Approach to Abdominal pain in children
advertisement

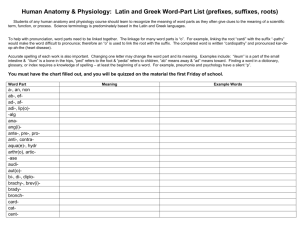
What is the problem? 11/9/2015 ped.emergency.Dr.Alsaif 1 Approach to Abdominal pain in children Ibrahim Alsaif Pediatric Emergency Consultant Al-Yamamah Hospital 11/9/2015 ped.emergency.Dr.Alsaif 2 Goals and Objectives Be Systematic Evaluate then identify the problem then intervene. Anatomic and Path physiology of pain Is the pain acute or chronic? Causes of pain Approach to reach the diagnosis Red flags Indications for Surgical consultation. 11/9/2015 ped.emergency.Dr.Alsaif 3 Systematic Approach to a sick child Initial impression (appearance, work of breathing, circulation) Is the child need Resuscitation(CPR)? Yes No C A B Evaluate • Primary assessment (ABCDE approach) • Secondary assessment (focused H&P) • Diagnostic tests Intervene Identify 11/9/2015 ped.emergency.Dr.Alsaif 4 What is the abdominal pain? Abdominal pain is a common complaint in all settings of medical practice. Pain may be a symptom of a severe, lifethreatening disease or Of a benign underlying condition. 11/9/2015 ped.emergency.Dr.Alsaif 5 Anatomic origin of pain The classic division of abdomen: 11/9/2015 ped.emergency.Dr.Alsaif 6 Anatomic origin of pain Abdomen is divided into 9 regions: 2 vertical lines (RT&LT midclavicular) 2 horizontal lines (subcostal and intertubercular) 11/9/2015 ped.emergency.Dr.Alsaif 7 Pathophysiology Types of pain Visceral pain: Due to irritation of visceral peritonium Dull Poorly localized Usually periumbilical 11/9/2015 ped.emergency.Dr.Alsaif 8 Pathophysiology Parietal (somatic) pain: Due to irritation of parietal peritonium Sharp Intense Discrete localized Aggravated by coughing or movement 11/9/2015 ped.emergency.Dr.Alsaif 9 Pathophysiology Referred pain: Same feature as parietal. It results from shared central pathways for afferent neurons from different sites. The classic example is pneumonia (the T9 dermatome distribution is shared by the lung and the abdomen). 11/9/2015 ped.emergency.Dr.Alsaif 10 Is the pain acute or chronic? Acute abdominal pain: A sudden, severe abdominal pain of unclear cause lasts less than one week. chronic abdominal pain: Intermittent or constant abdominal pain (of functional or organic etiology) last for at least two months Chronic abdominal pain occur in 10 to 20 % of children. 11/9/2015 ped.emergency.Dr.Alsaif 11 Is the pain acute or chronic? Chronic abdominal pain classically defined by four criteria: ≥3 episodes of abdominal pain Pain sufficiently severe to affect activities Episodes occur over a period of ≥2 months No known organic cause. 11/9/2015 ped.emergency.Dr.Alsaif 12 Causes of abdominal pain Age is a key factor in the evaluation of abdominal pain. 11/9/2015 ped.emergency.Dr.Alsaif 13 11/9/2015 ped.emergency.Dr.Alsaif 14 Causes 11/9/2015 ped.emergency.Dr.Alsaif 15 Approach to reach the diagnosis In fact: Based on history and a physical exam alone, physicians were able to correctly differentiate between organic and nonorganic causes of abdominal pain nearly 80% of the time. 11/9/2015 ped.emergency.Dr.Alsaif 16 History Place/Location ask child to use one finger to locate the pain. Quality: pain can be a sharp stabbing pain (i.e. trauma) or diffuse, poorly, localized pain (i.e. chronic or visceral pain). Radiation: pain can radiate from its point of origin in any direction. Severity: degree of pain on a scale of 10 Timing/Onset: onset of the pain, duration of pain, course during the day, does it wake them at night, and the frequency of episodes. 11/9/2015 ped.emergency.Dr.Alsaif 17 History Alleviating Factors: Anything that reduces the pain like body position, movements ,medications. Aggravating Factors: Anything that increases the pain like body position, movements, relation to food intake. Associated Symptoms: Hematemesis, vomiting, nausea, melena, diarrhea, fever, and weight loss. 11/9/2015 ped.emergency.Dr.Alsaif 18 Associated symptoms for abdominal pain Associated Symptom Relevance Diarrhea Gastroenteritis, Protein losing enteropathy Bloody stool Ulcerative colitis, necrotizing enterocolitis, dysentery, constipation Hematemesis Peptic Ulcer Disease, Gastritis Bilious emesis Small bowel obstruction Jaundice Hepatitis or Biliary obstruction Joint pain/swelling IBD, HSP Skin Lesions IBD, HSP, Liver disease Testicular pain Testicular torsion Dysuria/polyuria/hematuria Urinary tract infection/Pyelonephritis Vaginal/Penile discharge STI Dysmenorrhea Endometriosis Shortness of breath Pneumonia or empyema 19 History Ask about: Bowel movement patterns and stool quality (size, hard/soft, odour). Ingestion of toxin or foreign object accidental or non-accidental trauma. Dietary history: in young children, too much milk can lead to constipation. 11/9/2015 ped.emergency.Dr.Alsaif 20 History Ask about: Past medical history and medical illness: Cystic fibrosis predisposes to gallstones. Spina bifida/cerebral palsy/developmental delay predisposes to constipation. Sickle cell disease predisposes to splenic autoinfarction. Recurrent respiratory tract infections suggest mesenteric adenitis. 11/9/2015 ped.emergency.Dr.Alsaif 21 History Ask about: Family medical history, especially inflammatory bowel disease. Travel history, social and psychiatric (potential stressors) history. 11/9/2015 ped.emergency.Dr.Alsaif 22 Physical exam General exam: ABCDE Including vital signs and growth parameters, is there evidence of failure to thrive?. Inspection: Iook for contour, symmetry, pulsations, peristalsis, skin markings, wall protrusions (hernias), any signs of trauma (ie. bruising, swelling), and abdominal distension. 11/9/2015 ped.emergency.Dr.Alsaif 23 Physical exam Auscultation: Auscultate before palpation in the abdominal exam. Iisten for bowel sounds, abdominal bruits. Pressure of the stethoscope also tests for tenderness. Percussion: (tympanic vs non-tympanic). Percuss for liver span and spleen tip. Assess for ascites. 11/9/2015 ped.emergency.Dr.Alsaif 24 Physical exam Palpation: Tenderness with light and deep palpation. Guarding and rebound tenderness Palpate for liver, spleen, kidney and abdominal masses (including fecal mass). 11/9/2015 ped.emergency.Dr.Alsaif 25 Physical exam Digital rectal exam: First exam the anus for fissures and skin tags. Then assess for tone, stool, and blood. Special Tests: There are a number of special tests for each differential diagnosis. 11/9/2015 ped.emergency.Dr.Alsaif 26 findings on physical exam for common differential diagnoses Medical Condition Findings on Physical Exam Constipation Abdominal tenderness, palpable fecal mass, look for imperforate anus or stenosis, spina bifida, developmental delay, cerebral palsy Acute appendicitis Patient avoids movement, rebound tenderness, McBurney sign (pain at 2/3 between umbilicus and right ASIS), Rovsing sign (pain in right lower quadrant on left-sided palpation), Psoas sign (pain in right lower quadrant when child on left and right hip hyperextended), obturator sign (pain in right lower quadrant on internal rotation of flexed right thigh) Gastroenteritis Diffuse pain with no rebound tenderness, abdominal distension, hyperactive bowel sounds Irritable bowel syndrome Periumbilical tenderness, no rebound tenderness Trauma Signs of bruising and tenderness Celiac Disease Growth failure, distended abdomen, diffuse abdominal tenderness. Inflammatory bowel disease Appears thin, abdominal tenderness, anal skin tags, possible sign of bloody stool on DRE, examine for skin lesions (erythema nodosum, pyoderma gangrenosum), iritis, and joint inflammation Urinary tract infection Fever, suprapubic and costovertebral angle tenderness, irritability, foulsmeling urine, gross hematuria Primary dysmenorrhea Lower abdominal tenderness Pneumonia and Empyema Tachypnea, cyanosis, decreased breath sounds, crackles and rales, dullness on percussion, febrile Associated Signs Jaundice suggests hemolysis or liver disease. Pallor and jaundice point to sickle cell crisis. Psoas & Obturator test If positive: Inflamed retrocecal appendix Ruptured appendix or Iliopsoas abscess. 11/9/2015 ped.emergency.Dr.Alsaif 28 Associated Signs Murphy's sign: (interruption of deep inspiration by pain when the physician's fingers are pressed beneath the right costal margin). Suggests acute cholecystitis. 11/9/2015 ped.emergency.Dr.Alsaif 29 Associated Signs Cullen's sign (bluish umbilicus) Grey Turner's sign (discoloration in the flank) Unusual signs of internal hemorrhage. 11/9/2015 ped.emergency.Dr.Alsaif 30 Associated Signs Purpura and arthritis: Henoch-Schönlein purpura 11/9/2015 ped.emergency.Dr.Alsaif 31 Uncommon differential diagnoses and potential complications Medical Condition Relevant Findings and Potential Complications Intussusception Colicky pain, flexing of legs, fever, lethargy, vomiting, peak incidence in children at 6 months of age Mekel’s diverticulum Similar presentation to appendicitis, profuse GI bleeding, can develop to diverticulitis Mesenteric adenitis Can present like acute appendicitis, recurrent respiratory tract infections Hirschsprung disease Vomiting, abdominal distension, enterocolitis, primarily in first year of life Small bowel obstruction Bloating, vomiting, failure to pass flatus or stool, bilious emesis Volvulus Can present like small bowel obstruction, due to intestinal twisting Large bowel obstruction Abdominal distension, hard feces and rectal bleeding, can lead to bowel perforation Necrotizing enterocolitis Feeding intolerance, apnea, lethargy, bloody stools, abdominal distension and tenderness, abdominal erythema, bradycardiac, primarily in premature infants Peptic ulcer disease Epigastric tenderness, pain related to eating a meal, ulcer can perforate Viral hepatitis Fever, malaise and jaundice, consider fecal-oral or vertical transmission Acute pancreatitis Steady and sudden-onset pain radiating to the back, nausea, vomiting Splenic infarction Personal or family history of sickle cell disease Nephrolithiasis Acute renal colic, flank pain radiating to groin Testicular torsion Testicular pain with acute onset, nausea, vomiting Laboratory investigations for common differential diagnoses Medical Condition Relevant Diagnostic Tests Constipation None if history does not suggest an alternative diagnosis. Acute appendicitis CBC (WBC normal or elevated), urinalysis, urine pregnancy Gastroenteritis Serum electrolytes, stool culture, stool for virology Irritable bowel syndrome None, based on history and clinical findings Trauma CBC for blood loss, abdominal CT with contrast Celiac Disease IgA Inflammatory Bowel Disease CBC, ESR/CRP, electrolytes, albumin, LFTs, Bilirubin, Stool culture, AXR Urinary tract infection Urine dipstick (for leukocyte esterase and nitrite), urine microscopy, urine culture (best if suprapubic aspirate) Primary dysmenorrhea None, based on history and clinical findings Pneumonia and Empyema CBC, Chest x-ray, sputum culture 33 Red flags in abdominal pain Certain historical and examination findings should raise ‘‘red flags’’ that a severe lifethreatening underlying abdominal process is present and prompt early triage to an emergency department. 11/9/2015 ped.emergency.Dr.Alsaif 34 Red flags in abdominal pain History Inability to maintain po intake Projectile vomiting Overt gastrointestinal blood loss Syncope Pregnancy Recent surgery or endoscopic procedure Fever Caustic or foreign body ingestion 11/9/2015 ped.emergency.Dr.Alsaif 35 Red flags in abdominal pain Physical examination Pathologic changes in vital signs Bloody, melenic stool Hernia (incarcerated and tender) Hypoxia Cyanosis Change in level of consciousness Jaundice Peritoneal signs Abdominal pain out of proportion to examination 11/9/2015 ped.emergency.Dr.Alsaif 36 Red flags in abdominal pain Laboratory results Renal failure Metabolic acidosis Leukocytosis Elevated transaminases Elevated alkaline phosphatase and bilirubin Anemia or polycythemia Hyperlipasemia/hyperamylasemia Hyperglycemia/hypoglycemia 11/9/2015 ped.emergency.Dr.Alsaif 37 Red flags in abdominal pain Radiography Abdominal free air Gallbladder wall thickening Pericholecystic fluid Dilated biliary tree Bowel obstruction Dilated small bowel loops ± air fluid levels Intra-abdominal abscess Bowel wall thickening Air in the portal venous system Pneumatosis intestinalis 11/9/2015 ped.emergency.Dr.Alsaif 38 Indications for Surgical Consultations Severe or increasing abdominal pain with progressive signs of deterioration Bile-stained or feculent vomitus Involuntary abdominal guarding/rigidity Rebound abdominal tenderness Marked abdominal distension with diffuse tympany Signs of acute fluid or blood loss into the abdomen Significant abdominal trauma Suspected surgical cause for the pain Abdominal pain without an obvious etiology 11/9/2015 ped.emergency.Dr.Alsaif 39 11/9/2015 ped.emergency.Dr.Alsaif 40 Any question ? 11/9/2015 ped.emergency.Dr.Alsaif 41