File
advertisement

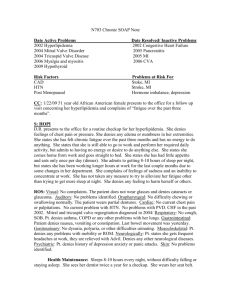
SUBJECTIVE CC/Reason for Visit: “I have had this nasty cough and I get shot winded when I try do anything for the last week.” HPI: NC is a 66-year-old Caucasian male who presented to the clinic with complaint of an ongoing “nasty” productive cough and dyspnea on exertion that won’t go away. Patient describes cough as moist, productive with a moderate amount of yellow, thick sputum, which he is able to expectorate. Patient reports that cough is worst at night time when he is in a supine position, and is significantly interfering with his ability to get a good night’s sleep. He reports having to sleep in the recliner the past couple of nights in order to get any rest at all due to the coughing attacks he has when lying down. Patient stated he has tried drinking some honey mixed with lemon with a little bit of whiskey to soothe his throat and cough but reports modest if any improvement. He has not taken any over the counter medications for fear of interactions with his prescription medications. Exacerbating factors for SOB consist of activities of daily living such as bathing, getting himself dressed, and picking up the kitchen, working in the small garden in his backyard. Relieving factors consist of rest. He confirms that he has continued use of all of his medications including his Spiriva, Advair, and albuterol inhalers for his Chronic Obstructive Pulmonary Disease (COPD). In January 2014, patient was started on Advair, in addition to his anticholinergic inhaler, Spiriva, and short acting beta agonist, albuterol which has help reduced the use of his albuterol rescue inhaler to 1-2 times per week. Patient states, “because of this cough which I am worried about, I am beginning to use my albuterol inhaler more than usual, about 3-4 times per day to relieve this short windedness.” Patient denies fever or body aches states he have occasional chills and occasional night sweats. Patient complains of pleuritic chest pain, denies hemoptysis or any swelling of his lower extremities. Patient complains of anorexia but denies nausea or vomiting, and while he reports a sore throat, he denies dysphasia or difficulty maintaining adequate liquid oral intake. He denies rhinorrhea, facial pain, ear pain, or nasal congestion. He denies any changes in vision, hearing, or sense of smell. He complains of increase insomnia related to his cough stated “even though I can’t sleep sometimes it is worst with the cough” patient reports that he continues to smoke cigarettes but has tried to reduce to only two cigarettes per day. Patient denies being around anyone that has recently been sick. Past Medical History: 1.Hypertension 2.Dyslipidemia 3.COPD 4.Gastroesophageal reflux disease 5.Diabetes mellitus II 6.PTSD Allergies: Penicillin (causes patient to breakout in hives) No allergic to latex or any foods that he is aware of Current Medication: Lisinopril 20mg by mouth daily Hydrochlorothiazide 12.5mg by mouth daily, Metoprolol 50mg by mouth twice daily, Atorvastatin 40mg by mouth daily, Protonix 40mg by mouth daily, Metformin 500mg XR by mouth twice daily Glyburide 2.5mg by mouth daily, Aspirin 81 mg po daily, Spiriva handihaler 18mcg/cap 1 cap inhaled daily, Advair diskus 250/50 1 inhalation twice daily, ProAir HFA 2 puffs every four to six hours as needed for shortness of breath. Trazodone 25mg po QHS as needed for insomnia 65 years old male with multiple cor-mobidities Immunization: Influenza vaccine annually last received October 2013. Pneumovax vaccine in 2011 Zostavax and TDap vaccines in 2010. Patient reports that he believes he is current on any childhood vaccinations. Medical history: Hospitalization: 1958 Appendectomy 1975 Unspecific knee surgery from injury in the Vietnam War in 1972 Childhood Illness: Chicken pox and measles Past surgical history: Appendectomy in 1956, Unspecified right knee surgery in 1972 after injury from the Vietnam War, Colonoscopy in 2001 that was benign, Esophagogastroduodenoscopy and colonoscopy in 2007 in which two polyps were removed from his colon and esophagitis was diagnosed. Family History: Father had hypertension, high cholesterol, and Deceased from an acute myocardial infarction at age 73. Mother 83 living in overall good health suffers from dementia. Brother 60, HTN but otherwise is in good health. Sister deceased at age 39 MVC. Children ages 27 years and 32 in overall good health Grand children 5 years and 3 years alive and well Patient denies any family history of cancer, asthma, stroke, kidney disease, vascular disease, livers disease, seizure disorder, bleeding disorder, or mental illness. Social History: Married lives in a private home on several acres of land with his wife of forty years. -2 sons age 27 and 32 both alive and well 2 granddaughters ages 5 years and 3 years both alive and well. -Smokes ½ pack of cigarette a day for the past 40 years. -Occasional consumes alcohol usually beer about 3times a week - Vietnam war veteran 1970-1972 He also tends their ½ acre garden. Until his recent illness, he denies any difficulty with his activities of daily living, but he reports that in the last few weeks he has had to cut back his hours at work and ask for help in the garden. ROS: (1) Constitutional symptoms- Patient reports fatigue, chills, and decreased appetite, but denies any recent weight loss of which he is aware. He reports recent antibiotic use as noted in the chart. He denies any recent international travel, a past PPD skin test, or possible known exposure to tuberculosis. NC denies exposure to occupational hazards or chemicals, reporting that he works mostly in the office these days. He does report; however, he used to work on the farm more often and was exposed to various pesticides. . (2) Eyes- No history of vision problems, Denies double or blurred vision, no use of corrective lenses or medications. Bilateral watery and itchy eyes without crusting, inflammation. (3) Ears, nose, mouth and throat- Ears: denies hearing changes, tinnitus, vertigo, drainage, or pain, hearing acuity, exposure to high noise level, tinnitus, and presence of infection or pain, vertigo, no use of assistive hearing device. Nose: He denies, rhinorrhea, nasal congestion, He denies any changes in his vision, hearing or sense of smell Mouth and teeth: History of smoking and occasional drinking Cigarettes, denies sores, bleeding, and toothaches. Last dental exam date August 2014 brushes teeth at least twice a day with fluoride toothpaste, no problem with dentition. Throat: complains, sore throat (4) Cardiovascular- Complains of chest tightness, denies chest pain, palpitations, DOE, edema, claudication, or history of heart murmur, History of high blood pressure and dyslipidemia (5) Respiratory- complains of persistent cough, sore throat and shortness of breath with activity and occasional chest tightness. He denies hemoptysis, just slight pain upon inspiration in left chest but not on expiration. Patient does report orthopnea and has been sleeping in the recliner. Denies history of recent respiratory infections. (6) Gastrointestinal- He complains of anorexia but denies nausea, vomiting, abdominal pain or change in bowel habits or stool color or consistency. He denies blood in his stool. He reports occasional heartburn that it is usually self-limiting. (7) Genitourinary- He denies hematuria, dysuria, incontinence, change in urinary frequency, or difficulty starting or stopping his stream of urine. Patient denies any change in sexual partners, sexual interest. (8) Musculoskeletal- He denies muscle pain or body aches, joint swelling, or extremity weakness. (9) Integumentary (skin and/or breast)- Denies rash, urticarial, bruising, change in color, or hair loss. Patient enjoys working in his garden and routine use of skin protection with sun exposure and does routinely checks for any changes in skin color or moles. (10) Neurologic- Patient denies syncope, seizures, disorientation, anxiety, recent falls, or difficulty with balance (11) Psychiatric- Patient is Vietnam war veteran served from 1970- 72 and has history of PTSD, stated he sometimes has insomnia but using trazodone sometimes helps, denies history of depression, anxiety no mood changes, nervousness, denies suicidal thoughts. (12) Endocrine- denies polydipsia, polyuria, polyphagia, cold/heat intolerance, complains of appetite change or weight changes. History of Diabetes type 2, no hyper/hypothyroidism (13) Hematologic/lymphatic- He denies any signs of bleeding in the form of excessive bruising or bleeding from his gums. (14) Allergic/immunologic- History of seasonal allergies but denies having any problems at the moment. OBJECTIVE: Physical Exam: (1) General-Constitutional: Mr. is a 65 years old white male alert and oriented, ambulatory with slight limp who appears his stated age and is appropriately groomed. He appears obviously ill but is in no apparent acute distress at this time. He is oriented to person, place, and time, reliable and has no difficulty staying on topic and maintaining fluent conversation. Height (without shoes): 74 Inches Weight (dressed): 233 BMI: 28.4kg/m2 Vital signs: T 99.8 orally, Pulse BPM, Resp 18, BP 135/76, O2 92% RA Head and Neck: normocephalic, atraumatic, no hematomas, or tenderness Mild pressure reported upon palpation of maxillary sinuses. Neck supple non-tender without lymphadenopathy, trachea at midline (2) Eyes- sclera white, and conjunctiva pink, but pale, without evidence of icterus, excessive tearing or exudate. Eyelids are non-remarkable and appropriate for race without edema or lesions. His pupils are equal, round, reactive to light and accommodating. His corrected visual acuity and extra ocular eye movements are intact. (3) ENT-. Ears: Normal hearing, External ears without trauma or drainage. Auricle, tragus, mastoid non-tender to palpation. Bilateral ear canal patent without erythema, edema, or exudate. Bilateral tympanic membranes are intact with good cone of light. NOSE: nose unremarkable, bilateral nares patent, septum midline. MOUTH: Posterior oropharynx erythematous without tonsillar edema or exudate, mucous membranes pale and moist without ulceration (4) Cardiovascular- apical pulse is not visible but is barely palpable at a downward displaced location of the 6th intercostal space mid-clavicle line without thrill, lift, or heave. Mild JVD at this time approximately 6 cm with the exam table elevated to 30 degrees. Bilateral carotid upstrokes are brisk and without bruits. Auscultation of the heart reveals a regular rate and rhythm with crisp S1 and S2 that were accompanied by a soft S3 barely audible with the bell of the diaphragm. No murmur is noted. (5) Respiratory- He is tachypenic, but does not appear to be in acute respiratory distress and no use of accessory muscles and is not exhibiting stridor or retractions. Patient is able to carry on a conversation without respiratory compromise. He is noted to have a barrel shaped chest with an increased anterior- posterior diameter that is non-tender with symmetric expansion. Diaphragmatic excursion 6cm with increased tactile fremitus bilaterally, but more pronounced over the left lung field. Resonance noted upon percussion in the bilateral upper lung field dull upon percussion of bilateral lower field. Bilateral breath sounds are vesicular with diffuse crackles that do not clear with cough, audibly congested cough on auscultation. . (6) Gastrointestinal- Stomach round, bowel sounds active on all four quadrants, Abdomen soft, non-distended, non- tender. No presence of abdominal bruits or palpable pulsations. There are no palpable masses or organomegaly (7) Gastrourinary- deferred not directly related to HPI (8) Musculoskeletal- slight deformities to right knee joint previous injury in Vietnam War. Slight limp gait, good range of motion in other joints. (9) Integument /lymphatic pertaining to each location: grossly intact, warm, dry, and without rash or lesion. Skin fragile, good turgor and capillary refill < 3 sec. 2+ palpable radial and dorsalis pedis pulses bilaterally. No extremity edema, trophic skin changes, or stasis changes are noted. Feet dry intact without lesion, blister or sore. Monofilament intact bilaterally. (10) Neurologic: Alert and oriented X4 cranial nerve II-XII intact. Sensation intact to pin prick and touch throughout. Reflexes 2+ throughout, (11) Psychiatric: Non-judgmental, (12) Hematologic/Immunologic- No areas of bruising noted, no open bleeding area noted Labs: Today a CBC with differential shows leukocytosis with a total white blood count of 14.3 and an elevated absolute neutrophil at 67.9%. Leukocytosis with elevated neutrophils leads toward the diagnosis of a bacterial infection. -BMP was within normal limits. CBC with Diff and BMP were both order because due to cough, SOB, elevated temp, chills and night sweats. -A stat chest x-ray was ordered – This was ordered because of SOB, left lower lobe infiltrates, indicative of pneumonia Assessment/Analysis 1. Community Acquired Pneumonia (ICD-9: 482.9) symptomatology of shortness of breathes, noisy productive cough, crackles upon auscultation. Pleuritic chest pain, increased tactile fremitus and left sided dullness accompanied by tachypnea, and chills support the clinical presentation of a patient with pneumonia. Patient’s diagnostics labs of neutorphilia on his CBC with differential and presence of left lower lobe infiltrates on his chest x-ray along with fever and decreased oxygen saturation further support the diagnosis of community acquired pneumonia 2. Congestive Heart Failure (ICD-9 428.0): This is a possible diagnosis Congestive heart failure would be most likely accompanied by an elevation in pro-BNP and patient would not only have shortness of breath, orthopnea, with an extra heart sound S3 but also some expected peripheral edema and pulmonary edema, hepatomegaly, JVD or effusions on chest x-ray. 3. Aspiration lung injury (ICD -9: 507.0). While aspiration lung injury would likely be noted in a dependent lung lobe, the patient does not have dysphagia or an impaired gag reflex, and symptoms would most likely have had a more acute onset. Patient didn’t complain of any vomiting, that could have suspected if he aspirated. While this is likely it is not possible. 4. COPD exacerbation (ICD-9 473.9). While the patient must have had COPD exacerbations in the past, he presents with additional symptoms in addition to just he coughing, purulent sputum, and tachypnea shortness of breath and decreased oxygen saturation. Furthermore, the hyperinflation that was noted on patient’s chest x-ray was not accompanied this time by infiltrates, this is not specific to COPD but to another disease process. Also, CBC showed some bacteria involvement in the disease process. 5. Viral URI: (ICD-9 487). Patient presented with cough, slight fever, chills, sore throat, no complains of body ache, negative complains of headache and neg purulent sputum with Viral URI, neg tachypnea, symptomatology may suggest this but based on diagnostic lab data indicative of a bacterial, not viral process this can be excluded in the differential. 6. Health maintenance issues: Overweight (ICD -9: 278.02): BMI 28.4 Smoking (patient has a history of 40 years) PLAN 1. Community Acquired Pneumonia (CAP). (ICD-9: 482.9) Based on the above subjective, objectives and diagnostics, the definitive diagnosis is CAP. 2. Patient is instructed to continue all of his current medications in addition to his two new prescriptions. 3. Increase fluid intake especially clear fluids and get plenty of rest. 4. Medications: New RX: 1). Levofloxacin (Levaquin) 750mg PO daily x 5days. Dispense 5, no refills. A respiratory fluoroquinolone is an appropriate antimicrobial choice for CAP. 2). Prednisone 40mg PO daily x 7 days. Dispense 7, no refills. A corticosteroid to help control inflammatory process in patient’s lungs that is worsening his respiratory status, In addition to appropriate antimicrobial coverage, is prescribed 6. Overweight and smoking: Schedule well- visit for patient for consultation regarding specific lifestyle modification intervention Atorvastatin (Lipitor) 40mg PO at bedtime a). Indication for patient: Prescribed for patient mixed dyslipidemia b) MOA: Atorvastatin inhibits 3-hydroxy-3- methylglutaryl- coenzyme A (HMG- CoA) reeducates c). Usual Dose: Usual adult dosing is between 10mg -80mg d). Available as name brand, generic or both: Available as both brand name and generic e). Cost out the medication a 3 different pharmacies: Names of pharmacies -Publix 2415 Moore’s mill Rd Auburn -Wal-Mart 1717 S. College St -Target 2640 Enterprise Drive f). Cost of prescription at each pharmacy as prescribed - Publix Pharmacy: Estimated cash price $ 110.95 they accept coupon, which brings the price down to $15.75 and covered by most insurance. -Wal-Mart Pharmacy: Estimated cash price for a 30-day supply is $30 and $16.25 with a coupon. -Target Pharmacy: Estimated cash price without insurance for a 30 day supply for 30 days supply is $49.99 and $16.25 with a coupon and covered by most insurance Intervention: 1). In- office intervention: CBC with diff, Basic metabolic panel, and Chest xray. 2). Patient is advised to complete all course of antibiotic. It is recommended to him that he take the medication with food at approximately the same time each day in order to achieve a constant concentration in his blood stream. Patient is informed of the rare occurrence, but increased risk, of tendonitis and tendon rupture associated with fluoroquinolones, especially in combination with corticosteroids. Because steroid will increase your blood glucose level, it will be very important to keep a tight control on your monitoring make sure you check your glucose for the next 2-4 weeks more regularly to make sure it is not running extremely high. 3). Veteran is also instructed that in the event of pain, swelling, inflammation, inability to bear weight, or a tendon snap in the ankles, shoulder, hands or other tendons to immediately quit taking the levofloxacin and call the health line. Veteran is instructed that while therapy is initiated as outpatient; he is to return to the clinic if symptoms get worst or does not improve within 48-72 hours. He is informed to return to the clinic in the event of temperature greater than 101.0 F, leg swelling, or continued orthopnea despite daytime improvements. Health Maintenance: 1. Need to explore motivation to lose weight, set target weight loss by next well visit. 2. Smoking cessation is encouraged and receptiveness and readiness assessed. 3. Explore alternative nicotine titration therapies such as e-cigarettes, nicotine transdermal, gum system 4. Offer referral to tobacco cessation program Evaluation: 1. Schedule a formal follow-up appointment with a chest x-ray in six weeks. If his radiograph has not cleared at this time or his S3 hear sound persist, he will require increased collaboration with preceptor’s collaborating physician and probable referral to a cardiologist for further evaluation. 2. Patient and his wife are instructed that in the event of increased shortness of breath unrelieved by rescue inhaler, chest pain, or respiratory distress; he is to report to the local emergency department or call 911. 3. If his condition does not improve, or signs of right sided heart failure present, Patient will need to be admitted to the any local hospital for acute care management. 4. Schedule follow-up well visit for goal setting/ lifestyle modification counseling.