S4) The pelvic splanchnics branch from the hypogastric plexus and pass through the deep perineal pouch and perineal membrane to innervate the erectile structures in the superficial perineal pouch Stimulation of these nerves causes branches of the internal pudendal arteries to relax, allowing blood to fill the penis or clitoris, causing erection Branches of the Pudendal nerve (S2-S4) carry sensory nerves from the penis/clitoris Fascia, Peritoneum and Ligaments: continuation of extraperitoneal connective tissue of the abdomen Fascia Rectovaginal Pubocervical Ligament Transverse Cervical Ligament Uterosacral Ligament Vesico-uterine Pouch Pouch of Douglas (recto-uterine) Recto-uterine Folds Broad Ligament Prostatic Rectovesical Pouch Rectovesical Septum Suspensory Ligament of Penis Fundiform Ligament of Penis Location/Function Separates the posterior surface of the vagina from the rectum Stabilize the uterus in the pelvic cavity (Cardinal Ligament) Stabilize the uterus in the pelvic cavity Stabilize the uterus in the pelvic cavity Between the bladder and the uterus Between uterus and rectum Raised ridge of peritoneum on each side near the base of the rectouterine pouch. Covers the Uterosacral ligaments. Runs from lateral pelvic walls to the uterus and covers the ovaries, uterine tubes, round ligaments and ligaments of ovaries (remnants of gubernaculum) Contains and surrounds the prostatic plexus of veins Occurs between the bladder and the rectum Separates the posterior surface of the prostate and the base of the bladder from the rectum Supports base of body of penis, attached superiorly to pubic symphysis Supports body of penis, attached to the linea alba of the anterior abdominal wall and splits into 2 bands that unite under the penis Important Nerves in the Pelvis: Sacral Plexus: - Formed by the anterior rami of the lumbosacral trunk (L4-L5) and S1-S4. S4 only has a ventral division. It is located anteriorly to the piriformis muscle. The pelvic visceral nerves (S2-S4) provide parasympathetic fibers to the inferior hypogastric plexus Major Branches include: sciatic, superior and inferior gluteal, pudendal nerve, nerve to obturator internus, nerve to quadrates femoris and inferior gemellus, piriformis, and levator ani, posterior cutaneous and perforating cutaneous nerves Coccygeal Plexus: - Formed by the anterior rami of S4-Co Form the anococcygeal nerves Penetrate the coccygeus muscle, overlying sacrospinous and sacrotuberous ligaments, passing superficially to innervate the skin in the anal triangle Superior Hypogastric Plexus: situated anterior to vertebrae L5 between the promontory of the sacrum and the bifurcation of the aorta. Hypogastric Nerves: the entrance of the prevertebral plexus into the pelvis, crossing the pelvic inlet medially to the internal iliac vessels. Formed b y the separation of the superior hypogastric plexus into right and left bundles. Inferior Hypogastric Plexus: form when hypogastric nerves are joined by the pelvic splanchnic nerves carrying parasympathetic fibers. Gives rise to: - - Rectal plexus Uterovaginal Plexus Prostatic Plexus Vesical Plexus Cavernous Nerves: terminal branches supplying the erectile tissues of the penis and clitoris Sympathetics: T10-L2, innervate blood vessels, contract internal anal and urethral sphincters, smooth muscle contraction of reproductive glands and tract, and move secretions from the epididymis and accessory glands into the urethra to form semen. Parasympathetics: S2-S4, vasodilatory, contract bladder, stimulate erection, modulate enteric nervous system of the colon distal to left colic flexure. Visceral Afferents: follow sympathetic (these VAs carry pain) and parasympathetic (these VAs carry receptor information) fibers to the spinal cord Pudendal Nerve: leaves greater sciatic foramen inferior to piriformis, passes around sacrospinous ligament, then enters the anal triangle by passing through the lesser sciatic foramen to supply the perineum. 3 terminal branches: - Inferior Rectal Nerve: external anal sphincter, levator ani, skin of anal triangle Perineal Nerve: motor to muscles of deep and superficial perineal pouches and sensory to skin of scrotum/labia Dorsal Nerve of Penis/Clitoris: sensory to penis/clitoris Nerve Sciatic Pudendal (accompanied by internal pudendal vessels) Superior Gluteal Inferior Gluteal Nerve to Obturator internus Cord Levels L4-S3 Inferior to piriformis Motor Posterior thigh, and the leg and foot S2-S4 Inferior to piriformis, through lesser sciatic foramen Skeletal muscles of perineum (external urethral and anal sphincters, levator ani) L4-S1 Superior to piriformis Gluteus medius, gluteus minimus, and tensor fascia latae Gluteus maximus L5-S2 Inferior to piriformis L5-S2 Obturator internus and Superior gemellus Sensory Skin of foot (tibial part) and lateral leg (common fibular part) Skin of perineum, penis, and clitoris Nerve to quadrates femoris and inferior gemellus Posterior Femoral Cutaneous Perforating Cutaneous Nerve to Piriformis Nerves to levator ani, coccygeus, and external anal sphincter L4-S1 Inferior to piriformis S1, S3 Inferior to piriformis S2, S3 Through sacrotuberous ligament L5, S1, S2 S4 Pelvic Splanchnic Nerves S2-S4 Anococcygeal Nerves S4-Co Quadrates femoris and inferior gemellus Skin of posterior thigh Skin over gluteal fold Piriformis Levator ani, coccygeus, and external sphincter Visceral: stimulate erection, modulate mobility of GI system distal to left colic flexure, inhibits internal urethral sphincter Skin between anus and coccyx Visceral: visceral afferents from pelvic viscera and parts of distal colon. Pain from cervix and possibly from bladder and proximal urethra Perianal skin Dermatomes of the Perineum and Pelvic Floor Arteries of the Pelvis: The Internal Iliac Artery on each side is the major artery for the pelvis and perineum; it originates from the Common Iliac Artery anteriorly to the disc between L5 and S1, courses inferiorly over the pelvic inlet, dividing into anterior and posterior trunks at the level of the superior border of the greater sciatic foramen. o o Posterior trunk: lower posterior abdominal wall, posterior pelvic wall, and gluteal region Iliolumbar Artery: divides into lumbar, spinal, and iliac branches Lateral Sacral Arteries Superior Gluteal Artery Anterior Trunk: pelvic viscera, perineum, gluteal region, and the adductor region of the thigh. Umbilical Artery Superior Vesical Artery Inferior Vesical Artery or Vaginal Artery Middle Rectal Artery Obturator Artery Internal Pudendal Artery: many branches to perineum Inferior Rectal Artery Perineal Artery: Transverse Perineal Branch and Posterior Scrotal/Labial Artery Artery of Bulb of Penis/Vestibule Urethral Artery Deep Artery of Penis/Clitoris Dorsal Artery of Penis/Clitoris Inferior Gluteal Artery Uterine Artery External Pudendal Arteries: a superficial and a deep vessel that originate from the femoral artery: enter the perineum and supply the skin of the penis/clitoris and scrotum/labia majora Testicular/Ovarian Arteries: originate from the abdominal Aorta Cremasteric Arteries: originate from the inferior epigastric branch of the external iliac artery, accompanying the spermatic cord into the scrotum Veins: The veins of the pelvis drain into the internal iliac veins which join the common iliac veins. Veins associated with the rectum and anal canal drain into the portal system. The Pelvic Plexus is an important portacaval shunt when the hepatic system is blocked. - Internal Pudendal Vein Internal Iliac Vein Obturator Vein Pelvic Plexus o Vesicular o - Rectum: internal (between internal anal sphincter and epithelium lining the anal canal) and external (encircles the external anal sphincter and is subcutaneous)parts drain via the superior, middle, and inferior rectal veins into the portal and caval systems o Prostate o Uterus o Vagina Deep Dorsal Vein: drains erectile tissues of penis or clitoris. Joins the prostatic plexus in men or the vesicle plexus in women Median Sacral Veins: join to empty into the left common iliac or the junction of the common iliac veins Ovarian Veins: the left one joins the left renal vein and the right one joins the IVC External Pudendal Veins: come from great saphenous vein in thigh and drain the superficial skin of the penis or clitoris and scrotum or labia majora Important Anastomoses: - Uterine artery with Ovarian and vaginal arteries (uterine and vaginal from anterior internal iliac and ovarian from abdominal aorta) Middle rectal artery (from anterior internal iliac) with superior rectal artery (inferior mesenteric)and the inferior rectal artery (internal pudendal) Median Sacral artery (from posterior abdominal aorta) with the iliolumbar and lateral sacral arteries (from posterior internal iliac) Pelvic Plexus: rectum, bladder, prostate, uterus, vagina Dorsal Artery of Penis with Deep Artery of Penis and the Urethral Artery Lymph Drainage: Remember that lymph follows the major arterial supplies! Region Testes, Ovaries and related parts of Uterus and Uterine Tubes Pelvic Viscera, Gluteal region, deep areas of Perineum Superficial tissues of Penis/Clitoris and Scrotum/Labia Majora Glans Penis/Clitoris, Labia Minora, and lower Vagina Nodes Providing Drainage Lumbar nodes and pre-aortic nodes Internal Iliac Nodes Superficial Inguinal Nodes Deep Inguinal Nodes and External Iliac Nodes Clinical Correlations: - Femoral Artery: palpated midway between ASIS and pubic tubercle, inferior to inguinal ligament Bone Marrow Biopsy: iliac crest often used because it lies close to the surface and is easily palpated Obstetric Pelvic Measurements: transverse and Sagittal measurements of pelvic inlet and outlet can help predict likelihood of safe vaginal delivery. Obtained by using radiographs and MRIs - - - - - Defecation: quadrates lumborum, rectus abdominis, external and internal obliques, and transversus abdominis contract to raise intra-abdominal pressure. The puborectalic (levator ani) relaxes to allow straightening of the anorectal angle (increase angle from 90⁰ to about 135⁰) as the external and internal anal sphincters relax to shorten the anal canal and allow passage of feces Episiotomy: an incision in the skin and perineal body to allow room for the fetus to pass through the vagina to prevent stretching and tearing of the perineal body. A clean incision is easier to suture than a complex jagged tear. A posterolateral episiotomy bypasses the perineal body and a median episiotomy cuts through the perineal body. Digital Rectal Examination: can palpate anal mucosa, posterior wall of vagina and cervix or the prostate gland. Suprapubic Catheterization: catheterize the bladder through the anterior abdominal wall above the pubic symphysis. Urethral Catheterization: women are easier because the urethra is very short and nearly straight. The male anatomy can make it more challenging, the spongy urethra is vulnerable to injury because of its angles. Vasectomy: surgical dissection and division of the ductus deferens, can be performed through skin above inguinal canal instead of entering the abdomen or pelvis Tubal Ligation: clip the uterine tubes to prevent eggs from entering the uterus to be fertilized Recto-uterine Pouch (Pouch of Douglas): site of collection for infected fluids and materials in the pelvic cavity because it is the lowest portion of the abdominopelvic cavity Pudendal Block: given where the pudendal nerve crosses the lateral aspect of the sacrospinous ligament near its attachment to the Ischial spine. Ischial spines are palpated transvaginally, and the needle is passed through the skin above the medial aspect of the Ischial spine Prostatectomy and Impotence: when the prostate is removed, the seminal vesicles are removed with it and the pelvic splanchnic nerves in the inferior hypogastric plexus may be disturbed causing erectile dysfunction/impotence Clinical Finding Pelvic Fracture Sacro-iliac joints Urinary Stones Bladder Cancer Anatomy Involved Bony rings of pelvis: pelvic inlet and obturator foramina Fibrous and synovial components of joint Kidneys, Ureters, bladder, urethra Bladder, sometimes rectum, uterus, prostate gland, and lateral pelvic walls Patient Presents With Large hematoma, disruption/compression of urethra, bowel, nerves/vessels Pain and discomfort in sacroiliac region Problems emptying bladder, pain referred to pubic, flank, inguinal areas, and lateral/medial thighs. Other complications of urinary, GI, and/or reproductive tracts as the cancer spreads Miscellaneous Cause significant bleeding Can be caused by rheumatoid arthritis, IBD, and psoriasis Residual urine left in bladder may become infected and alter pH Can spread via internal iliac lymph nodes Bladder Infection Bladder, urethra Cystitis (inflammation of bladder) Testicular Cancer testes Prostate Problems Prostate gland, urethra Hysterectomy Uterus, uterine tubes, ovaries Internal and External rectal venous plexuses at or inside the anal sphincter Abnormal lumps felt in scrotum Hard, enlarged prostate, problems urinating due to compressed urethra Reproductive malignancy, endometriosis, excessive bleeding External hemorrhoids cause pain, swelling (pudendal nerve innervation), internal hemorrhoids usually bleed, but do not cause pain Anal canal, ischio-anal fossae Tear in anal canal leading to infection Hemorrhoids Abscess in ischioanal fossae Urethral Rupture Urethra, surrounding tissues/fascias Hydrocele, Varicocele Testes, scrotum, pampiniform venous plexus Straddling injury, urine collects in scrotum and deep to superficial abdominal fascia. In pelvic fractures the prostatic/membranous urethra may be torn and urine will collect inside the true pelvis Hydrocele- enlarged scrotum Varicocele- “bag of worms” Women more susceptible because of short urethras Occur in younger patients Prostate cancer is one of the most common cancers in men Pfannenstiel’s incision used (transverse Suprapubic) Pectinate line distinguishes between external and internal hemorrhoids Caused by straining, obesity, sedentary life Infection may tract into pelvic cavity or laterally into the i-a fossae Proximal spongy urethra is most commonly ruptured Most serious is related to disruption of puboprostatic ligaments