Major Basic Science Discoveries in HIV
advertisement

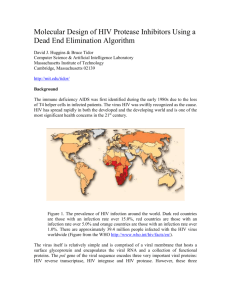
Major basic science discoveries in HIV Dr. Matthew Marsden, Ph.D. UCLA School of Medicine A new disease… On http://aids.gov/hiv-aids-basics/hiv-aids-101/aids-timeline/ A new disease… • By the end of 1981, there was a cumulative total of 270 reported cases of severe immune deficiency among gay men, and 121 of those individuals had died. • In 1983, Luc Montagnier and Françoise Barré-Sinoussi reported the discovery of a new virus (later called HIV) that is the cause of AIDS. • The first commercial blood test for HIV was licensed in 1985, allowing screening of the U.S. blood supply. • In 1987 the first anti-HIV drug (AZT) was approved by the U.S. Food and Drug Administration. • The first potent combination of anti-HIV drugs became available in 1995. On http://aids.gov/hiv-aids-basics/hiv-aids-101/aids-timeline/ Some Significant Historical Discoveries in the field of Retrovirology 1908- Discovery of Retroviruses in chickens (Ellermann and Bang). 1911- Cell free transmission of a sarcoma in chickens (Rous) named “Rous sarcoma virus”. Some Significant Historical Discoveries in the field of Retrovirology 1908- Discovery of Retroviruses in chickens (Ellermann and Bang). 1911- Cell free transmission of a sarcoma in chickens (Rous) named “Rous sarcoma virus”. Many additional retroviruses were subsequently identified in different animals, including important model systems: 1936- Mammary carcinoma in mice caused by milktransmitted, filterable agent (Bittner) termed “Mouse Mammary Tumor virus”. 1957- Potent leukemia virus isolated from mice (Gross) named “Gross murine leukemia virus”. Some Significant Historical Discoveries in the field of Retrovirology 1908- Discovery of Retroviruses in chickens (Ellermann and Bang). 1911- Cell free transmission of a sarcoma in chickens (Rous) named “Rous sarcoma virus”. Many additional retroviruses were subsequently identified in different animals, including important model systems: 1936- Mammary carcinoma in mice caused by milktransmitted, filterable agent (Bittner) termed “Mouse Mammary Tumor virus”. 1957- Potent leukemia virus isolated from mice (Gross) named “Gross murine leukemia virus”. 1957- Visna, a neurological disease in sheep caused by a lentivirus was described, giving rise to the concept of slow infections by these viruses (Latin: lentus, slow). 1980- 1st human retrovirus “Human T-cell leukemia virus 1” (HTLV-1) isolated. For more information see “Retroviruses” textbook chapter here: http://www.ncbi.nlm.nih.gov/books/NBK19403/ Timeline of discoveries 1970s: Discovery of retroviruses and retroviral enzymes 1970- Discovery of Reverse Transcriptase- Howard Temin and David Baltimore (Received 1975 Nobel Prize in Physiology or Medicine) “Central dogma” of molecular biology http://www.ncbi.nlm.nih.gov/Class/MLACourse/Modules/MolBioReview/central_dogma.html 1970- Discovery of Reverse Transcriptase- Howard Temin and David Baltimore (Received 1975 Nobel Prize in Physiology or Medicine) “Central dogma” of molecular biology However….. Reverse transcriptase catalyzes formation of DNA using an RNA template http://www.ncbi.nlm.nih.gov/Class/MLACourse/Modules/MolBioReview/central_dogma.html Timeline of discoveries 1970s: Discovery of retroviruses and retroviral enzymes 1981: Epidemic first identified 1983: Identification of the HIV virus 1983- Identification of the HIV virus- Françoise Barré-Sinoussi and Luc Montagnier (Shared 2008 Nobel Prize in Physiology or Medicine) http://www.nobelprize.org/nobel_prizes/medicine/laureates/2008/press.html Timeline of discoveries 1970s: Discovery of retroviruses and retroviral enzymes 1981: Epidemic first identified 1983: Identification of the HIV virus 1985: First commercial test to detect HIV 1987: First antiretroviral drug approved 1987- First antiretroviral drug approved (AZT; azidothymidine; zidovudine) Just 25 months from demonstrated efficacy in vitro (in a test tube) to FDA approval- Record time http://www.mcld.co.uk/hiv/?q=AZT 1987- First antiretroviral drug approved (AZT; azidothymidine; zidovudine) The nucleoside analog reverse transcriptase inhibitors (e.g. AZT) and non-nucleoside reverse transcriptase inhibitors (e.g. efavirenz) target this stage of the virus life cycle. Timeline of discoveries 1970s: Discovery of retroviruses and retroviral enzymes 1981: Epidemic first identified 1983: Identification of the HIV virus 1985: First commercial test to detect HIV 1987: First antiretroviral drug approved 1989: Crystallization of protease 1991: 2nd and 3rd anti-retrovirals approved 1995: Discovery of RANTES and MIP as suppressive factors 1995: Protease inhibitors approved 1989- Crystallization of protease enzyme (allowed rational design of protease inhibitors) 1995- Protease inhibitors approved for clinical use http://people.mbi.ucla.edu/yeates/153AH_2009_project/sriphanlop.html http://physiologyonline.physiology.org/content /26/4/236/F2.expansion.html 1989- Crystallization of protease enzyme (allowed rational design of protease inhibitors) 1995- Protease inhibitors approved for clinical use Protease inhibitors (e.g. Saquinavir) Timeline of discoveries 1970s: Discovery of retroviruses and retroviral enzymes 1981: Epidemic first identified 1983: Identification of the HIV virus 1985: First commercial test to detect HIV 1987: First antiretroviral drug approved 1989: Crystallization of protease 1991: 2nd and 3rd anti-retrovirals approved 1995: Discovery of RANTES and MIP as suppressive factors 1995: Protease inhibitors approved 1996: Discovery of CXCR4 and CCR5 co-receptors 1996- Discovery of the HIV coreceptors (CCR5 and CXCR4) 2007- Entry inhibitor approved based on this knowledge. http://www.thefullwiki.org/Discovery_and_development_of_CCR5_receptor_antagonists 1996- Discovery of the HIV coreceptors (CCR5 and CXCR4) 2007- Entry inhibitor approved based on this knowledge. Entry inhibitor (maraviroc) Timeline of discoveries 1970s: Discovery of retroviruses and retroviral enzymes 1981: Epidemic first identified 1983: Identification of the HIV virus 1985: First commercial test to detect HIV 1987: First antiretroviral drug approved 1989: Crystallization of protease 1991: 2nd and 3rd anti-retrovirals approved 1995: Discovery of RANTES and MIP as suppressive factors 1995: Protease inhibitors approved 1996: Discovery of CXCR4 and CCR5 co-receptors 1996: Discovery of protective effect of Δ32 CCR5 deletion 1997: Three-drug therapy (HAART) shown to delay progression 1997: Core structure of gp41 solved (6-helix bundle) 1997- Core structure of gp41 solved (6-helical bundle) 2003- Fusion inhibitor approved http://www.pnas.org/content/98/20/11187/F1.expansion.html 1997- Core structure of gp41 solved (6-helical bundle) 2003- Fusion inhibitor approved Fusion inhibitor (T-20, enfuvirtide) Timeline of discoveries 1970s: Discovery of retroviruses and retroviral enzymes 1981: Epidemic first identified 1983: Identification of the HIV virus 1985: First commercial test to detect HIV 1987: First antiretroviral drug approved 1989: Crystallization of protease 1991: 2nd and 3rd anti-retrovirals approved 1995: Discovery of RANTES and MIP as suppressive factors 1995: Protease inhibitors approved 1996: Discovery of CXCR4 and CCR5 co-receptors 1996: Discovery of protective effect of Δ32 CCR5 deletion 1997: Three-drug therapy (HAART) shown to delay progression 1997: Core structure of gp41 solved (6-helix bundle) 1997: Virus shown to persist in treated patients HIV persistence during therapy Short-lived infected cell Long-lived infected cell (latently infected) HIV persistence during therapy Antiretroviral therapy Short-lived infected cell Long-lived infected cell (latently infected) HIV persistence during therapy Short-lived infected cell Long-lived infected cell (latently infected) HIV persistence during therapy Antiretroviral therapy •Latently infected CD4+ T lymphocytes are rare in vivo: •Approximately 1 per 106 total resting CD4+ T cells •Probably constitute around 105-106 cells per patient Approximately 1 per million resting CD4+ T cells harbor a latent provirus. Rose Bowl Capacity = 92,542 Approximately 1 per million resting CD4+ T cells harbor a latent provirus. Rose Bowl Capacity = 92,542 Like finding one person in 11 football stadiums. To cure the infection we need to do this with 1,000,000 (one million) cells hidden in this way. Activation/elimination strategy for clearing latently-infected cells: Marsden and Zack (2010) Future Virol. 5(1): 97–109. Prostratin is a phorbol ester isolated from the Samoan medicinal plant Homalanthus nutans (and previously from Pimelea prostrata) Pimelea prostrata © 1991 Kennedy Harris Homalanthus nutans (Mamala Tree) http://members.ozemail.com.au/~pete rrjones/plants/f.html Traditionally used in treatment of jaundice and hepatitis http://www.berkeley.edu/news/ media/releases/2004/09/29_sa moa.shtml U1 cell latency assay: Add PKC agonist Assay p24 concentration in supernatant 2 days Bugula neritina Bryostatin 1: •First isolated from Bugula neritina. •Modulates PKC activity. •Shows potential as an anti-cancer therapeutic •Has been shown to inhibit tumor invasion, tumor growth in vitro and in vivo, and angiogenesis. http://www.marine.csiro.au •In various phase 1 and phase 2 clinical trials for treatment of cancer. •Previously was very difficult to obtain and hard to modify to alter activity. Bryostatin 1 -Publication involves 7 bryostatin analogs (bryologs). -These can be synthesized for several thousand dollars/gram (rather than 1 million). -Can be modified according to need. -Activate latent HIV expression more efficiently in vitro (cell lines). J-Lat 10.6 latency assay: Add latency activating agent 48 hours Timeline of discoveries 1970s: Discovery of retroviruses and retroviral enzymes 1981: Epidemic first identified 1983: Identification of the HIV virus 1985: First commercial test to detect HIV 1987: First antiretroviral drug approved 1989: Crystallization of protease 1991: 2nd and 3rd anti-retrovirals approved 1995: Discovery of RANTES and MIP as suppressive factors 1995: Protease inhibitors approved 1996: Discovery of CXCR4 and CCR5 co-receptors 1996: Discovery of protective effect of Δ32 CCR5 deletion 1997: Three-drug therapy (HAART) shown to delay progression 1997: Core structure of gp41 solved (6-helix bundle) 1997: Virus shown to persist in treated patients 1998: First non-nucleoside RT inhibitor approved 2003: Fusion inhibitor approved 2003: Restriction factors, TRIM5α and APOBEC3G, identified 2007: Integrase inhibitor approved 2007- Integrase inhibitor approved Raltegravir http://www.prn.org/index.php/management/article/integrase_inhibitors_raltegravir_elvitegravir_hiv_disease_478 2007- Integrase inhibitor approved Integrase inhibitor (e.g. raltegravir) Movie of the HIV Life Cycle http://www.youtube.com/watch?v=9leO28ydyfU Timeline of discoveries 1970s: Discovery of retroviruses and retroviral enzymes 1981: Epidemic first identified 1983: Identification of the HIV virus 1985: First commercial test to detect HIV 1987: First antiretroviral drug approved 1989: Crystallization of protease 1991: 2nd and 3rd anti-retrovirals approved 1995: Discovery of RANTES and MIP as suppressive factors 1995: Protease inhibitors approved 1996: Discovery of CXCR4 and CCR5 co-receptors 1996: Discovery of protective effect of Δ32 CCR5 deletion 1997: Three-drug therapy (HAART) shown to delay progression 1997: Core structure of gp41 solved (6-helix bundle) 1997: Virus shown to persist in treated patients 1998: First non-nucleoside RT inhibitor approved 2003: Fusion inhibitor approved 2003: Restriction factors, TRIM5α and APOBEC3G, identified 2007: Integrase inhibitor approved 2007: Entry inhibitor approved (Maraviroc) 2008: Discovery of Tetherin 2008: Transplant of infected subject with Δ32 donor stem cells http://www.nytimes.com/2011/11/29/health/new-hope-of-a-cure-for-hiv.html?pagewanted=all HIV enters cells by binding to CD4 and a “corecepter” (often CCR5). CCR5 is not functional in approximately 1% of Caucasians, which means they are highly resistant (but not completely immune) to infection with most strains of HIV. This mutation is called CCR532. http://www.thefullwiki.org/Discovery_and_development_of_CCR5_receptor_antagonists • The “Berlin Patient” was HIV positive and also developed leukemia. • He underwent aggressive chemotherapy to clear the leukemia, and in the process almost all the HIV+ cells in his body were also killed. • This patient then received two bone marrow transplants from a CCR5-32 individual. • The new immune cells were not susceptible HIV, and the virus in currently undetectable more than four years post-transplant. Cells of the Immune System Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Dendritic cell CD4+ T cell CD8+ T cell B lymphocyte Natural killer cell Modified from : http://www.cancer.gov/cancertopics/understandingcancer/immunesystem Cells of the Immune System Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Dendritic cell CD4+ T cell CD8+ T cell B lymphocyte Natural killer cell Modified from : http://www.cancer.gov/cancertopics/understandingcancer/immunesystem Cells of the Immune System Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Dendritic cell CD4+ T cell CD8+ T cell B lymphocyte Natural killer cell Modified from : http://www.cancer.gov/cancertopics/understandingcancer/immunesystem Cells of the Immune System Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Dendritic cell CD4+ T cell CD8+ T cell B lymphocyte Natural killer cell Modified from : http://www.cancer.gov/cancertopics/understandingcancer/immunesystem Cells of the Immune System Macrophage Marrow Mast cell Eosinophil Erythrocytes Basophil Monocyte Bone Megakaryocyte Hematopoietic stem cell CCR5-32 Multipotential stem cell Myeloid progenitor Neutrophil cell Platelets Lymphoid progenitor cell T lymphocyte Dendritic cell CD4+ T cell CD8+ T cell B lymphocyte Natural killer cell Modified from : http://www.cancer.gov/cancertopics/understandingcancer/immunesystem Why can’t we use this approach for everybody? • The chemotherapy and bone marrow transplant procedure was very risky (the patient nearly died). • Matching donors that are also CCR5-32 are very hard to find. • The procedure is very expensive, time consuming, and requires excellent medical facilities (not feasible in many parts of the world) . • The patient will have to take immunosuppressive drugs for the rest of their life to avoid problems with the transplant (this may be worse than just taking the anti-HIV drugs). Timeline of discoveries 1970s: Discovery of retroviruses and retroviral enzymes 1981: Epidemic first identified 1983: Identification of the HIV virus 1985: First commercial test to detect HIV 1987: First antiretroviral drug approved 1989: Crystallization of protease 1991: 2nd and 3rd anti-retrovirals approved 1995: Discovery of RANTES and MIP as suppressive factors 1995: Protease inhibitors approved 1996: Discovery of CXCR4 and CCR5 co-receptors 1996: Discovery of protective effect of Δ32 CCR5 deletion 1997: Three-drug therapy (HAART) shown to delay progression 1997: Core structure of gp41 solved (6-helix bundle) 1997: Virus shown to persist in treated patients 1998: First non-nucleoside RT inhibitor approved 2003: Fusion inhibitor approved 2003: Restriction factors, TRIM5α and APOBEC3G, identified 2007: Integrase inhibitor approved 2007: Entry inhibitor approved (Maraviroc) 2008: Discovery of Tetherin 2008: Transplant of infected subject with Δ32 donor stem cells Thank you for your attention! Questions?