Management Statement 1 - Asia Pacific Working Group in
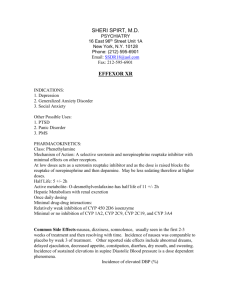
advertisement

Asia Pacific Consensus on Crohn’s disease Statements on Management Aims in Mx of a patient with CD Symptoms and signs Weight Clinical remission DOES NOT DETERMINE CLINICAL COURSE INFLAMMATORY PARAMETERS CRP IL-6 Faecal calprotectin Faecal lactoferrin Platelet Inflammation remissoin STRUCTURAL PARAMETERS Endoscoy MRI CT Intestinal healing INFLUENCE CLINICAL COURSE Management Statement 1 • Induction of remission is usually a symptomatic end point although increasingly, endoscopic mucosal healing is considered an important objective sign of therapeutic efficacy. • Normalisation of inflammatory biomarkers including C-reactive protein and faecal calprotectin are other objective endpoints of therapeutic efficacy. • Other goals of treatment include maintenance of the disease in the remission phase, and prevention of strictures and fistulae. Population based studies: Follow –up data on natural history of adult CD worldwide Country Location No of incident CD Inclusion Median duration of FU USA Olmsted County 314 1940-2004 14 years Canada Manitoba 4,193 April 1984-March 2003 N/A Denmark Copenhagen County 641 1962-1987; 1991- 17, 10 and 1 1993; 2003-2004 year for the (three cohorts) three cohort respectively 237 January 1990 to December 1993 124 mo (range, 108-144 mo) Norway (IBSEN) Sweden Stockholm County 20,120 1954-2000 N/A 7 European countries and Israel European collaborative Study Group on IBD 365 1991-2004 10.3 years (range, 9.4-11 years) Natural History of CD • Natural behaviour: Remissions and relapses – Most patients need to take medication for a large period of their life, mostly for maintenance of remission and intermittently additional induction therapy • Population-based data from Denmark:1st yr after diagnosis, – 55 % are in remission – 15% have mild disease – 35% have highly active disease. • Similar data from Olmsted County, US – > Two-thirds (64.4%): Medical or surgical remission – One third active disease Activity of disease in previous yr predicts the course in subsequent yrs. A full year of remission is followed by an 80% chance of remission in following year, A recent flare only has a 30% chance of remission in the following year. Natural History of CD • Disease extent: – Ileocolonic: 40–50% – Isolated small intestine: 30% – Pure colonic: 30% • Changes in location of disease is minimal – Only 10-15% show changes in localization 10 yrs after diagnosis. • Change in Behaviour: More frequent as disease becomes older – At presentation: Majority (90%) have inflammatory, (nonstricturing, non-penetrating disease – With longer follow up: Development of either a stricture or a fistula increases Evolution of Disease Behavior in CD Cumulative Probability (%) 100 90 80 70 Penetrating 60 50 40 Inflammatory 30 20 10 0 0 12 24 36 48 60 72 84 96 108 120 132 144 156 168 180 192 204 216 228 240 Months Patients at risk: N= 2002 552 229 95 37 Cosnes J et al. Inflamm Bowel Dis. 2002;8:244. Cumulative risk of hospitalization in Olmsted County, in the pre-biological era: 211 diagnosed between Jan 1970 -June 1997 and followed until June 1997 Cumulative risk of intestinal resection 314 pts with CD from Olmsted County, diagnosed between 1940-2001 Natural history of a pt with CD: Predicted course based on Markov Model • A representative patient spends • Lifetime disease course – – – – – – – 24% in medical remission 27% as mild disease: 1% with severe drug-responsive disease, 4% with severe drug-dependent disease, 2% with severe drug-refractory disease, 1% in surgery, 41% in post surgical remission • Over time, – Decreasing in proportion of medical remission state – Increase in proportion post-surgical remission state; CD is a progressive disease Predictors of natural history in adult Crohn’s disease Variable Comment Clinical Risk factors Age <40 years at diagnosis, Need for systemic steroids for first flare, Perianal disease Terminal ileal disease C-reactive protein Endoscopic factors Mucosal healing Mx: Statement 1 • Induction of remission is usually a symptomatic end point although increasingly, endoscopic mucosal healing is considered an important objective sign of therapeutic efficacy. • Normalisation of inflammatory biomarkers including C-reactive protein and faecal calprotectin are other objective endpoints of therapeutic efficacy. • Other goals of treatment include maintenance of the disease in the remission phase, and prevention of strictures and fistulae. Mucosal healing predicts better outcome Population study • Norwegian population-based study: 141 CD Pts – Endoscopic re-evaluation within 0.5 and 2 yrs after diagnosis, – 50 evaluated 5 yrs after diagnosis – Mucosal healing at base line was associated with less endoscopic disease activity at 5 years – Decreased need for subsequent treatment with steroid • In UC: Mucosal healing after 1 yr of T/T strongly predictive of less surgery • Discrepancies between UC and CD – CD is a transmural disease, – UC: predominantly mucosal Mucosa healing Complication of CD: Deep ulcer, fistula, stricture If mucosa heal : such complications decrease Recurrence in post op Endoscopy at 1 year Mild lesion Advanced lesion Recur over 5-10 yrs <10% >90% Mucosal healing : less hospitalization/ surgical intervention Rutgeert’s Gastroenterology 1990 • Mucosal healing appears to be an ideal end point for assessment Non invasive marker may be used to determine activity in IBD Acute phase ESR, CRP, Orosomucoid, Platelet count reactants Serological tests ASCA, pANCA, Lactoferrin, fibrinogen Cytokines Interleukins (IL-1,IL-2,IL-6,IL-8,IL-10,IL-15)TNF-α Faecal Indium labeled white cells, calprotectin, lactoferrin, Nitric oxide, α-antitrypsin excretion, lysozyme excretion Others Indium labeled white cells scan, Intestinal permeability test, whole gut lavage fluid for immunoglobulin and albumin C-reactive protein as a predictor for disease activity and natural course • CRP: acute phase protein, synthesized in liver in response to stimulation by IL-6, TNF α, and IL-1β, and is produced at site of inflammation. • Functions as an opsonin for bacterial sequences and nuclear material expressed during apoptosis. • Half life of CRP is small (19 Hrs), – Concentration decreases once acute phase stimulus disappears. C-reactive protein as a predictor for disease activity and natural course • CRP: Only biological parameter, identified as predictor of a more severe clinical course of CD • Norwegian population-based study: 176 CD – CRP levels measured at diagnosis, after 1 and 5 yrs • At diagnosis: Mean CRP was 51 mg/L (>>than in UC) – At 1 yr: Significant decrease from 51 to 16 mg/L – Significant association between CRP levels at diagnosis and risk of surgery in next 5 yrs – In those with L1 disease, the risk of surgery increased by a factor of six when CRP levels were above 53 mg/1 MANAGEMENT 1) Induction of remission is usually a symptomatic endpoint although increasingly, endoscopic mucosal healing is considered an important objective sign of therapeutic efficacy. Normalisation of inflammatory biomarkers including C-reactive protein and faecal calprotectin are other endpoints. Other goals of treatment include keeping of the disease in remission, and prevention of strictures and fistulae. Comments: •What are we trying to say? •Statement is too complex •Too many substatements here will make the voting difficult •Should we add a word or two about "quality of life"? •Too many parameters in this statement. Revised Mx: Statement 1 • The goals of treatment include :induction and maintenance of remission, prevention of strictures, fistulae and other complications and improving quality of life. Revised Mx: Statement 1 • Induction of remission is usually a symptomatic endpoint though increasingly endoscopic mucosal healing is considered an important objective sign of therapeutic efficacy.( goes to text) • Normalisation of inflammatory biomarkers including C-reactive protein and faecal calprotectin are other objective endpoints of therapeutic efficacy. (EL 3, RG C) Mx: Statement 2 • All patients with CD should be assessed for the extent of the disease, activity of the disease and their behaviour should also be assessed. Treatment of CD depends upon extent of the disease, behaviour of the disease and activity of the disease Phenotype of CD Montreal classification Age of onset ≤ 16 yrs (A1) Location lleal (L1) Behavior Non- stricturing, Nonpenetrating (B1) Stricturing (B2) 17- 40 yrs (A2) Colonic (L2) > 40 yrs (A3) lleal-colonic (L4) lsolated UGI (L4) Penetrating (B3) + ‘p’ if peri-anal disease CD: Activity scoring system Ulcerative colitis Truelove and Witts (1955) Crohn’s disease Crohn’s Disease Activity Index (Best WR, 1979) Powell-Tuck (1978) Harvey and Bradshaw(1980) Complex clinical activity score, Oxford criteria (Myren J, 1984) (Seo, 1995) Simple clinical colitis index (Walsemy, 1998) Mayo index (Riley SA, 1991) Crohn’s Disease Activity Index Item(day) No. liquid or very soft stools(each day for 7days) Abdominal pain, sum of 7 d rating (0=none,1=mild,2=moderate,3=severe) General well being (1-4) Exteraintestinal (1 per finding) Arthritis/arthralgia Mucocutaneous lesion Iritis/uveitis Anal disease (fissure, fistula,etc) External fistula Fever>36.8 Antidiarrheal use Abdomial mass(none-0,equivocal-2,definite-5 Hematocrit (males-47) (Females-42) Bodyweight (1-body weight/standard weight) ×100 Total CDAI Score Weight ×2 ×5 ×7 ×20 ×30 ×10 ×6 ×1 Harvey Bradshaw index Variable General well being Abdominal pain No. of liquid stools Abdominal mass Complications Variable description 0= very well, 1=slightly poor, 2 =poor, 3= very poor, 4= terrible 0=none 1=mild 2=moderate 3=severe Daily 0=none 1=dubious 2=definite 3=definite and tender) Arthralgia, Uveitis, Erythema nodosum, aphthous ulcer, pyoderma gangrenosum, Anal fissure, New fistula Assessment of perianal CD activity index Catogries affected by fistula Discharge Pain/restriction of activities Restriction of sexual activity Type of Perianal disease Frequency No discharge Score 0 Minimal mucus discharge Moderate mucous or purulent discharge Substantial discharge Gross fecal soiling No activity restriction Mild-discomfort, no restriction Moderate discomfort, some limitation of activities Marked discomfort, marked limitation Severe pain, severe limitation No restriction of sexual activity Slight restriction of sexual activity Moderate limitation of sexual activity Marked limitation of sexual activity Unable to engage in sexual activity No perianal disease/skin tags Anal fissure or mucosal tear <3Perianal fistulae >3 Perianal fistulae 1 2 3 4 0 1 2 3 4 0 1 2 3 4 0 1 2 3 4 Anal sphincter ulceration or fistulae with significant undermining skin Degree of indurations No induration Minimal induration Moderate induration Substantial induration Gross fluctuance /abscess 0 1 2 3 4 Fistula activity score Endpoint Definition Improvement Closure of individual fistulas defined as no fistula drainage despite gentle finger compression. Improvement defined as a decrease from baseline in the number of opening draining fistulas of >50%for at least consecutive visits (i.e., at least 4 weeks.) Remission Remission defined as closure of all fistulas that were draining at baseline for at least 2 consecutive visits (i.e., at least 4 weeks.) Crohn’s disease Endoscopic index for severity index Number of recto-colonic segments, that deep ulceration are seen in divided by no. Sigmoid of segment examined Rectum Transverse colon Right colon Ileum Number of rectocolonic segments, that superficial ulceration are seen in divided by no. Sigmoid of segment examined Rectum Transverse colon Right colon Ileum Segmental surfaces involved by disease. The degree of disease involvement in each segment is determined by examining each segment for the following 9 lesions,(Pseudopolyps, healed ulcers, frank-erythema, frank-mucosal-swelling, aphthoid ulcers, superficial ulcer, deep ulcer, non nucleated stenosis, ulcerated stenosis) and estimating the no. of cm of involvement (1 or more lesion present) in a representative 10 cm portion from each segment. The average segmental surface involved by disease is calculated by dividing the sum of each of individual segmental surfaces involved by disease by the no. of segments examined. Segmental surfaces involved by ulcerations. The degree of ulceration in each segment is determined by examine each segment for ulceration (aphthoid ulcers, superficial ulcers, deep ulcers, ulcerated stenosis) and estimating the number of cm of intestine involved by ulceration in a representative 10 cm portion from each segment. The average segmental surface involved by ulceration is calculated by dividing the sum of each of individual segmental surfaces involved by ulceration by the no. of segments examined. Presence of non ulcerated stenosis in any of segments examined. Presence of ulcerated stenosis in any of segments examined. 12 6 1 1 3 3 Endoscopic scoring system for postop recurrence (Rutgeerts score) Grade Endoscopic Findings 0 No lesions in distal ileum 1 <5 Aphthous lesion 2 >5 Aphthous lesion with normal mucosa between lesions or skip areas of larger lesion lesions confined to ileocolonic anastomosis (i.e.<1cm in length) 3 Diffuse Aphthous ileitis with diffusely inflamed mucosa 4 Diffuse inflammation with already larger ulcers, nodules and/or narrowing Histological Disease activity in CD Histological finding Score Epithelial damage 0: Normal 1: Focal pathology 2: Extensive pathology 0: Normal 1: Moderately disturbed (<50%) 2: Severely disturbed (>50%) 0: Normal 1: Moderately increase 2: Severely increase 0: Normal 1: Moderately increase 2: Severely increase 1: In surface of epithelium 2: Cryptitis 3: Crypt abscess 0:No 1:Yes 0:No 1:Yes 0: None (0-6) 1: <33% (1 or 2-6) 2: 33%-66% (3 or 4-6) 3: >66% (5 or 6 of 6) Architectural changes Infiltration of mononuclear cells in the lamina propria Polymorphonuclear cells in lamina propria Polymorphonuclear cells in epithelium Presence of erosions and ulcers Presence of granuloma No. of biopsy specimens affected Treatment will depend on phenotype of CD Age of onset ≤ 16 yrs (A1) Location lleal (L1) Behavior Non- stricturing, Nonpenetrating (B1) Stricturing (B2) 17- 40 yrs (A2) Colonic (L2) > 40 yrs (A3) lleal-colonic (L4) lsolated UGI (L4) Penetrating (B3) Rx will depend upon Phenotype of CD and activity Age of onset ≤ 16 yrs (A1) Location lleal (L1) Behavior Non- stricturing, Nonpenetrating (B1) Stricturing (B2) 17- 40 yrs (A2) Colonic (L2) > 40 yrs (A3) lleal-colonic (L4) lsolated UGI (L4) Penetrating (B3) Activity of the disease 2) All patients with CD should be assessed for the extent of the disease, activity of the disease and their behaviour should also be assessed. Treatment of CD depends upon extent of the disease, behaviour of the disease and activity of the disease. Comments: •Yes exept assessing the upper GI tract and small bowel is not indicated in all patients •We should evaluate "high risk patients". (i.e, young age onset, anal lesion, etc) •"When should there be assessed? •Double-barrelled statement " Conventional Mx: Statement 2 • All patients with CD should be assessed for the extent of the disease, activity of the disease and their behaviour should also be assessed. ( bury in subtext) • Treatment of CD depends upon extent of the disease, behaviour of the disease and activity of the disease EL 3, RG C Drugs for CD Induction of remission SSZ (site specific) Mesalamines (site specific) Conventional steroids Budesonide (Site specific) Immunosuppressants Biologics Maintenance of remission Induction Mx: Statement 3 • Mild to moderately active CD involving terminal ileum (L1) or localised ileocaecal disease should be treated with budesonide. Conventional steroids should be used if budesonide is unavailable or failure of response. IA • For severe disease: conventional corticosteroids is the initial treatment of choice. [IA] Surgical resection [III-C] and anti-TNF are alternatives [IIIC]. Induction Mx: Statement 4 • Sulphasalazine can be used for mild CD limited to the colon. [IA] • There is no evidence of efficacy of mesalazine. [IA] • Moderately severe or severe colonic disease should be treated with conventional corticosteroids. [IA] Induction Mx: Statement 5 • For extensive small intestinal disease, patients should be treated with conventional corticosteroids. [III-C] • Alternative include anti-TNF agent and surgery. [III-C] Induction Mx: Statement 6 • For ileocolonic disease (L3), patients should be treated with conventional corticosteroids. [I-A] • Alternative include anti-TNF agent and surgery. [III-C] Rise of aminosalicytes in CD • Prototypic 5-ASA: SSZ, used to treat CD for > 40 yrs. • Late 1970s: 2 large multicenter RCTs showed SSZ marginally superior to placebo for induction of remission in active disease. – National Cooperative Crohn’s Disease Study – European Cooperative Crohn’s Disease Study • Remission rates: 40% in SSZ vs (30% in placebo) – Problem: Side-effects • Azad Kahn: 5-ASA is active component of SPS. – Newer formulations of 5-ASA were developed without sulfa • This innovation facilitated adm of higher doses of 5-ASA with better tolerability and less side effects Rise of aminosalicytes in IBD • Initial studies of various 5-ASA formulations: equivocal results • Singleton et al, 1993: 16-week trial Pentasa CD Study Group: had a profound effect on clinical practice. • In this dose-finding trial evaluated 310 patients for 16 wks, • Primary outcome: Change in CDAI from baseline to final visit. • Remission rates – Placebo: 18% – Pentasa 1gm:23% Controlled-release mesalamine prep: safe and effective – Pentase 2 gm:24% at 4–g/day in 4gm: active CD(Pof<ileum colon. vs. 4 g/day). Pentasa 43% 0.0017and for placebo • Pentasa 4 g/d:decrease of 72 points (placebo 21 )(P< 0.01). • Pts with ileum-only disease: 93-point improvement (placebo 2 • Not associated with clinically significant toxicity. Singleton et al Gastroenterology. 1993 May;104(5):1293-301. Fall of SSZ • On the basis of these data and an extensive and satisfactory experience with the newer 5ASA formulations in UC, • By the mid-1990s, Pentasa and other new 5ASA formulations became treatments of choice for mild to moderately active CD, – None of the new agents was ever approved for this indication by the U.S. FDA) • Gastroenterologists abandoned SSZ 2 more studies on Pentasa Unpublished results of 2 additional large-scale RCTs. 5-ASA formulations in induction of remission of CD Meta-analysis Induction of remission in active CD 4 gm Pentasa vs. placebo There is no significant decrease in CDAI with pentasa 3 studies ,(n = 615). (Pentasa – placebo): A non-significant decrease in CDAI: -19.8 (95% CI -46.2 to 6.7, P = 0.14) Clinically significant decrease in CDAI is 50 Lim WC, Hanauer S, Cochrane review 2010 Induction of remission in active CD Contr-release Mesalamine 1-2 g/d Vs placebo 8 trials, in treatment of mildly-moderately active CD Controlled-release mesalamine (Pentasa), Delayed-release mesalamine (Asacol) Olsalazine (Dipentum) 8 trials, (n =342). Induction of remission: 1 to 2 g/day was not superior to placebo RR 1.46; 95% CI 0.89 to 2.40; P = 0.14. Lim WC, Hanauer S, Cochrane review 2010 Induction of remission in CD: Delayed-release mesalamine vs conventional CS 3 trials, (n=178) No statistically significant difference between mesalamine and conventional CS (RR 1.04; 95%CI 0.79 to 1.36) Lim WC, Hanauer S, Cochrane review 2010 Induction of remission in CD Controlled release mesalamine vs Budesonide Budesonide >> Mesalamines for induction of remission A single, (Pentasa with budesonide®), 182 pts (limited to distal ileum and AC) Remission at 16 weeks Pentasa:33.7% (30/89) Budesonide: 60.2% (56/93) (RR 0.56; 95%CI 0.40 to 0.78; P = 0.0007), ABI: = 26.5%, NNT = 4. Lower remission with pentasa for pts with more severe disease at entry (CDAI > 300) (11% Pentasa versus 41% budesonide, P = 0.01, RR 0.26 [95% CI 0.08) Colonic involvement (23%versus 56% respectively, P = 0.03, RR 0.41) Median time to remission: Longer for mesalamine (28 vs 58 d, P = 0.12) Lim WC, Hanauer S, Cochrane review 2010 Induction of remission in CD: SSZ with placebo SSZ at 3 to 6 g/d: only modest efficacy over placebo. A pooled RR of 1.38 (38% higher chance of achieving rem) Limited to pts with Crohn’s colitis. Those with small bowel disease did not improve Three trials,(n=289): SSZ = Placebo (a trend towards stat sig) RR 1.51; 95% CI 0.97 to 2.35; P = 0.07, Combining data from only NCCDS and ECCDS (similar efficacy measures, therapeutic endpoints and duration of therapy) SSZ >> placebo in inducing remission: RR 1.38; 95% CI 1.02 to 1.87, P = 0.04; ABI = 13%, NNT = 8. Lim WC, Hanauer S, Cochrane review 2010 Induction of remission in CD: SSZ Vs steroids Two trials: (n = 260), SSZ clearly inferior to CS RR 0.66; 95% CI 0.53 to 0.81, P = 0.0001. SSZ-treated pts had 34% less chance of achieving remission than those treated with CS Lim WC, Hanauer S, Cochrane review 2010 Induction of remission in CD: SSZ vs SSZ+Steroids Sulfasalazine monotherapy: Less effective than combination therapy with CS Lim WC, Hanauer S, Cochrane review 2010 Induction of remission: Efficacy of 5-ASA in CD: Another Meta-analysis • 3,061 citations: 22 RCT eligible • 6 RCTs: 5-ASA with placebo in active CD for IR • SSZ over placebo: 2 RCT – RR of failure to achieve remission=0.83 95% CI=0.69-1.00), • Mesalamine over placebo: 4 RCTs: No benefit • RR=0.91; 95% CI=0.77-1.06) • Neither SSZ nor mesalamine: Effective in preventing quiescent CD relapse, • Per protocol analysis of mesalamine: appeared to reduce risk of relapse (RR=0.79; 95% CI=0.66-0.95, NNT=13). Ford AC, Am J Gastroenterol 2011 Apr Efficacy: Location wise Limitations in evidences for ASAs • Inconsistent trial outcomes heterogeneity in studies – Enrollment of patients – Inclusion and exlusion criteria, – End-points, – Duration, – Dose, – Delivery system – Placebo responses due to SSZ for induction of remission in CD: Summary • Sulfasalazine at 3 to 6 g/day: Only modestly superior to placebo, – Benefit confined to those with colitis. • Sulfasalazine: Inferior to corticosteroid • Sulfasalazine not an useful adjunct to corticosteroid Lim WC, Hanauer S, Cochrane review 2010 5-ASA for induction of remission in CD Summary • Low dose (1 to 2 g/d) of olsalazine and mesalamine: Ineffective and not superior to placebo. • Higher doses of mesalamine at 3 to 4.5 g/day: – Statistically significant but clinically insignificant changes The role of 5-ASAs in inducing remission of in CDAI scores, active preventing relapse of quiescent – HaveCD notand been consistently effective for induction of mild to moderately CDremission remains in uncertain, and moreactive RCTs CD are – Are inferior to budesonide. required. • Mesalamine seems to be inferior to conventional steroids. Steroids for active CD • Conventional CS – Population studies – 2 RCTs – Meta-analysis (Cochrane review; ACG Task Force) • Budesonide – Compared with placebo – Compared with 5-ASA prep – Coventional CS vs Budesonide Efficacy of Steroids in active CD Population studies Steroid Use Steroid dose Copenhagen study 109/196 (56%) 1 mg/kg Olmsted County 74/173 (43%) 40-60mg/kg Study period 1979-1987 1970-1993 Outcome of Corticosteroid in CD Outcome of the first steroid course : evaluated prospectively regional cohort of 196 patients with CD diagnosed 1979-1987. Immediate outcome at day 30 Prolonged outcome: 30 days after treatment had stopped In all 109 patients treatment was analysed. 1-month outcomes 12-month outcomes Remission Improved 48% 32% Remission 54% Relapse Improved 46% 57% * Remission at 12 Months = 25% No change 20% Relapse 43% Localisation of disease, age, sex or clinical symptoms did not significantly correlate with outcome Munkholm P, University of Coppenhagen, Denmark Gut. 1994 The natural history of corticosteroid therapy for IBD: a population-based • Patients: All pts with IBD in Olmsted County, Minnesota, – CD (n = 173) or UC (n = 185) • Intervention: Systemic corticosteroids during 1970-93 • Outcome: – Immediate outcome (30 days) – 1-year outcome after the first course of corticosteroids • Use of corticosteroids: – CD: 74/173 (43%) – UC: 63/185 (34%) Faubion WA Jr, Gastroenterology. 2001 The natural history of corticosteroid therapy for IBD: a population-based Immediate Outcome* (n = 74) 1-Year Outcome (n = 74) Complete Remission 58% (n = 43) Partial Remission 26% (n = 19) No Response 16% (n = 12) Prolonged Response 32% (n = 24) Steroid Dependent 28% (n = 21) Surgery 38% (n = 28) *30 days after initiating corticosteroid therapy Most patients with CD and UC initially respond to corticosteroids. At 1 year, 32% of patients with Crohn's disease and 48% with ulcerative colitis are corticosteroid free without operation. Faubion W et al. Gastroenterology 2001;121:225 Summary of population studies • • • • Only less than half require steroid Prolonged steroid response in 44%, Steroid dependency in 36%, Steroid resistant in 20% National Cooperative Crohn's Disease Study: NCCS study • • • • • • • • • 569 pts in a placebo-controlled, randomized, multicenter cooperative trial Active and quiescent CD: Prednisone, sulfasalazine, or azathioprine In active disease: Prednisone and sulfasalazine significantly >> to placebo. Azathioprine >> placebo, but the difference did not reach conventional levels of statistical significance. Pts with colonic involvement were especially responsive to sulfasalazine, Pts with small bowel involvement were especially responsive to prednisone. Patients' drug therapy immediately before entry to the study significantly affected subsequent response. For patients with quiescent disease: None of drugs was superior to placebo in prophylaxis against flare-up or recurrence. There is less than a 5% risk that a clinically significant prophylactic effect of any of the drug regimens was missed. Summers RW, Gastroenterology. 1979 Oct;77(4 Pt 2):847-69. Corticosteroids in CD: Induction of Remission 92%† p not calculated 100 82%* % Patients 80 Corticosteroids Placebo 60%* 60 38% 40 30% 20 0 NCCDS 17 weeks ECCDS GETAID 7 weeks 18 weeks Clinical Remission *Randomized controlled trial †Multicenter prospective trial Malchow H et al. Gastroenterology. 1984;86:249. Modigliani R et al. Gastroenterology. 1990;98:811. Summers RW et al. Gastroenterology. 1979;77:847. Steroids for induction of remission in CD: Cochrane review Two studies Diff doses in both study: Same remission rate. Remission with steroids: Pooled RR 1.99; 95% CI 1.51 to 2.64; P< 0.00001). Absolute risk reduction: 30% (95% CI 20% to 41%) NNT 3.33(95%CI 2.4 to 5.0). Although raw data were not available for meta-analysis, it was clear from lifetable data (Summers 1979): Corticosteroids showed benefit over placebo within 1 wk of initiation Benefit plateau at wks 8-10 when approx 70-80% of at risk pts enter remission. A strong placebo effect (Summers 1979), After wk 10, approx 40% of at-risk pts continued to enter remission while on placebo. Benchimol EI, Cochrane review 2010 Efficacy & safety of Conventional CS vs. placebo Induction of remission in active luminal CD • 2 trials: 267 patients • Failure to achieve remission: – Conventional CS: 53/132 (40.2% ) – Placebo: 93/135 (68.9%) • Statistically sig rate of remission in both studies individually • No significant difference in remission in active CD – (RR of failure to achieve remission = 0.46; 95 % CI 0.17 – 1.28) – Because of the heterogeneity between studies ( I2=88 % ,P = 0.004) – Small number of trials. • Indeed, if risk difference was used as summary statistic, then the treatment effect was significant (NNT= 3; 95 % CI 2 – 11). Ford AC, Am J Gastroenterol 2011 Induction of remission: CS vs 5-ASA compounds 3 studies (164/158pts) compared efficacy of CS & 5ASA for induction of late remission (>15 wks). Pooled analysis; CS >> 5-ASA in inducing late remission RR 1.65; 95% CI 1.33 to 2.03; P < 0.00001 Abs risk reduction: 27% (95% CI 17% to 37%) NNT: 3.7 (95% CI 2.7 to 5.9). Conventional steroids in induction of remission in CD: Summary Analyses conducted in the reviews are limited by the design quality of the included studies and the unavailability of raw data • CS effective for induction of remission in CD • Better than 5-ASA for late remission • Whether steroids are more effective than 5-ASA in short-term therapy: more studies required (Highly unlikely such trials will be performed). Steroid dosing for induction of remission in CD • No CS dose-ranging study in pts with CD, – Population based studies: Prednisone 1mg/kg/d achieves high rate of remission • In pts with UC: 3 doses of prednisone (20,40, 60 mg/d) – 40 and 60 mg > 20 mg – 60 mg/d associated with a higher toxicity – But not more effacious than 40 mg/d dose • A small study in pts with UC: Splitting of dosing 6 h, no better than OD dosing • Continuous infusion no better than bolus dosing Tapering of steroid • Current evidence suggests that the algorithm used for CS tapering after achieving an initial response is unlikely to influence the longterm outcome in patients with CD or UC. • In the NCCDS, the dosage of prednisone was adjusted during the 17wk induction period based on the severity of disease activity as measured by – CDAI 300: 0.75mg/kg/d for a – CDAI 150 and 300: 0.5 mg/kg/d – CDAI <150: 0.25 mg/kg/d • In the ECCDS, 6-methylpred was given initially and tapered over 6 wks – – – – – – Induction: 48 mg/d in wk 1 tapered to 32 mg/d in wk 2, 24 mg/day in wk 3, 20 mg/day in wk 4, 16 mg/day in wk 5, 12 mg/day in wk 6. • In patients who received placebo after induction of remission, about 35% remained in remission at 2 years. Tapering of steroids • Dose of steroid – Oral: 40–60 mg/d or 1 mg/kg/d of prednisone or equivalent – Parenteral CS: • Hydrocortisone 200–300 mg/d • Methylprednisolone: 40–60 mg/day • Induction of response: Averages 7–14 d • Tapering: – 5 mg/wk of prednisone (or equivalent) to a dose of 20 mg – Then, 2.5–5 mg/wk below 20 mg • For patients failing to respond to 7–14 d of high-dose oral prednisone or equivalent CS, use parenteral CS • Budesonide: Gradually taper from 9 mg to 6mg and subsequently 3 mg. Budesonide • Limited systemic bioavailability due to extensive (90%) first pass hepatic metabolism by cyt p-450 enzymes, • First described in pilot studies in early 1990’s (Lofberg 1993). • Contr release prep designed to deliver in distal small intestine • Two formulations: • Controlled-ileal release: – uses a gelatin capsule containing acid-stable microgranules composed of an inner sugar core surrounded by a layer of budesonide in ethylcellulose and an outer acrylic-based resin coating (Eudragit) that dissolves at a pH of 5.5 or higher. – Absorption of this formulation in ileocecal region is approx 69% • pH-dependent release budesonide – pH-dependent release formulations are available as capsules which contain 400 pellets with a diameter of 1 mm, coated with Eudragit Induction of remission in active CD Budesonide Vs Placebo • 2 large multicentre, DBRCT: Greenberg 1994; Tremaine 2002). – Greenberg 1994: Conducted over 27Canadian centres – Tremaine 2002 study recruited across 24 American centres. • Greenberg 1994: 258 participants were randomized into 4 gp – 3 groups assigned budesonide,3mg (n=67), 9 mg (n=61) &15 mg (n=64) in 2 dd, – Fourth group received placebo (n = 66). • In the Tremaine study, 200 randomized into three groups – 2 budesonide groups received 9 mg as either 9 mg OD (n= 80) or 4.5 mg BD(n=79) – Third group received placebo (n = 41). • Primary outcome measure was assessed at 8 wks, at which point medications were tapered. • Total treatment duration 10 wks. Seow CH, Cochrane review, 2009 Induction of remission in active CD Budesonide Vs Placebo At all three time points, budesonide>> placebo Week 2: RR 2.97 (95% CI, 1.67 to 5.29) Week 4: RR 1.67 (95% CI, 1.12 to 2.47); Week 8: RR 1.96 (95%CI, 1.19 to 3.23). Time to remission Greenberg 1994:: No diff (9 mg and 15 mg) Time to remission in bud vs plac not provided. Tremaine 2002 On post hoc analysis: Med time to remission shorter for budesonide (27 days vs 66 days; P < 0.05). Budesonide effective for IR Medium time for response 27 d EL: 1 RG 1 Seow CH, Cochrane review, 2009 Induction of remission in active CD Budesonide vs Conventional CS 9 RCTs compared budesonide to CS. At 8 wks, a total of 750 pts in 8 trials. Budesonide << conventional CS (RR 0.85 (95% CI 0.75 to 0.97). Seow CH, Cochrane review, 2009 Induction of remission: Conventional CS > Budesonide Six RCTs, 669 pts with distal ileal, IC, rt-sided colonic CD Failure to achieve remission: Conventional CS: 116/304 (38.2 % ) Budesonide:173/365 (47.4 % ) RR of failure to achieve remission (stat significant) = 0.82; 95 % CI 0.68 – 0.98 in favour of CS CS related adverse events commoner (RR=1.64; 95 % CI 1.34–2) Ford AC, Am J Gastroenterol 2011 Induction of remission in active CD Budesonide vs Conventional CS Gross 1996: Mean time for remission Budesonide: 22.3 ± 12.1 d Prednisolone: 20.0 ± 17.7 days. Tursi 2006: Mean time to remission (budesonide faster) Budesonide: 27 d (range 23 to 31 d) Beclomethasone: 41 d (36 to 46 d) (P< 0.05) Seow CH, Cochrane review, 2009 Induction of remission in SEVERELY active CD Budesonide Vs Conventional CS 2 studies examined proportion of pts with severe disease (CDAI > 300) who achieved remission. Pooled RR for remission 0.52 (95% CI, 0.28 to 0.95), in favour of CS steroids. Seow CH, Cochrane review, 2009 IR in active CD: Effect on CDAI Budesonide Vs Conventional CS Reduction in CDAI more with Conventional CS Limited information available on the change in CDAI. Statistically larger change in CDAI in conventional CS Weighted mean diff in CDAI of 42.27 points (95% CI 14.86 to 69.67) Seow CH, Cochrane review, 2009 IR in Ileal or right sided ileo-colonic disease Budesonide Vs Conventional CS A pooled analysis of six studies of pts with terminal ileal, or ileo-colonic disease, A non-significant trend in favour of Conv CS RR for remission 0.86 (95% CI, 0.75 to 1.00; P = 0.05). Seow CH, Cochrane review, 2009 Induction of remission: Steroid side effects Budesonide vs Conventional CS Budesonide is approx 13% less effective than conventional CS for ind of rem in CD: Kane 2002 Present study: 15% less Six RCT (703 pts): Frequency of CS-related adverse events Budesonide < Conv steroids (RR 0.64, 95%CI 0.54 to 0.76). None of the studies reported mortality outcomes. Seow CH, Cochrane review, 2009 Induction of remission in active CD Budesonide 9 mg vs Mesalamine A single trial of 182 pts compared budesonide with mesalamine More favorable response with a longer duration of t/t with budesonide Relative risk At 2 weeks: 1.23 (95% CI, 0.85 to 1.78), P: NS At 4 weeks, 1.26 (95% CI, 0.88 to 1.79), P: NS At 8 weeks, 1.63 (95% CI, 1.23 to 2.16; P = 0.0007); At 12 weeks, 1.59 (95% CI, 1.17 to 2.15; P =0.003), At 16 weeks, the relative risk was 1.79 (95% CI, 1.28 to 2.50; P = 0.0007). Seow CH, Cochrane review, 2009 Induction of remission in active CD (CDAI>300) Budesonide 9 mg Vs Mesalamine Seow CH, Cochrane review, 2009 Budesonide in induction of remission: Confidence and Caveat • These results are similar to those found in previous 3 meta-analyses (Papi 2000; Kane 2002; Otley 2005). Caveat: Budesonide was given at ’full’ dose (9 mg) for first 8 wks of study and then tapered, but not discontinued at the final study evaluation, whereas conventional CS were given at full dose for two wks, and then tapered Efficacy and safety of budesonide vs. placebo in inducing remission in active luminal CD • 2 eligible RCTs involving 458 pts • Included patients with terminal ileal, ileocolonic, or right-sided colonic CD. • Failure to achieve remission: • Budesonide: 192 (54.7% ) of 351 • Placebo: 81 (75.7% ) of 107 • With a statistically significant effect in favor of budesonide (RR of failure to achieve remission = 0.73; 95 % CI 0.63 – 0.84. • NNT with budesonide to achieve remission in one patient was 5 (95 % CI 3 – 9). • Side effects: – Budesonide: 312 (88.9% ) of 351 budesonide patients and – Placebo: 88 (82.2 % ) of 107 placebo patients (RR = 1.05; 95 % CI 0.91 – 1.22). AJG: IR in CD Conv steroid vs Budesonide Six RCTs ,669 pts with distal ileal ileocecal, or right-sided colonic CD, Failure to achieve remission: Conv steroid: 116 (38.2 % ) of 304 Budesonide: 173 (47.4 % ) of 365 RR of failure to achieve remission= 0.82;95% CI 0.68 – 0.98 NNT: 11 (95 % CI 6 – 50) (To achieve remission in 1 pt) Steroids for induction of remission: Summary • Benefit of corticosteroids over 5-ASA at inducing remission with short-term therapy is unclear, – Unavailability of raw data, – poor study design and – poor study enrollment. • Most clinicians treat active CD with full-dose steroids for 3 to 6 weeks followed by a gradual wean. The total course of therapy is often 3 to 4 mo in duration and the benefits to patients receiving corticosteroids shown by this review at longer follow-up periods are clinically applicable. • Future studies: • Comparison of short term outcome between steroids and 5-ASA: Non-inferiority trial design. • Additional studies: – corticosteroid delivery, – phenotype and disease location in predicting the likelihood of inducing remission with corticosteroids, – with particular attention to comparing steroids to 5-ASA therapy in patients with colonic disease. Azathioprine Induction of remission in CD: Combining steroids and AZA • Role of combined antimetabolite and steroid in active disease has been controversial. • NCCD Study failed to show a statistically significant benefit for aza monotherapy and has been criticized for not allowing concurrent steroid therapy during the lag period before azathioprine could act • Combination of azathioprine & steroids may lead to a higher response rate with less steroid use. Induction of remission in CD: Immunosuppressive drugs Cochrane Review: 2010 • 8 Plcebo controlled RCT using aza and 6-MP in adult pts with CD – 5 dealt with active disease – 3 had multiple therapeutic arms Induction of remission: AZA/6-MP vs Placebo 8 studies (6 AZA, 2 6MP) Overall response rate Drugs: 113/209 (54%; 95% CI 47% to 61%) Placebo: 72/216 (33%; 95% CI 27% to 40%) Pooled odds ratio for response AZA or 6-MP: 2.43 (95% CI 1.62 to 3.64). NNT one patient to respond was 5 AZA Vs Placebo Pooled OR: 2.06 (95% CI 1.25 to 3.39). 6-MP Vs placebo Pooled OR: 3.34 (95% CI 1.67 to 6.66). NNT for one pt to respond was about 3. Induction of remission: Effect of duration of AZA/6-MP on remission rate Present 1980: Mean time to response with 6MP in active CD : 3.1 mo 19% of pts who responded took > 16 wks to respond. Time for response with AZA mono: Long As monotherapy, not a suitable inducing Durremission of T/T Response rate drug NNT (2-12mo) <17 wks 1.55 (95%CI 0.52-4.59 18 >17 wks 2.61 (95%CI 1.69-4.03) 4 In an attempt to accelerate the onset of action, a trial evaluating the efficacy of a high-dose 36h infusion was no more effective than conventional oral dosing Induction of remission: Steroids sparing effect of AZA/6-MP Ability to reduce prednisolone dose is an important outcome measure It can be assessed 1) the ability to follow a pre-defined steroid tapering regimen, 2) Ability to reduce steroid dose to < 10 mg/d while maintaining remission. In 5 studies reporting data on reduction of steroid consumption: Reduction in steroids in Pts receiving anti-metabolites: 76/117 (65%; 95% CI 56% to 74%) Pts receiving placebo: 39/109 (36%; 95% CI 27% to 45%) Pooled OR in favour of anti-metab: 3.69 (95% CI 2.12 to 6.42) Indicating a significant steroid sparing effect. NNT : 3 (to obtain a steroid sparing effect in 1 pt) Induction of remission: Fistula healing with AZA AZA heals fistula: no definite evidence Response of fistulae to AZA or 6-MP: reported by four studies Two trials reported no difference between AZA and placebo One trial (Present 1980) reported the no of fistulae that responded rather than the no. pts with fistulae that responded, Overall response rate: Therapy: 6/11 (55%) Placebo: 2/7 (29%) Pooled OR of 4.68 (95% CI 0.60 to 36.69) favouring fistula healing. (NS) AZA/6-MP: Adverse event during IR Most common adverse effects Allergic reactions (2.3%) Leucopenia (1.4%) Pancreatitis (1.4%) Nausea (1.4%) No malignancies or deaths Adverse events severe enough to cause withdrawal: AZA/6-MP: 20/214 (9.3%; 95% CI 5.8% to 14.1%) Placebo: 5/215 (2.3%; 95% CI 0.1% to 5.3%) Pooled OR 3.44 (95% CI 1.52 to 7.77) in favour of AZA. NNT: 14 (to observe an adverse event in 1 pt) Induction of remission: Immunosuppressive therapy Overall data for IS vs. placebo Combining the studies IS therapy >> placebo: statistically significant (RR = 0.84;95 % CI = 0.76 – 0.94) NNT: 8 (95% CI = 5– 20). Suppressing immune system: Have some impact on inducing remission in CD Differing M/A of each class of IS drugs Not appropriate to pool data. No significant difference between each of three classes of drugs and for each individual class there was no statistically significant effect in favour of Rx Khan KJ, AJG, 2011 Mx: Statement 3 • III A: Terminal ileal or localised ileocaecal disease: Mild to moderately active CD involving terminal ileum (L1) or localised ileocaecal disease should be treated with budesonide 9 mg daily. • IIIB: If there is no response systemic corticosteroids should be used. • IIIC: Steroids should be tapered over 3 months. (EL • IIID: Severely active CD involving terminal ileum (L1) or localised ileocaecal disease should be treated using systemic corticosteroids. (EL 1, RG 1) 3) Terminal ileal or localised ileocaecal disease: Mild to moderately active CD involving terminal ileum (L1) or localised ileocaecal disease should be treated with budesonide 9 mg daily. If there is no response systemic corticosteroids should be used. Steroids should be tapered over 3 months. Severely active CD involving terminal ileum (L1) or localised ileocaecal disease should be treated using systemic corticosteroids. Comments: •You could also argue that those with severe ileal disease with strictures or fistulae should undergo surgery with resection as a primary therapy •The use of budesonide depends on availability and cost. •Need to give some alternatives •ASA may be useful in mild disease. •It would be better to use the “conventional” instead of “systematic” •Budesonide 9mg (Availability?) •Depend on the situation in countries. Budesonide is not available in some countries including Japan.Statement should consider the difference of medical situation in Asian countries. •Steroid should be used at initial stage, but AZA or infliximab can be considered for maintenance. •there is good evidence either for budesonide or CS to induce remission •Reduced too lengthy. •Not all need steroids. •Too many substatements here will make the voting difficult Revised Mx: Statement 3 • III A: Terminal ileal or localised ileocaecal disease: Mild to moderately active CD involving terminal ileum (L1) or localised ileocaecal disease should be treated with budesonide 9 mg daily. (EL 1, RG 1) • IIIB: If there is no response conventional corticosteroids should be used. (EL 1, RG 1) • IIIC: Steroids should be tapered over 3 months. (EL • IIID: Severely active CD involving terminal ileum (L1) or localised ileocaecal disease should be treated using sys(Conventional) corticosteroids. (EL 1, RG 1) Mx: Statement 4 • Colonic disease (L2): Sulphalazine can be used for mild CD limited to the colon. • Mesalamines are not effective. • Moderately severe or severe colonic disease should be treated with systemic corticosteroids. • 4) Colonic disease (L2): Sulphalazine can be used for mild CD limited to the colon. Mesalamines are not effective. Moderately severe or severe colonic disease should be treated with systemic corticosteroids. Comments: •"Need to amend statement. •(i) Sulphalazine can be used for mild CD limited to the colon, & (ii)Mesalamines are not effective are contradicting as Sulphalazine also contra Mesalamines(5-ASA)" •Balsalazide and meszavant are options. Also, 5-ASAs work as well and given in higher doses can target the colon. Sulpha intolerance and allergy are common. •5ASA/S2P are both acceptable therapies for mild-mod CD •Biologics are also indication for moderately severe or severe colonic disease. •Mesalamines can be used in colon type CD. •Topical 5-ASA can be useful for distal colonic CD and may be useful as an adjunct therapy for Lt sided colonic CD. Revised Mx: Statement 4 IVa. Colonic disease (L2): Sulphalazine can be used for mild CD limited to the colon. (EL 1, RG 1) IVb. Mesalamines are not effective. (EL 1, RG 1) IVc. Moderately severe or severe colonic disease should be treated with systemic corticosteroids. EL 1, RG 1 Mx: Statement 5 • Extensive small intestinal disease (L1, L4): For extensive small intestinal disease, mesalamines or sulphasalazine are ineffective both for the induction of remission or maintenance of remission. • Patients with mild to moderate or severely active disease should be treated with systemic corticosteroids. • Immunosuppressive drugs (azathioprine, 6-MP or methotrexate) should be started simultaneously. Those who are sick may be treated with intravenous steroid. Alternatives to corticosteroid is anti-TNF agent. 5) Extensive small intestinal disease (L1, L4): Mesalamines or sulphasalazine are ineffective both for the induction of remission or maintenance of remission. Patients with active disease should be treated with systemic corticosteroids. Severe disease may require intravenous steroids. Alternative to corticosteroid is anti-TNF agent. Immunosuppressive drugs (azathioprine, 6-MP or methotrexate) should be started simultaneously. Comments: •This is unclear. do you mean that IS drugs should be started simultaneously with steroids or biologis or both. •Avoid "ineffective". "Consider starting immunosuppressive early, especially with recurrent or severe disease" may be better. •"If patients' adherence is good, enteral nutrition therapy is also indication for small intestinal Crohn's disease. •Especially, it should be considered in pediatric CD." •Intravenous steroid should not be used in CD patients, and anti-TNF is recommended. •Reduced •Too many substatements here will make the voting difficult •The statement should be clear that we are talking about: anti-TNF being the alternative for severe extensive small bowel disease not responding to IV steroids. Revised Mx: Statement 5 • Va. Extensive small intestinal disease (L1, L4): For extensive small intestinal disease, mesalamines or sulphasalazine are ineffective both for the induction of remission or maintenance of remission. (EL 3, RG C) • Vb. Patients with mild to moderate or severely active disease should be treated with Conventional corticosteroids. (EL 3, RG 3) • Vc. Immunosuppressive drugs (azathioprine, 6-MP or methotrexate) should be started simultaneously. Those who are sick may be treated with intravenous steroid. (EL 3, RG C) • Vd. Alternatives to corticosteroid is anti-TNF agent. (EL 3, RG C) Mx: Statement 6 • Ileo-colonic disease (L3): Mesalamines or sulphasalazine alone are ineffective both for the induction of remission or maintenance of remission. • Mild to moderate disease and severe disease should be controlled using systemic corticosteroids. • Immunosuppressive drugs (azathioprine, 6-MP or methotrexate) should be started simultaneously. • Those who are sick may be treated with intravenous corticosteroid. • Alternative to corticosteroid is anti-TNF agent. 6) Ileo-colonic disease (L3): Mesalamines or sulphasalazine alone are ineffective both for the induction of remission or maintenance of remission. Moderate and severe disease should be controlled using systemic corticosteroids. Immunosuppressive drugs (azathioprine, mercaptopurine or methotrexate) may be started simultaneously or commenced for relapse or failure of corticosteroids. Severe disease may require intravenous corticosteroid. Alternative to corticosteroid is anti-TNF agent. Comments: •What about using antibiotics? •Severity of disease should be defraud •Sulfasalzine may be effective in inducing remission in mild cases •Intravenous steroid should be avoided. •Too many substatements here will make the voting difficult •Again, stament should be clear that: anti-TNF is the alternative for severe disease not responding to IV steroids. Mx: Statement 6 • Ileo-colonic disease (L3): Mesalamines or sulphasalazine alone are ineffective both for the induction of remission or maintenance of remission. • Mild to moderate disease and severe disease should be controlled using systemic corticosteroids. • Immunosuppressive drugs (azathioprine, 6-MP or methotrexate) should be started simultaneously. • Those who are sick may be treated with intravenous corticosteroid. • Alternative to corticosteroid is anti-TNF agent. Conventional Mx: Statement 7 • Active Crohn's disease with a concomitant abdominal abscess should be treated with antibiotics, percutaneous or surgical drainage followed by delayed resection if necessary, in addition to specific medical management of CD. [III-C] Evidences • There are no RCTs • When active small bowel CD is associated with a concomitant abdominal abscess, – Drainage followed by medical treatment if there are no obstructive symptoms – Percutaneous drainage and delayed resection if there are obstructive symptoms. – Some abscesses do not lend themselves to percutaneous drainage. • There are no randomized studies in the literature Although most case series favour a delayed elective resection – Opinions vary. 7) Active small bowel Crohn's disease with a concomitant abdominal abscess should preferably be managed with antibiotics, percutaneous or surgical drainage followed by delayed resection if necessary. Comments: •Surgery may be the first line in some cases •Primary surgery can often manage perforating disease unless there is severe soiling or very immunosuppressed patients with risk of anastomotic breakdown. •What about the role of biologicts/immunomodulation when others has been controlled •Reduced •"Anti inflammatory? •Surgery as first line? " Revised Mx: Statement 7 • Active small bowel Crohn's disease with a concomitant abdominal abscess should preferably be managed with antibiotics, percutaneous or surgical drainage followed by delayed resection if necessary. EL 3, RG C Induction Mx: Statement 8 • Esophageal or gastro-duodenal Crohn's disease (L4) may best be treated with a proton pump inhibitor, if necessary together with systemic corticosteroids and thiopurines or methotrexate. Gastroduodenal CD • GD involvement in CD : mostly as a Hp-negative focal gastritis, – Endoscopically in 20% – Histological: 40% • Mostly in pts with concomitant distal disease usually ileal. • Mostly asymptomatic, only 4% symptomatic – Dysphagia, odynophagia, pyrosis for esophageal – Nausea, anorexia, epigastric pain, dyspepsia for GD CD Alcanta, Endoscopy 193; Oberhuber G Virchows Arch 1998;Oberhuber, Gastroenterology 1997 Quality of literature on Gastroduod CD • No high-quality-level evidence-based data, – Small uncontrolled retrospective case series – Anecdotal reports, – Clinical experience, – Pathophysiological theories – Result extrapolation from studies performed on more distal disease. Activity of concomitant distal CD usually determines the indication for T/T Proton-Pump Inhibitors • No data are available on this topic • As gastric acid may also perpetuate gastrduodenal ulcers due to CD, there acid supppression is important • Acid suppression alone probably does not control the idiopathic mucosal infl ammatory process. • Both acid suppresion and antiinflammatory/immunosuppressive seems appropriate. Mesalamines and SSZ in GD CD • Sulfasalazine: no place in Mx of proximal CD • Mesalamine: No place • Pentasa: may be – No data Steroids in GD CD • A small retrospective study in 10 pts with symptomatic CD showed, in every patient, a good clinical response with oral corticosteroids • Similar results in a retrospective case series. – Of 46 patients treated with steroids for nonobstructingdisease, 42 had good to excellent results, concomitant medication with sulfasalazine, anH 2 RA or intermittently with azathioprine or metronidazole. • Budesonide: No data Azathioprine, 6-Mercaptopurine • Only anecdotal clinical experience has been published • Indications: – Those who remain symptomatic on steroids, – Steroid-dependent – Maintenance therapy • Korelitz et al. Am J Gastroenterol 1993 – 20 years of clinical experience with 6-MP – All achieved in healing or marked improvement in gastroduodenal lesion • Miehsler W, Inflam Bowel Dis 2001 – 12 pts with UGI CD treated with AZA – Prednisone could be discontinued in 7 after 4–6 mo – A significant decrease in CDAI score Infliximab • Resolution of severe esophagogastric and esophago-bronchial fistula with Infliximab Heller, IBD 1999; Ho JCG 2002 • 4 cases of severe isolated gastroduodenal CD – 2 were treated with infliximab, 1 healed, other did not Grubel, Dig Dis Sci 2003 • Severe gastric and duodenal CD with diffuse thickening and ulceration throughout the antrum and duodenum: Responded to Infliximab Firth JJ, Am J Gastroenterol 2002 Gastroduodenal CD Balloon Dilation • Presence of a stenosis with obstruction indicates a severe disease • If medical therapy with steroid and immunosppr drugs does not alleviate symptoms, balloon dilation or surgery • Successful dilatation for obstructive gastroduodenal CD Matsui et al, Murthy; Kelly and Hunter 8) Esophageal or gastro-duodenal Crohn's disease (L4) may best be treated with a proton pump inhibitor, if necessary together with systemic corticosteroids and thiopurines or methotrexate. Comments: •the evidence of the efficacy of PPI in upper GI CD is insufficient. Biologics should be considered in severe upper GI lesions. Revised Mx: Statement 8 • Esophageal or gastro-duodenal Crohn's disease (L4) is treated with conventional corticosteroids and thiopurines or methotrexate. Short term use of a proton pump inhibitor should be considered for upper GI symptoms. [III-C] Maintenance Mx: Statement 9 • Treatment for the maintenance of remission should be recommended in almost all CD patients. [II-2-B] • Conventional steroid and budesonide are not recommended in the maintenance of remission. [IA] • The first line of treatment for maintenance of remission is thiopurines. Methotrexate can also be used. [I-A] • Alternative to immunomodulators is anti-TNF therapy. Mention in text some patients do not require treatment. Maintenance of remission 5-ASA Vs Placebo 16 RCT, 2,496 pts, Rate of relpase 5-ASA vs control: 55.8 % vs 57.0 % RR of relapse with 5-ASA 0.97 (95 %CI = 0.90 – 1.05), 5-ASA no more effective than control in maintaining remission Ford AC, Am J Gastroenterol 2011 Apr Steroid for Maintenance Maintenance of remission: Budesonide • 11 studies included – 8 studies: Budesonide Vs placebo, – I study: Budesonide Vs 5-ASA – I study: Budesonide Vs conventional CS – 1 study: Budesonide two doses • 8 studies used a controlled ileal release budesonide, while one used a pH-modified release formulation. Benchimol EI, Cochrane review, 2010 • • • • • • • • 6 mg daily was no more effective than placebo for maintenance of remission at 3 months (RR 1.25; 95% CI 1.00 to 1.58; P = 0.05), 6 months (RR 1.15; 95% CI 0.95 to 1.39; P = 0.14), or 12 months (RR 1.13; 95% CI 0.94 to 1.35; P = 0.19). Budesonide was not more effective than weaning doses of prednisolone for maintenance of remission at 12 months (RR 0.79; 95% CI 0.55 to 1.13; P =0.20), but was better than mesalamine 3 grams per day (RR of remission 2.51; 95% CI 1.03 to 6.12; P = 0.04). Budesonide 3 mg daily was more effective than placebo at 3 months (RR 1.31; 95% CI 1.03 to 1.67; P = 0.03). This benefit was not sustained at 6 months (RR 1.10; 95% CI 0.81 to 1.50; P = 0.53), or 12 months (RR 1.04; 95% CI 0.84 to 1.30; P = 0.70). No differences in efficacy were detected based on the different formulations of budesonide, methods used to induce remission, or budesonide dose. The use of budesonide 6 mg resulted in slight improvements in CDAI scores when assessed at 6 months (WMD -24.3; 95% CI -46.31 to -2.29; P = 0.03) and 12 months (WMD -23.49; 95% CI -46.65 to -0.32; P = 0.05) and mean time to relapse of disease (WMD 59.93 days; 95% CI 19.02 to 100.84; P = 0.004). Adverse events were more frequent in patients treated with 6 mg of budesonide compared with placebo (RR 1.49; 95% CI 1.01 to 2.19; P = 0.05), but not in patients using lower doses of budesonide. These events were relatively minor and did not result in increased rates of study withdrawal. Abnormal adrenocorticoid stimulation tests were seen more frequently in patients receiving both 6 mg daily (RR 2.88; 95% CI 1.72 to 4.82; P < 0.0001) and 3 mg daily (RR 2.73; 95% CI 1.34 to 5.57; P = 0.006) compared with placebo. Benchimol EI, Cochrane review, 2010 Placebo-controlled trials of budesonide for maintenance of medically induced remission in Crohn’s disease Author Löfberg (1996) No. of Dosage (mg/day) patients 96a 6 Duration (Months) 12 3 Greenberg (1996) 105a 6 75a 6 12 179 3 74 63 P NS 61 12 46 67 NS 67 Controlled Controlled Ileal release 60 NS Controlled Ileal release 48 12 formulation Ileal release 70 3 Gross (1998) Budesonide Placebo 59 3 Ferguson (1998) Relapse 65 NS pH-modified release Continued: Author Cortol (2001) Hanauer (2005) Duration Relapse No. of Dosage (mg/day) (Months) patients Budesonide Placebo 120 6 4-5 33 65 110 6 12 40 47 formulatio n P 0.05 at Controlled 3 months ileal release NS Controlled ileal release Maintenance of remission in CD 6mg Budesonide = Placebo Only 1 study: stat sifgnificant benefit at 3 mo (RR 1.90; 95%CI 1.29 to 2.81). Pooled RR of continued rem with budesonide At 3 mo: 1.25 (95% CI 1.00 to 1.58; P= 0.05) At 6 mo: 1.15 (95% CI 0.95 to 1.39; P= 0.14) At 12 mo: 1.13 (95% CI 0.94 to 1.3; P= 0.19), Budesonide 6 mg/d is not effective for maintenance of clinical remission in CD Benchimol EI, Cochrane review, 2010 Maintenance of remission in CD 3mg Budesonide = Placebo Maintenance of remission: At 3 mo: Budesonide>> placebo (RR1.3; 95%CI 1.03 to 1.6; P= .03), NNT: 8. At 6mo (RR1.10; 95% CI 0.8 to 1.5;P =0.5) At 12mo:(RR 1.04;95%CI 0.8 to 1.3; P 0.7 Not effective at 6 mo and 12 mo Benchimol EI, Cochrane review, 2010 Maintenance of remission in CD 3mg Budesonide = 6 mg budesonide Benchimol EI, Cochrane review, 2010 Maintenance of remission in CD 9mg Budesonide = 6mg in Benchimol EI, Cochrane review, 2010 Maintenance of remission Budesonide 9 mg = Conventional CS One study compared CIR budesonide 9 mg to prednisolone 40 mg/d with a weaning schedule (Schoon 2005). Remission rates (defined by CDAI 200) were not significantly different 3 months (RR 0.81; 95 CI 0.60 to 1.09), 6 months (RR 0.79; 95% CI 0.56 to 1.12), 12 months (RR 0.79; 95% CI 0.55 to 1.13). Benchimol EI, Cochrane review, 2010 Maintenance of remission in CD Budesonide 6mg >> Mesalamine 3 g One study compared Budesonide Vs pH-dep mesalamine in steroid-dept CD Remission rates after 1 yr of Rx Budesonide >> mesalamine (RR2.51;95% CI 1.03 to 6.12; P=0.04). Benchimol EI, Cochrane review, 2010 Mean time to relapse of disease with budesonide used for maintenance • Budesonide 6 mg versus placebo – Budesonide 6 mg significantly increased mean time to relapse (59.9d; 95%C 19 to 100.8; P=0.004). • Budesonide 3 mg versus placebo – Significant benefit for mean time to relapse for budesonide(30.5d; 95%CI 9.1 to 52.09; P=0.005), • Budesonide 6 mg versus budesonide 3mg : Amongst dowas relapse, – Meanpts timewho to relapse not significantly different in patients Budesonide timebudesonide to relapse6 by • Budesonideprolong 9 mg versus mg:approx 60 d with – Median to relapse in 6daily mg group was 809 days (95% CI 360 to 6mg/d or 30time d with 3 mg 1259 days) – Median time to relapse in 9 mg group was 1049 days (95% CI 384 to 1713 days). – there was no significant difference between groups. • Budesonide 9 mg versus traditional corticosteroids: Study did not report • Budesonide 6 mg versus mesalamine 3 g: Study did not report Benchimol EI, Cochrane review, 2010 Why budesonide or steroid are not effective for maintenance? • Not entirely clear – Use of systemic corticosteroids may contribute to reduced immune cell apoptosis (Towers 2005). – Early use of steroids may propagate abnormal immune response in pts with CD resulting in repeated episodes of inflammation and tissue damage – Decreased efficacy of corticosteroids with repeated or long-term use (Van Den Brande 2002). • It is also possible that the location of disease in pts receiving budesonide who relapse: Is outside of location of budesonide greatest effect (ileo-cecal region). Benchimol EI, Cochrane review, 2010 Azathioprine for maintenance of remission in CD • 1118 references reviewed, • 21 potentially eligible studies were identified. – Thirteen of these studies were excluded for various reasons. – 8 trials were identified that satisfied the inclusion criteria as placebo controlled RCT, • Maintenance Rx with AZA was compared to no Rx • 1 trial (Hanauer 2004) used 6-MP for maintenance of remission. AZA for maintenance of remission • 5 studies dealt exclusively with quiescent disease • In total 550 pts included, – 208 received azathioprine, – 47 received 6-MP – 295 received placebo • 2 studies included steroid dep pts & attempted to withdraw steroids after adding AZA or placebo • 2 other studies (O’Donaghue 1978, Lemann 2005) identified pts who were in remission on AZA and randomized them to receive a 12mo or 18 month of either AZA or placebo. AZA/6-MP: Maintenance of Remission in CD Overall remission rate AZA: 147/208 (71%; 95% CI 64% to 77%) 6-MP: 24/47 (51%; 95% CI 36% to 66%) Placebo: 141/255 (55%; 95% CI 49% - 61%) Peto OR for response AZA: 2.32 (95% CI 1.55 to 3.49) 6-MP: 3.32 (95%CI 1.40 to 7.87). NNT: AZA: 6 for prevention of 1 recurrence 6-MP: 4 for prevention of 1 recurrence Increase in dose of AZA increases response rate • When the maintenance therapy data were analysed for the effect of azathioprine dose range 1.0 to 2.5 mg/kg/day), Adequate dosing of AZA is important Peto OR for response Do we really use 2-2.5mg dose in Asia – At 1 mg/kg/d: 1.20 (95% CI 0.60 to 2.41) – At 2 mg/kg/d: 3.01 (95% CI 1.66 to 5.45) – At 2.5 mg/kg/d: 4.13 (95% CI 1.59 to 10.71) During maintenance t/t: AZA withdrawal due to drug side effects Drug withdrawal due to adverse event: AZA: 6% 6-MP: 19% Placebo: 3% AZA/6-MP>Placebo AZA: Peto OR 3.74; 95% CI 1.48 to 9.45). Number needed to harm (NNH) was 20. 6-MP: similar results (Peto OR 2.04; 95%CI 0.63 to 6.60). Common events for withdrawal Pancreatitis, Leukopenia, Nausea, Allergic reaction Infection. During maintenance T/T: Steroid withdrawal on AZA Although desired Data very small and non-convincing Two very small studies reporting steroid withdrawal data: Ability to reduce or discontinue steroid on maintenance: AZA: 13/15 (87%; 95% CI 60% to 98%) compared to Placebo: 8/15 (53%; 95% CI 27% to 79%) Peto OR 5.22; 95% CI 1.06 to 25.68) NNT for reduction in steroid =3 Summary: AZA for maintenance At this time AZA appears to be an effective agent for maintenance of remission and may be effective as a steroid sparing agent. Strength of evidence: Weak Available studies and eligible patients: Relatively small (208 AZA; 47 6-MP; 295 placebo) How long to use AZA for maintenance? • The current literature does not provide a great deal of guidance on this point. • Bouhnik 1996:Patients might be maintained on AZA for 42 mo before stopping How long to use AZA: Long-term efficacy of AZA does not wane after four years of continuous treatment • Pts with steroid-dep CD in remission on AZA (2-2.5 mg/kg) for between 2-8 yrs were assigned into two groups. – Group A (n=58) : Treated continuously for 2 to 4 yrs – Group B (n=42): Treated continuously for 4 to 8 yrs. • Assessment: – FU every mo for 1 yr with physicals, compliance – CDAI, IBD QOL: 3 monthly ; Colonoscopy with CDEIS at baseline and at end • Endpoints: – primary end point: was relapse after 1 year. – Secondary end points: safety of treatment, QOL, and endoscopic healing. • Relapse rates per protocol: 19.6% and 11.9%, respectively (p: NS). • No sig differences in overall and at each time point between two t/t groups regarding compliance, safety, CDAI, IBDQ, and CDEIS • Multivariate analysis: No identifiable factor influencing remission • Long-term Rx with AZA for steroid-dep CD is efficacious and safe. Mantzaris GJ, J Crohns Colitis 2007 Sep;1(1):28-34 Athens, Greece How long to use AZA? • Further research is required to determine if patients can stop taking AZA after long-term use without risking relapse. • Most clinicians, however use for a longer duration Relapse while on AZA • ECCO Statement 6E: • Patients receiving azathioprine or mercaptopurine who relapse should be evaluated for adherence to therapy and have their dose optimised. Change of their maintenance therapy to methotrexate [EL1b RG B] or anti-TNF therapy [EL1a RGB] should be considered. • Surgery should always be considered as an option in localised disease [EL4, RG D]. • Patients receiving azathioprine or mercaptopurine who relapse whilst on standard maintenance doses can have their dose escalated (N2.5 mg/kg/day or N1.5 mg/kg respectively) until leucopenia occurs [EL3, RG D], or according to 6-TGN concentrations [EL2a, RG B] (see Section 5.4.6). • Methotrexate is another option [EL1b, RG B] (see Section 6.2.5). Anti-TNF therapy has also proven to be Methotrexate for remission The probability for maintaining clinical remission as a function of time in the 50 patients who achieved this therapeutic goal after 3 months and were maintained on MTX are presented in Figure 2. The cumulative probability not to relapse was 95.3% (95% CI: 75.9–100%), 89.5% (95% CI: 69.6–100%), 70.6% (95% CI: 47.1–94.1%) and 62.8% (95% CI: 33.5–92.0%) at 6 months, 1, 2, and 3 years after starting MTX treatment, respectively. There was a significant decrease in the mean HBI from 4.5 points at the beginning of MTX therapy to 2.1 points after 3 months of treatment (P < 0.001). Subsequently, the mean HBI remained unchanged for up to 3 years. Guidelines 9) Maintenance of remission: Most patients with CD will require treatment for maintenance of remission. Systemic steroids including bedesonide are ineffective in maintenance of remission. The first line of treatment for maintenance of remission in patients with terminal ileal disease, colonic (L2), ileocolonic disease, extensive small intestinal disease, or localised ileocaecal disease is thiopurines. Methotrexate can also be used. Alternative to thiopurines can be anti-TNF therapy. Comments: •Spelling mistakes- Budesonide •Combined therapy with thiopurines and anti-TNF agents can also be used. •Too many ideas in the statements •The wording needs tweaking. The problem with longterm steroids is adverse-effects rather than efficacy in maintenance. This should be highlighted. Revised Mx: Statement 9 • Maintenance of remission: Most patients with CD will require treatment for maintenance of remission. • Systemic steroids including budesonide are ineffective in maintenance of remission. (EL 1, RG A) • The first line of treatment for maintenance of remission in patients with terminal ileal disease, colonic, ileocolonic disease, extensive small intestinal disease, or localised ileocaecal disease is thiopurines. (EL 1, RG 1) • Methotrexate can also be used. • Alternative to thiopurines can be anti-TNF therapy. (EL 3, RG C) Mx: Statement 10 • Patients on azathioprine need close monitoring. Some patients may be unduly sensitive and develop pancytopenia even with smaller doses. The dose should therefore be tailored to the individual. • Where ever available TMPT testing should be done prior to starting of azathioprine. AZATHIOPRINE 84% 6-THIOURIC ACID XO TPMT 6-MERCAPTOPURINE 6-METHYL MERCAPTOPURINE HGPRT IMPDH 6-THIOXANTHOSINE 5’- MP 6-THIOISONINE 5’- MP HGPRT TPMT GMPS 6-THIOGUANOSINE 5’- MP 6-METHYLTHIOINOSINE 5’-MONOPHOSPHATE MPK 6-THIOGUANOSINE 5’-DIPHOSPHATE DPK 6-THIOGUANOSINE 5’-TRIPHOSPHATE 6-THIOGUANOSINE NUCLEOTIDES Three enzymes: Competitive state TPMT • TPMT enzyme activity in general population: – Low or absent level (Homozygous): Approx 0.3% – Intermediate level: 11% – High level: 89% • only 25% of leukopenia: associated with the presence of one of genetic polymorphisms • Prospective studies evaluating dose optimization based on measurements of TPMT, 6-TGN, or 6-MP: Lacking • Despite the lack of such data, routine use of TPMT genotype or enzyme activity is currently recommended by the FDA before initiation of therapy with either AZA or 6-MP Monitoring • At initiation: – Complete blood count with differential every other week till dose is stablized. • Thereafter: At least once every 3 months. • Periodic LFT • FDA: – individuals should have TPMT genotype or phenotype assessed before initiation of therapy with AZA or 6-MP in an effort to detect individuals who have low enzyme activity (or who are homozygous defi- cient in TPMT) in an effort to avoid AZA or 6-MP therapy in these patients and thus avoid potential adverse events 10) Patients on azathioprine need close monitoring. Some patients may be unduly sensitive and develop pancytopenia even with smaller doses. The dose should therefore be tailored to the individual. Where ever available TMPT testing should be done prior to starting of azathioprine. Comments: •Should give guidance as to how we suggest the dose is tailored - lymphocyte count, MCV, thiopurine metabolites ... •Whether it is cost effective to test EVERYONE for TPMT is debatable. Agreed close monitoring is essential •TMPT may not be sensitive enough in some •"""...close monitoring of FBC and LFT, at least 1-2 weekly initially."" •""Educate patients to cease thiopurines in the event of allergic reactions.""" •TPMT test results do not have a defintie association with azathioprine adverse events •In addition, MRP4 testing and ITPase testing may be helpful for tailored medicine. •Reduceda •"Many substatements...not clear what we are voting for. •""Patients on azathioprine need close monitoring particularly to test for TPMT deficiency""....sounds more like what we are looking for" Revised Mx Statement 10 • Patients on thiopurines need close monitoring for myelotoxicity and hepatotoxicity. • More evidence of the benefit of TPMT testing in Asia is required. [III-C] Dose Mx: Statement 11 • Patients receiving systemic steroids for more than three weeks should receive calcium supplementation. Steroids and Bone • Effect of CS on bone modelling – – – – Impair osteoblast function, induce osteoblast apoptosis, reduce intestinal calcium absorption, increase renal excretion of calcium. • Increases risk of fracture • Greatest bone loss occurring in the initial months of treatment • Decrease in fracture risk back toward baseline after stopping glucocorticoid • Prednisone, prednisolone, and methylprednisolone: major • Budesonide, a locally acting corticosteroid, better Risk Factors for Glucocorticoid-Induced Osteoporosis Advanced age Low body-mass index (<24) Underlying disease: IBD, RA, SLE Prevalent fractures, smoking, excessive alcohol consumption, frequent falls, family history of hip fracture Glucocorticoid receptor genotype Increased 11β-HSD1 expression High glucocorticoid dose (high current or cumulative dose; long duration of therapy) Low bone mineral density Guidelines for management of glucocorticoidinduced osteoporosis Variable ACR NDF RCP(L) Dose & durn of ≥ 7.5mg/d for glucocorticoids atleast 3 mo ≥ 5 mg/d for atleast 3 mo Any dose for 9.3mg/day for atleast 3 mo atleast 3 mo Yearly BMD Yes Yes Yes Calcium suppl 1200-1500 mg/d 1200mg /d Only for pts For all with low Ca patients intake(<1g/d Vit D suppl 800-1000 IU vit D/d 2000 units of vit D/d vit D deficiency •ACR- American college of Rheumatology •NDF- National Osteoporosis Foundation •RCP(L)- Royal collage of Physicians of London •BBC- Belgian Bone club BBC Yes Survey of gastroenterologists' awareness and implementation of AGA guidelines on osteoporosis in IBD patients • 1000 physicians: Surveyed about awareness about implementation of guidelines on osteoporosis • Of 304 responders, 258 respondents were analysed. • 49% used guidelines in decision-making or in Mx • Physician saw more IBD pts more likely to do assess osteoporosis Mostwho of the responding physicians notforutilize compared to those who sawon lessmetabolic (P < 0.0001).bone disease in the AGA Guidelines • Only 16% who saw <25% IBD pts, treated osteoporosis (P < 0.0001). IBD patients. • Barriers: – IBD should be the focus of the visit (48, 42%); – osteoporosis should be managed by another physician: 30% – Lack of time: 11%) – Cost: 10. 9% – Lack of knowledge: 10, 9% Wagnon JH, Inflamm Bowel Dis. 2009 Do guidelines matter: Implementation of the ACG and AGA osteoporosis screening guidelines • ACG and AGA have both recently issued guidelines • 100 IBD patients underwent DEXA • Indications for screening – Prolonged past or concurrent steroid use (92%), – Postmenopausal status (7%), – History of low trauma fracture (7%). • • • • 42% had osteopenia 12% had osteoporosis 44% had normal BMD Factors predicting a greater likelihood of osteoporosis – Diagnosis of Crohn's disease – Low body mass index in women, and postmenopausal status. • Implementation of the Guidelines led to the detection of osteopenia or osteoporosis and initiation of specific therapies in a majority of patients Kornbluth A, Am J Gastroenterol. 2006 11) Patients receiving systemic steroids for more than three weeks should receive calcium supplementation. Comments: •And vitamin D status should be measured and replaced if deficient. Perhaps referring the reader to local osteoporosis guidelines would be best as well. There may be times where bisphosphanates are commened early. •?and vitamin D or variable within the region. •"Now, Ca and Vit D supplementation to avoid osteoporosis are not 1st choice in general population. •Bisphosphonate or Vit K are recommended. •So, even in IBD, we do not have enough evidence that Ca supplementation is effective. " •Calcium supplements should be given even if steroids are given for less than 3 weeks •=+Vit D + shot with steroids Revised Mx: Statement 11 • Patients receiving systemic steroids should also be prescribed calcium supplementation and vitamin D. III-C • ** Check level of evidence Mx: Statement 24 • At present, there is no definite role of antimycobacterial avium para-tuberculosis therapy in patients with CD. Isolation of MAP in pts with CD Country Method CD UC Healthy control control 2010 Mendoza Spain Blood Culture (MGIT) 18-m0 0/30 0/29 0/10 2009 Kirkwood Australia BACTEC 12B 4/10 (40%) 0/2 0/4 2009 Reddy DN India PCR-IS900 0/81 0 0/85 Maryland USA BACTEC 460 0/130 0 0/130 4/5 (80%) 0 0/130 19/30 (63.3%) 0/2 10.3% Year, Author 2009 Parrish NM 2008 Singh AV 2005, Sechi21 PCR-IS900 India Italy MGIT Tissue culture Isolation of MAP in pts with CD Year, Author Country Method Pts with CD 2004, Naser20 USA Lancet Blood culture 14/28 (50%) (MGIT) 2/9 (22%) 2003, Bull TJ19 UK, JCM Tissue culture (MGIT) 14/33(42%) (after 14-88 wks) 3/33(9%) 2000, Schwartz Clin Micro Infect Culture MGIT Surgical sp 6/7 (86%) 4/20 (20%) 2/36 (5.6%) 2000 Collins48 USA (JCM) BACTEC 12B 0 0 1993 Wall S49 UK (JCM) 6/30 UC control Healthy control Comments 0/15 MAP lies in submucosa 0 None positve Identified by DNA MAP (As detected by PCR) Meta-analysis Anti-MAP therapy in patients with CD Author (year) Pts Trial Antibiotic combination Concom steroid TT (mos) Primary endpoints Efficacy (main result): Treatment/placebo (%) Elliott (1982) 51 RCT Sulfadoxine, No pyrimethamine 12 Changes in CDAI scores Clinical remission: 38/50 Schaffer (1984) 27 RCT Ethambutol, rifampin No 12 Changes in CDAI scores (or any clinical indicator of disease activity) Clinical remission: 36/64 Basilisco (1989) 24 RCT Rifabutin No 6 Changes in the HarveyBradshaw index Clinical remission: 29/38 Hampson (1989) 20 Open label Ethambutol, rifampin, isoniazid, Yes clofazimine (or pyrazinamide) 9 Clinical remission defined as CDAI < 150 Clinical remission: 50 Prantera (1989) 5 Open label Dapsone No 1 Changes in CDAI scores and Clinical remission: 40 mucosal healing Afdhal (1991) 49 RCT Clofazimine Yes 12 Clinical remission (use of modified CDAI scores) Clinical remission: 64/50 Anti-MAP therapy in patients with CD Author (year) Rutgeerts (1992) Pts 16 Prantera (1994) 40 Swift (1994) Thomas (1998) Trial Antibiotic combination Efficacy (main result): Treatment/placebo (%) Concom steroid TT (mos) No 6–12 Endoscopic healing in the neoterminal ileum Mucosal healing: 0 9 Clinical remission and mucosal healing Clinical remission: 84/35 24 Changes in the Harvey-Bradshaw index and CDAI scores, steroid sparing, need for surgery, radiological change Clinical remission: 35/38 Induction of clinical remission: 93.5 Clinical remission: 32/48 Open label Rifabutin, ethambutol RCT Clofazimine, rifampin Yes Primary endpoints 126 RCT Ethambutol, rifampin, isoniazid Gui (1997) 46 Open label Rifabutin, clarithromycin (or azithromycin) Yes 19 Changes in the Harvey-Bradshaw index and serum CRP, steroid sparing, need for surgery Leiper (2000) 25 Open label Clarithromycin Yes 1–15 Changes in the Harvey-Bradshaw index and serum CRP No Goodgame (2001) 31 RCT Clarithromycin, ethambutol Yes 3 Changes in the Changes in the lactulose-mannitol Harvey-Bradshaw test and the Harvey-Bradshaw index in the active index arm: P = .08 vs placebo Shafran (2002) 36 Open label Clarithromycin, rifabutin Noa 4–17 Response defined as marked improvement in CDAI scores Clinical response: 58.3 Borody (2002) 12 Open label Clarithromycin, Yes rifabutin, clofazimine 24 Changes in the Harvey-Bradshaw index Clinical remission: 25 Anti-MAP therapy in CD • Induction phase – Oral prednisolone 40 mg/day, taper to 0 over 16 weeks, • Randomization: Either antibiotic combo or placebos from wk 1 – Clarithromycin 250 mg/d for wk 1, 250 mgx2 for wks 2 &3then 750 mg/d from wk 4. – Rifabutin dose increased at the same time points 150 mg, 300 mg, and 450 mg. – Clofazimine 50 mg daily. • Subjects were stratified for use of thiopurine therapy. • Subjects not achieving remission at wk 16 and those unable to tolerate full doses of were considered Rx failures, withdrawn. • Maintenance phase – Subjects in remission at week 16 continued trial medications. – If a subject had a subsequent relapse (CDAI >150 with an increase ≥60), retreated with “rescue” prednisolone. – Failure to respond to this retreatment was an indication for withdrawal. • Follow-up phase – At 104 wks, the trial medications were ceased. – Selby W, Gastroenterology 2007 (Sydney Au) Result: Primary outcome measure Relapse Antibiotic Placebo 1 relapse, 16-52 wk 39% (26/67) 56% (31/55) (P = .054; OR, 2.04 [95%CI: 0.84–4.93] Wk 104 26% (11/42) 43% (12/28 (P =0 .14; OR, 2.22 [95%CI: 0.62–7.96] Wk 156 59% (20/34) 50% (10/2 (P = .54; OR, 0.70 [95%CI: 0.18–2.74]. Remission at 3 yrs 14 (13.7% 10 (9.0% Summary: Anti-MAP therapy in CD • Insufficient evidence • Many limitations • Anti-MAP therapy: Not known – The drugs, How many – How long – What doses • In-sufficient evidence to recommend ati-MAP therapy in CD 24) At present, there is no definite role of anti-mycobacterial avium para-tuberculosis therapy in patients with CD. Comments: NIL Revised Mx: Statement 24 • At present, there is no definite role of antimycobacterial avium para-tuberculosis therapy in patients with CD. [I-A] Text: drug dose efficacy duration. Mx: Statement 25 • Medication use Fertility, pregnancy, breast feeding, nutrition and osteoporosis are important considerations in the management of CD. Pregnancy outcome in CD 13 studies comparing the pregnancy outcomes in IBD. 12 included (1986 and 2005) 3907 patients with IBD and 320531 controls. 63% CD and 36% UC Outcome of interest studies Pts Control OR (95% CI) LBW 2 597 3357 2.82 (1.42 to 5.60) Premature birth 7 1005 61565 1.97 (1.36 to 2.87) Still births 3 589 3558 1.91 (0.69 to 5.31) SGA 2 220 1373 5.72 (0.62 to 52.81) Caesarean section 4 321 57935 1.65 (1.19 to 2.29) Cong abnormalities 3 307 1712 2.14 (0.97 to 4.74) p Value 0.003 <0.001 0.22 0.12 0.003 0.06 Cornis J, Gut 2007 Effect of drugs for IBD in pregnancy Outcomes 5‐ASA AZA CS Anti‐TNFα pop incidence (%) Studies Women Pregnancies Successful pregnancies Spontaneous abortion Elective termination Still births LBW Premature birth Ectopic pregnancy Major congenital defect 14 3 4 2 . 1026 37 883 106 . 648 39 581 92 . 612 (94) 33 (84) 124 (94) 65 (70) . 16 (2.4) 1 (2) 2 (<1) 11 (12) 20 7 (1) 2 (5) 0 16 (17) 0.02 4 (<1) 0 1 (<1) 0 <1 4 (<1) 1 (3) 4 (3) 1 (1) 7.6 7 (1) 5 (15) 3 (2) 3 (5) 6 1 (<1) 0 0 0 1 14 (2.4) 2 (3) <1 10 (1.5) 2 (6) Food and drug administration categories Class Risk A B C Controlled studies show no risk No evidence of risk in human Risk cannot be ruled out, animal studies showed adverse effects on fetus Positive evidence of risk in humans, risk/ benefit ratio should be considered contraindicated D X Nursing and disease activity • Detriment to maternal health secondary to nursing after delivery is controversial. • A few reports: associations between nursing and increased disease activity, (whether related to disease course or cessation of medication) • Population based study: – No increased risk of flare during breastfeeding (Moffatt [39] • OR 2.2 (95% CI: 1.2-2.7) of disease flare for women who breastfeed compared to those who did not ( Kane et al[31]) Breast feeding in CD Few data and advice is based on anecdotes Drug Safety Sulfasalazine sulfapyridine moiety is absorbed in minimal amounts and is excreted in milk, but the milk: serum ratio is low Safe Mesalamines Confirmed in many prospective trials Safe Prednisone Detected in breast milk To minimise exposure, a 4-hour delay after oral dosing AZA/6-MP Undetectable or in nanomolar conc Acceptable IFX Not detected in breast milk Acceptable Metro/Cipro Excreted in milk Unsafe As with all drugs, discuss carefully and individually Osteoporosis and osteopenia in IBD • Prevalence of osteopenia: 22-77% • Prevalence of osteoporosis: 17%-41%,. Osteopenia and osteoporosis common in IBD Mean calcium intake was <200 mg/day in almost 90% Significantly lower values of BMD at the spine and hip in both UC and CD as compared with Indian healthy controls. 29 (63%) and 21 (45.6%) patients had either osteopenia or osteoporosis at the spine and hip region, respectively. AIIMS, Ind J Gastroenterol, 2008 Avoidance of milk and milk products is a Myth Calcium supplementation • Must whenever steroids are used for more than 2 weeks Nutrition and osteoporosis are important considerations in the management of UC. [III,B] 25) Fertility, pregnancy, breast feeding, nutrition and osteoporosis are important considerations in the management of CD. Comments: •what is the focus here? Revised Mx: Statement 25 • Nutrition and osteoporosis are important considerations in the long term management of CD. • Medication use and surgical options should take into consideration fertility, pregnancy and breastfeeding. • [III-C]