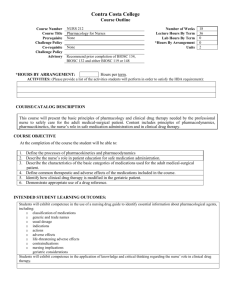
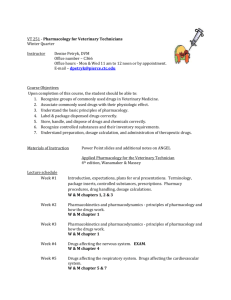
ST210_PrinciplesofSurgicalPharmacology_BB

Principles of Surgical
Pharmacology
ST210
Concorde Career College
Principles of Surgical
Pharmacology
History of Pharmacology
Objectives:
• Define the term pharmacology
• Provide a timeline of the events leading up to modern pharmacologic practice
• Perform basic mathematical calculations to allow conversion between the various measurement systems and correct drug dosages
Definition
Pharmacology = the study or science of drugs
Root derived from Greek terms farmakon (drug) and logy (science or study of)
Definition
• Drug
– Substance used as medicine for the diagnosis, treatment, cure, mitigation, or prevention of disease or a condition
Definition
Pharmacology concepts include:
• Composition (properties)
• Uses (medical mechanism of action)
• Effects (characteristics)
Related Definitions
Pharmacologist = one who has knowledge of drugs and the art of drug preparation (usually works in a research setting)
Pharmacist = health professional educated in the art of preparing and dispensing drugs (usually works in a hospital or retail pharmacy)
History of Pharmacology
Prehistoric – Accidental discoveries
Evidence of prehistoric healing arts is obtained from:
Wall Paintings
Carvings
Burial sites
History of Pharmacology
Ancient – Known drugs and healing techniques were utilized along with magic, religion, and rituals
Use of drugs systematically recorded as evidenced by
Egyptian Papyri, Cuneiform
Medical Tablets, and
Chinese inscriptions
History of Pharmacology
Classical – First pharmacies
• Hippocrates (Father of
Medicine) – Hippocratic
Oath developed during this period
• Galen (incorrect anatomical descriptions unchallenged for 1500 years) – Introduced minerals to pharmacology and began to soak, boil, and mix the preparations creating syrups, tinctures, etc.
History of Pharmacology
Middle Ages – New (sweet) formulations
• Greek and Roman
Asia
• Islamic physician Ibn Sina (aka
– Avicenna) made impressive additions to the works of
Galen and Dioscorides (Turkish physician – educated in Greece
– wrote the first text on botany and pharmacology that was free from superstition called the De Materia Medica
“on medical matters”)
History of Pharmacology
Renaissance – The age of enlightenment
• Advances in metallurgy and chemistry
History of Pharmacology
New World – Spanish exploration led to the introduction of Central and
South American remedies to the Europeans. Some of the medicines are still in use today (e.g., ipecac, nicotine, hallucinogenics, cocaine, and quinine – used to treat malaria).
History of Pharmacology
Modern – Pharmacology as an individual science/legislation developed (standardization)
Principles of Surgical
Pharmacology
Mathematical Calculations and
Conversions
Objectives:
• Perform basic mathematical calculations to allow conversion between the various measurement systems and correct drug dosages
Measurements/Conversions
• Refer to the Metric Conversion Charts,
Appendix C on Pages 1206-1207 of Surgical
Technology for the Surgical Technologist: A
Positive Care Approach, 4 th Edition
Measurements/Conversions
• Important calculations
– Concentration: ratio of solute to solvent
– Dose: overall amount of medication delivered to the patient
– Application: medication’s use in the surgical setting
Calculating Medication Dosages
• Concentration
– Convert solute to solvent
• A:B = C:D
• Cumulative dose
– Calculated by taking the amount of solution delivered and multiplying it by the amount of solute from the ratio above
Percentages
• Characteristics of a percentage
– Represents a fraction in which the denominator is always 100
– Expressed as a whole number followed by the percent symbol (%)
– Can also be expressed as a decimal by moving the decimal point two places to the left of the written number to indicate hundredths
Conversion of Temperature
• Scales used to measure temperature
– Fahrenheit and Celsius
• Monitoring body temperature is important
– If not in normal range, surgical procedure may be delayed or canceled
– Hypothermia is a concern intraoperatively
– Certain anesthetic agents affect the thermoregulatory centers in the brain, leading to the body’s inability to adapt to temperature changes
Units of Measure
• Metric system
– Based on powers or multiples of 10
• Value of numbers established by the use and placement of a decimal point to indicate whole numbers versus fractions
• Metric, household, and apothecary systems of measurement
– Household: refer to text for abbreviations
– Apothecary system: based on weight of a grain of wheat
Weight Conversions Practice
1.5g = 1500 mg
52 lb = 23.64 kg
46 kg = 101.2 lb
78 kg = 171.6 lb
500 mg = 0.5 g
4000 g = 4 kg
Weight Conversions Practice
5 g = 5000 mg
240 lb = 109.09 kg
300 mg = 0.3 g
2 g = 2000 mg
220 kg = 484 lb
175 lb = 79.55 kg
Length Conversions Practice
1 m = 39.38 inches
1 inch = 2.54 cm
4 cm = 1.6 inches
10 cm = 4 inches
12 inches = 30 cm
Length Conversions Practice
30 cm = 12 inches
6 inches = 15.24 cm
1 yard = 36 inches
Volume Conversions Practice
1 ml = 1 cc
4 cc = 4 ml
2 oz = 60 cc
5 liters = 5000 cc
1.5 liters = 1500 ml
Volume Conversions Practice
0.5 oz = 15 ml
500 cc = 0.5 L
0.75 L = 750 cc
1 gallon = 4000 cc
12 ml = 0.41 oz
15 gtt or minims = 0.6 cc
Temperature Conversions
(textbook method = fractions – eeeewwww!!!!)
Convert Fahrenheit to Celsius
°
C = (
°
F – 32) 5/9
Which means:
1. Subtract 32 from
°
F
2. Multiply by 5
3. Divide by 9
Temperature Conversions
(textbook method = fractions - eeeewwww!!!!)
Convert Celsius to Fahrenheit
°
F = (
°
C x 9/5) + 32
Which means:
1. Multiply
°
C by 9
2. Divide by 5
3. Add 32
Temperature Conversions
(another method = no fractions – WOW!)
• Convert Fahrenheit to Celsius
(
°
F - 32) x 0.56 =
°
C
• Convert Celsius to Fahrenheit
(
°
C x 1.8) + 32 =
°
F
Temperature Conversions Practice
36 ° C = 96.8
° F
32 ° F = 0 ° C
98.6
° F = 37.3
° C
100 ° C = 212 ° F
18 ° C = 64.4
° F
Temperature Conversions Practice
101º F = 38.64º C
104º F = 40.42º C
212º F = 100º C
37.7º C = 99.86º F
91.4º F = 33.26º C
Basic Conversions
1. 1 g = 1000 mg
2. 1 kg = 2.2 lb
3. 1 cc = 14-15 minims
4. 1 L = 1000 cc
5. 212º F = 100º C
– Boiling Point of Water
Basic Conversions
6. 1 minim = 1 gtt
7. 1 ounce = 30 cc
8. 98.6º F
9. 100 ml
10.1 meter
=
=
=
37º C
100 cc
100 cm
Abbreviations Related to Medication
Administration
• Medication errors have been attributed to the use of abbreviations
– The Joint Commission—Official “Do Not Use” List
• Refer to Table 9-11
Principles of Surgical
Pharmacology
Drug Classifications, Types, and
Administration
Objectives
• Discuss drug classifications and provide examples
• Identify the five main drug sources and provide examples of drugs from each source
• List and describe drug forms
Objectives
• Differentiate between the three types of drug nomenclature
• List and describe drug administration routes
Medication Information
• Basic information
– Names
– Classifications
– Actions
– Indications
– Dosage
Legal Drug Classifications
• Controlled substances
– Drugs with a high potential to cause psychological and/or physical dependence and abuse
• Prescribed medications
– Medications that, if used inappropriately, could cause significant harm to the patient
Controlled Substances
• Controlled Substances (special prescription)
– Schedule or Class I
– Schedule or Class II
– Schedule or Class III
– Schedule or Class IV
– Schedule or Class V
Legal Drug Classifications (cont’d.)
• Over-the-counter (OTC) medications
– Prepared in a dosage that are safe to administer without the direction of a physician
• Alternative medications
– There are limited studies to determine the safety and effectiveness of these therapies, resulting in a limited understanding
Drug Classifications
• Chemical type
• Body system affected
• Physiological action
• Therapeutic action
Classifications
1. Analgesic
2. Anesthetic
Relieves pain
Loss of sensation
3. Antibiotic Prevent/treat infection
4. Anticholinergic Block parasymp. impulses
5. Anticoagulant Prevents blood clotting
Classifications
6. Antiemetic
7. Antiinflammatory prevents N&V decrease swelling
8. Antipyretic decrease fever
9. Controlled substance narcotic
10.Contrast media X-ray delineation
11.Cycloplegic
12.Diuretic
13.Dye
14.Fibrinolytic
15.Hemostatic
Classifications
Paralyze ciliary
Increase urine
Color tissue
Dissolve clot
Clot formation
Classifications
16.Hormone
17.Miotic
18.Mydriatic
19.Sedative
Endocrine secretion
Constrict pupil
Dilate pupil
Reduce anxiety
20.Vasoconstrictor Increase BP
Medications in the Operating
Room
• Common pharmacologic agents used in the
OR setting
– Refer to Table 9-13
• Medications used by the anesthesia care provider as part of the anesthesia delivery
– Refer to Table 9-20
Medications for Use with Specific
Surgical Specialties
• Include:
– Obstetric and gynecologic surgery: oxytocics, vasopressin, and immunoglobin
– Orthopedic surgery: antibiotics, hemostatic agents, and steroids
– Cardiovascular surgery: heparinized saline solution
Medications for Use with Specific
Surgical Specialties (cont’d.)
– Neurosurgery: antibiotics, heparinized saline solution, contrast media, lidocaine HCl injection or absorbable gelatin sponge soaked in thrombin, and polifeprosan 20 with carmustine implants
– Ophthalmic surgery: Refer to Table 9-14
Drug Descriptions
1. Lidocaine
2. Dantrolene
Antidysrhythmic/anesthesia
Treat MH
3. Epinephrine Vasoconstrictor
4. Benzodiazepine Sedative
5. Atropine Anticholinergic
Drug Descriptions
6. Nitrous oxide
7. Heparin
8. Thrombin
9. Mannitol
10.Bacitracin
Anesthetic (gas)
Anticoagulant
Topical hemostatic
Osmotic diuretic
Antibiotic
Drug Identification
Adrenalin = epinephrine = vasoconstrictor
Ancef = cefazolin sodium = antibiotic
Anectine = succinylcholine chloride = depolarizing NMB
Benadryl = diphenhydramine = antihistamine
Coumadin = warfarin sodium = anticoagulant
Dantrium = dantrolene sodium = MH antagonist
Decadron = dexamethasone = steroidal antiinflammatory
Demerol = meperidine HCl = narcotic analgesic
Drug Identification
Flagyl = metronidazole = anti-fungal/amebic/protozoal
Gelfoam = absorbable hemostatic gelatin sponge = hemostatic
Heparin = heparin sodium = anticoagulant
Humulin = insulin, human = hormone
Kantrex = kanamycin sulfate = antibiotic
Lasix = furosemide = loop diuretic
Marcaine – bupivacaine HCl = anesthetic (amino amide)
Drug Identification
Narcan = naloxone hydrochloride = narcotic antagonist
Papaverine = papaverine HCl = vasopressor/vasodilator
Pentothal sodium = thiopental sodium = anesthetic (induction agent)
Pitocin = oxytocin = hormone
Renografin = diatrizoate meglumine, diatrizoate sodium = contrast
Silvadene = silver sulfadiazine = antiinfective sulfonamide
Solu-Cortef = hydrocortisone sodium succinate = steroidal antiinflammatory
Sublimaze = fentanyl citrate = narcotic analgesic
Drug Identification
Surgicel/Oxycel = oxidized cellulose = hemostatic agent
Tagamet = cimetidine = antacid/H2 Blocker
Toradol = ketorolac tromethamine = NSAID/nonnarcotic analgesic
Tracrium = atracurium besylate = nondepolarizing NMB
Valium = diazepam = sedative tranquilizer/benzodiazepine
Versed = midazolam HCl = sedative tranquilizer/benzodiazepine
Wydase = hyaluronidase = enzyme/local anesthesia agonist
Xylocaine = lidocaine = anesthetic/cardio (amino amide)
Drug Sources
1. Plants
2. Animals
3. Minerals
4. Laboratory synthesis
5. Biotechnology
1. Gas
2. Liquid
3. Solid
Drug Forms
• Chemical
• Generic
• Brand
Drug Nomenclature
Routes of Administration
• Enteral
• Topical
• Inhalation
• Parenteral
Principles of Surgical
Pharmacology
Pharmacodynamics &
Pharmacokinetics
Objectives
• Define the term pharmacokinetics and outline the process of pharmacokinesis
• Define the term pharmacodynamics and describe the three aspects of pharmacodynamics
Pharmacokinetics
Pharmacokinetics is the entire process of the drug within the body.
• Absorption
• Distribution
• Biotransformation
• Excretion
Pharmacokinetics
Absorption
• Drug must be absorbed to produce an effect
• Absorption occurs at the site of administration
(where it is absorbed into the bloodstream by the capillaries)
Pharmacokinetics
Absorption (continued)
Absorption occurs in one of two ways.
1. Passive transport
2. Active transport
Pharmacokinetics
Absorption (continued)
Passive transport – Substance is moved from an area of higher concentration to an area of lower concentration until concentration on both sides of the membrane is equal.
• Passive transport requires no energy.
• Most drugs are absorbed in this manner.
Pharmacokinetics
Absorption (continued)
Active transport – Required for some drugs, glucose, and amino acids (building block of proteins).
• Requires energy in the form of ATP (a cation such as sodium) to carry the substance from the area of lower concentration to an area of higher concentration.
Pharmacokinetics
Absorption (continued)
Rate of Absorption – Affects the final drug action
(pharmacodynamics) and is influenced by several factors.
• Type of drug preparation
• Dosage
• Route of administration
• Patient’s condition
Distribution
Pharmacokinetics
Transport of the drug substance to the target cells once it enters the circulatory system.
Pharmacokinetics
Distribution (continued)
Distribution of the drug is affected by several factors.
• Rate of absorption
• Cardiovascular function (systemic circulation)
• Regional blood flow (perfusion) to the target organ or tissue
• Drug is carried to all parts of the body; may result in effects other than intended
• Also affected by plasma protein binding, tissue binding, and barriers (placenta/blood-brain)
Pharmacokinetics
Biotransformation
Biotransformation = Metabolism
• Most often occurs in the liver; however other tissues such as intestinal mucosa, lungs, kidneys, and blood plasma may be involved.
• A few drugs are converted into active substances by the liver.
Pharmacokinetics
Biotransformation (continued)
The main function of the liver in metabolism is to break down the drug molecules with enzymes for excretion. The breakdown products of metabolism are called metabolites.
Metabolites are smaller, less active, or inactive substances
Pharmacokinetics
Biotransformation (continued)
The hepatic first pass effect must be considered when planning drug dosage and route of administration.
Hepatic First-Pass Effect
Hepatic Portal System
Ingested items must pass through the hepatic portal system. The portal vein receives blood vial the tributaries from the capillaries of the abdominal viscera when then drains into the hepatic sinusoids.
Pharmacokinetics
Excretion
• The effect of the drug continues until it is biotransformed or excreted.
• Drugs are removed from the target organ
(intact or biotransformed) by the circulatory system.
Pharmacokinetics
Excretion (continued)
The kidneys (with subsequent elimination in the urine) are primarily responsible for excretion.
Drug substances may also be eliminated in the feces, sweat, saliva, exhaled, or in breast milk posing a possible danger to the nursing baby.
Pharmacodynamics
• Pharmacodynamics is the interaction of the drug molecules within the target cells.
• Drug action causes an alteration in physiological activity, but is incapable of initiating new function.
• Drugs are administered to produce an expected or therapeutic effect.
Pharmacodynamics
Types of drug actions:
• Inhibition or destruction of foreign organisms
• Inhibition or destruction of foreign malignant cells
• Protection of cells from foreign agents
• Supplementation or replacement of hormones, vitamins, and/or enzymes
• Increasing or decreasing the speed of a physiological function
Pharmacodynamics
Three aspects (time and dosage related) of pharmacodynamics:
1. Onset
2. Peak effect
3. Duration of action
Pharmacodynamics
Onset – Time that it takes from administration of the drug for its action to become evident.
Pharmacodynamics
Peak effect – Period of time during which the drug is at its maximum effectiveness.
Pharmacodynamics
Duration of action – Time between onset of action to the cessation of action.
Note: Timing of future dosing depends on the three aspects of pharmacodynamics. Certain variables such as type of drug, dosage, route of administration, and patient condition must also be considered when planning future doses.
Pharmacodynamics
Three theories that may explain the ways that drugs produce their effects.
1. Drug receptor interaction
2. Drug enzyme interaction
3. Nonspecific interaction
Pharmacodynamics
Drug receptor interaction – The active substance in the drug has an affinity for a specific chemical constituent of a cell. The interaction occurs on a molecular level on the cell surface or within the cell.
Pharmacodynamics
Drug enzyme interaction – A drug may combine with a specific enzyme to inhibit the action of the enzyme or alter the cellular response to the enzyme.
Pharmacodynamics
Nonspecific interaction – Drug accumulates on the cell membrane or penetrates the membrane and interferes physically or chemically with a cellular function or metabolic process.
Side Effects
Side effects are undesirable consequences along with the therapeutic responses to the drug.
Side effects are:
• Expected
• Predictable
• Unavoidable
• Usually tolerable or treatable
Iatrogenic Response
An iatrogenic response is a type of serious unavoidable side effect or disease induced by pharmacological therapy.
Iatrogenic Response
There are five syndromes associated with iatrogenic responses:
1. Blood abnormalities
2. Liver toxicity
3. Kidney toxicity
4. Teratogenic (causing abnormal prenatal development)
5. Dermatologic
Adverse Effects
Adverse (idiosyncratic) effects are also undesirable consequences along with the therapeutic responses to the drug.
• Unintended
• Usually unpredictable (certain factors such as age, weight, time of administration may allow predictability)
• Usually unavoidable
• May be tolerable or treatable
Tolerance
Tolerance is a decreased therapeutic response to a drug following repeated administrations causing the dose to be increased to maintain the therapeutic effect.
Addiction
Addiction is physical or psychological dependence on a specific agent with an increasing tendency to its use or abuse.
Drug Interactions
Drug interactions may occur when two or more substances are prescribed concurrently, causing a modification of action of one or more of the substances.
• May be intentional (beneficial)
• May be undesirable (detrimental)
• Drug interactions are categorized as agonistic or antagonistic.
Drug Interactions
• Agonist – A drug that potentiates or enhances the effect of another.
• Antagonist – A drug that blocks the action of another.
Note – Agonists and antagonists produce no action of their own.
Principles of Surgical
Pharmacology
Drug Handling
Objectives
• List and describe federal and state drug regulations
• List the six “rights” for correct drug handling
• List and describe methods for identification of medications
• Understand medication handling techniques utilized in the surgical environment
Drug Standards and Forms
• Drug standards
– Medications in the U.S. are required to undergo review and approval by the FDA
• Refer to Table 9-3
• Drug forms
– Several forms of preparation
• Refer to Table 9-4
Drug-Handling Techniques
• Drug safety is of utmost concern to all involved
– Know the pertinent state and federal laws
– Know the policies and procedures of the health care facility
• The Six “Rights” of Medication Administration
– Refer to Table 9-12
Drug Handling Techniques
Six “RIGHTS” for correct drug handling:
1.
Right PATIENT
2.
Right DRUG
3.
Right DOSE
4.
Right ROUTE OF ADMINISTRATION
5.
Right FREQUENCY
6.
Right DOCUMENTATION
Medication Identification
• Common container types
– Refer to Figures 9-1 and 9-2
• Medication labels
– Refer to Figure 9-3
• See text for an example of:
– The steps of administration
– The interactions that occur between the circulator and the surgical technologist during transfer
Medication Identification
Packaging
• Ampule
• Vial
• Preloaded syringe
• Tube
Medication Identification
Ampule
Medication Identification
Vial
Medication Identification
Preloaded Syringe
Medication Identification
Tube
Medication Identification
Labeling
• Drug Name (trade and generic)
• Manufacturer
• Strength
• Amount
• Expiration Date
• Route of Administration
• Lot Number
• Handling (storage/warnings)
• Controlled Substance Classification
Medication Identification
When obtaining drugs and transferring them to the sterile field…
IDENTIFY each drug THREE TIMES
• First identification/verification
• Second identification/verification
• Third identification/verification
Medication Identification
How is the accomplished on the sterile field?
• Preprinted labels (stickers)
• Preprinted plastic markers
• Marking pen and blank label or tape
EACH LOCATION OF THE MEDICATION MUST BE
LABELED!
Syringe Anatomy
A. Needle
B. Luer-Loc Tip/Hub
C. Barrel
D. Rubber Stopper
E.
Plunger
Note: Flange
Needle Anatomy
A. Plastic Sheath
B. Bevel
C. Lumen
D. Point
E.
Lumen
F.
Shaft
G. Hilt
H. Hub