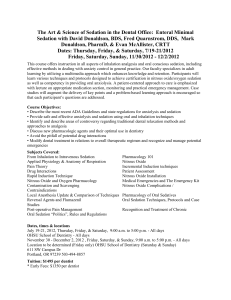
Conscious Sedation [PPT]
advertisement
![Conscious Sedation [PPT]](http://s3.studylib.net/store/data/009459180_1-1f61bc644aa9d1b1fc24be3a2167e194-768x994.png)
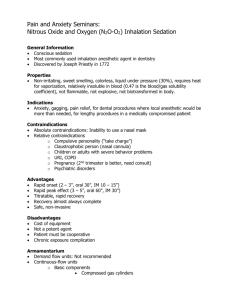
PRESENTED BYSUVIDHA SETH III YEAR HISTORY INTRODUCTION DEFINITIONS AIMS & OBJECTIVES OF CONSCIOUS SEDATION PREREQUISITIES FOR SEDATION ANATOMIC & PHYSIOLOGICAL DIFFERENCES(CHILD/ADULTS) INDICATIONS & CONTRAINDICATIONS PATIENT ASSESSMENT & PREPARATION LEVELS OF SEDATION & GA DRUGS USED FOR CONSCIOUS SEDATION AAP / AAPD GUIDELINES CONCLUSION REFERENCES To perform the highest quality dental care in pediatric patients, the practitioner may need to use pharmacologic means to obtain a quiet, cooperative patient. Techniques that use drugs to induce a cooperative yet conscious state in an otherwise uncooperative child are most commonly referred to as techniques of conscious sedation. Before the middle of 19th century many agents like alcohol were used to obtund surgical pain, but operations were horrible ordeals. Dr. Horace Wells (Dentist & Discoverer of Anesthesia), used NITROUS OXIDE (N2O) from a demonstration of laughing gas(1844). However he often failed to relieve dental pain completely & its use had to wait. Dr. W. Morton (1846),dentist at Boston , successfully used ETHER for extraction of a tooth & it became very popular. CHLOROFORM was used by Simpson,(1847), for Obstetrical purposes & despite its toxic potential, became a very popular surgical anesthetic. Nitrous oxide was not used until 1863,when Colton reintroduced the gas into dentistry. In 1868,Andrews,an American physician , introduced the combined use of nitrous oxide & oxygen inhalation. CONSCIOUS SEDATIONA minimally depressed level of consciousness, that retains the patient’s ability to maintain an airway independently & respond appropriately to physical stimulation & verbal commands. (AMERICAN DENTAL ASSOCIATION,1993) CONSCIOUS SEDATION (Old Terminology)Now called as MODERATE SEDATION Moderate Sedation-Analgesia: A drug-induced depression of consciousness during which patients respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. This includes— Airway is patent, & spontaneous ventilation is adequate. Cardiovascular function is usually maintained. Reflex withdrawal from a painful stimulus is not considered a purposeful response. (AAP/AAPD GUIDELINES,2006) ANXIOLYSIS (old terminology) Now called as MINIMAL SEDATION A drug-induced state during which patients respond normally to verbal commands. Cognitive function & coordination may be impaired. Ventilatory and cardiovascular functions are unaffected. (AAP/AAPD Guidelines 2006) DEEP SEDATIONA drug induced depression of consciousness during which patients cannot be easily aroused but respond purposefully after repeated verbal or painful stimulation. (AAP/AAPD Guidelines 2006) The ability to independently maintain ventilatory function, may be impaired. Patients may require assistance in maintaining a patent airway. Cardiovascular function is usually maintained. A state of deep sedation may be accompanied by partial or complete loss of protective airway reflexes. GENERAL ANESTHESIAA controlled state of unconsciousness, accompanied by partial or complete loss of protective reflexes, including inability to maintain an airway independently & respond purposefully to physical stimulation or verbal command. (AMERICAN DENTAL ASSOCIATION,1993) Guard the patient’s safety and welfare 2. Minimize physical discomfort and pain 3. Control anxiety, minimize psychological trauma 4. Maximize the potential for amnesia 5. Control behavior and movement to allow the safe completion of the procedure 6. Return the patient to a state in which safe discharge from medical supervision, as determined by recognized criteria.(AAP 2006) These goals can best be achieved by selecting the lowest dose of drug with the highest therapeutic 1. 1. 2. 3. The practitioner should have knowledge of the agents to be used & should be trained for their administration. There should be a well-documented informed consent by parent/guardian who has had a consultation on the alternatives & risks. There should be no lack of equipment to complicate the management of an emergency. There should be carefully planned rationale for use of sedation which is based onbehavior of patient, nature & extent of treatment required, risk-to-benefit ratio, capability of family to meet the demands of an extensive treatment plan & ◦ the economic feasibility. ◦ ◦ ◦ ◦ Mobile emergency medical services should be readily available. 1. 2. Difference in BASAL METABOLIC RATE. Greater in children, which ultimately affects not only the drug response, but also important physiologic parameters. Difference in RESPIRATORY RATE. Because oxygen demand is greater, but the alveolar system is less mature, the respiratory rate is far higher in children than adults. So, it must be considered when giving drugs that depress the respiratory system. 3. AIRWAY MANAGEMENT is different because of anatomic variations. The narrow nasal passages, glottis, hypertrophic tonsils & enlarged tongue produce a much greater risk of airway obstruction. The airway of all patients should be examined prior to sedation. Patients with tonsillar tissue that occupies more than 50% of pharyngeal space are at an increased risk of respiratory obstruction. Classification of tonsil size should be completed for all patients prior to sedation. Patients classified as +3 or greater (having more than 50% of the pharyngeal area occupied by tonsils) are at increased risk of developing airway obstruction. Cote CJ et al. A practice of anesthesia for infants and children, Philadelphia, 1993, WB Saunders, pp 313-314. Children demonstrate a reduced tolerance to respiratory obstruction. Thus, sudden APNOEA is a great concern in pediatric age group. Because thorax is smaller, with less expansion capability & children have less functional reserve. So, are prone to rapid obstruction or respiratory depression. For this reason children with sleep apnea are not good candidates for conscious sedation. 4. CARDIOVASCULAR parameters are different for children. The heart rate is faster and blood pressure is lower than in the adult. Children are more susceptible to bradycardia, decreased cardiac output, and hypotension. Compensatory mechanisms to maintain adequate blood pressure when the heart rate is depressed are not so developed. Thus a decrease in heart rate leads to a corresponding decrease in blood pressure and tissue oxygenation. So, it must be taken into consideration about those drugs that depress the heart rate in pediatric patients. AGE (YEAR) HEART RATE (BEATS / MINUTE) BLOOD PRESSURE MM / HG RESPIRATORY RATE (BREATHS / MINUTE) 1-3 70-110 90-105 / 55-70 20-30 3-6 65-110 95-110 / 60-75 20-25 6-12 60-95 100-120 / 60-75 14-22 12 55-85 110-135 / 65-85 12-18 Behrman, et al: Nelson textbook of Pediatrics, ed 17 These differences between children at different age levels and adults leads to the conclusion that dosage is not simply an application of a formula for derivation of a percentage of the adult dose of any agent. Drug dosages for children should be carefully individualized for each patient following established guidelines. 1. 2. 3. Patients who cannot cooperate & understand for definitive treatment. Patient lacking cooperation because of lack of psychological or emotional maturity Patients with dental care requirements, but are fearful & anxious. 1. 2. 3. 4. 5. Chronic obstructive pulmonary disease (COPD), epilepsy, & bleeding disorders. Uncooperative or unwilling patients. Unaccompanied patients.. Prolonged surgery. Lack of equipment or inadequate personnel. 1. 2. 3. 4. Obtaining patient history & information. Informed consent from the accompanying parent/ guardian. Instructions to parents preop & postop. Adequate documentation of the sedation experience with monitoring of vital signs. 1. a) b) OBTAINING PATIENT HISTORY AND INFORMATIONInformation exchanged through a formal interview helps in assessment of patient pain & anxiety. M/H specific to Sedationa) b) c) d) e) Abnormalities of major organ systems. Previous adverse experience with sedation / GA. Drug allergies & current medications. Age in years & months & weight in kgs. Time & nature of last oral intake. American Society of Anesthesiologists: Manual for Anesthesia department Organization & Management, Park Ridge, 2003 1. ASA Physical Status Classification SystemASA I- Patients with no systemic disease. These patients are able to tolerate mild physical exertion & psychologic stresses. They do not possess any organic, physiologic, biochemical, or psychiatric disturbances. 2. 3. ASA II- Patients with mild-to-moderate physiologic disturbance that is under good control. No significant compromise of normal activity, but patient’s specific condition could possibly affect safety of surgery & anesthesia. ASA III- Patients with a major systemic disturbance that is difficult to control, there is significant compromise of normal activity for this patient. This situation creates a significant impact on surgery & anesthesia. Medical consultation recommended for these patients. 4. ASA IV- Patients with severe & potentially life threatening systemic disease that significantly limits their activity are not usually seen in ambulatory health setting. Because of their unstable health problems, they are categorized as high risk for many situations & potential for acute emergency situation is great. Seek medical consultation and/or referral. 5. 6. 7. ASA V- Moribund patient in whom immediate surgery is the last effort to save their lives. ASA VI- The patient in this classification is clinically dead (i.e. declared brain-dead patient), but being maintained for organ donation. ASA E- Designation for a patient requiring an emergency procedure. Only patients who are categorized into ASA class I are routinely acceptable as candidates for conscious sedation. Children assigned to ASA classes II & III may actually benefit from this approach, but this must be determined in consultation with the child’s physician. Generally, patients categorized into classes III & IV are better managed in a hospital setting. INFORMED CONSENT- Parent/ Guardian must be agreeable to the use of conscious sedation for the child. They should receive complete information regarding-- 2. ◦ ◦ ◦ ◦ Risks & Benefits associated with the particular technique. Agents being used. Alternative methods , if available. 3. INSTRUCTIONS TO PARENTS This information should include a 24-hour contact number for the practitioner. Dietary instructions are as follows: 1. No milk or solids for 6 hours for children 6 to 36 months old and for 6-8 hours for children 36 months and older. 2. Clear liquids upto 3 hours before the procedure for children aged 6 months and older. Reasons for the instructions to parents1. Emesis during / after a sedative procedure is 2. 3. a potential complication that can result in aspiration of stomach contents leading to laryngospasm or severe airway obstruction. Aspiration may even lead to aspiration pneumonia. If the drug is taken by oral route, its uptake is maximized when the stomach is empty. 3. 4. On arriving home, the child may sleep for several hours, may be drowsy & irritable for upto 24 hours. Should be monitored while sleeping, to ensure an open airway. After treatment child should first be offered clear liquids & then solid foods as tolerated. Once solids are tolerated, there are no dietary restrictions. 4. ADEQUQTE DOCUMENTATION OF SEDATION EXPERIENCE Intraoperatively vital signs should be recorded. Type of drug, dose given, route, site, and time of administration should be noted. After completion of treatment, the patient be observed in a well-equipped recovery area. The patient should remain under direct observation until respiratory and cardiovascular stability have been ensured. GASES ANTIHISTAMINES BENZODIAZEPINES & ITS ANTAGONIST SEDATIVE HYPNOTICS NARCOTICS & ITS ANTAGONIST Gases used most commonly in Conscious Sedation techniques– Nitrous Oxide (N2O) & Oxygen(O2). 85% of Pediatric dentists use Nitrous oxide & oxygen for sedation of patients. This makes it the most frequently used sedative agent. Physical / Chemical properties of N2O: Nitrous oxide (MW 44 & Sp gravity 1.53) is a slightly sweet-smelling, colourless, inert gas. Boiling point is 88.5°C (127°F), indicates it is gas at room temperature. When compressed in cylinder it becomes liquid & vaporizes on release. It is nonflammable but, supports combustion. Physical / Chemical Properties of O2: O2 (MW 32 & Sp gravity 1.1) is a odorless, colorless & tasteless gas. It also supports combustion, but is nonflammable. DESIRABLE CHARACTERSTICS OF N2O/O2 SEDATION: 1. 2. Analgesic Properties (Pain Control)20% N2O & 80% O2 has the same effect as 15mg of Morphine. Has the ability to manage both pain & fear (fear of an injection). Amnestic properties- Postoperatively patients are unable to recall the severity of their pain or anxiety or its duration. 3. 4. 4. Anxiolytic properties (sedative effects)Assist patients in handling their fear of anxiety by producing sedation or a sense of well-being. Facilitates positive behavior. Onset of Action- Rapid less than 30 seconds, peak effects in less than 5 minutes. Recovery- Inhalation of N2O/O2 allows for complete recovery with 100% pure oxygen for 5 minutes after termination of drug. 4. 4. Elimination- It is 99% eliminated from the body within 5-10 minutes after discontinuation of use. Acceptance- Patient acceptance rate is same for oral surgical procedures as it is for general dentistry. COMBINING N2O/O2 SEDATION WITH OTHER METHODS: 1. Combination with Audio-analgesia. Since music is a method for relaxing, distracting (also known as “white sound”). 2. Oral premedication with Diazepam & Meperidine. 3. N2O/O2 & Local anesthesia because together offer superior pain & anxiety management option. PHARMACOKINETICS OF N2O: It has a blood-gas partition coefficient of 0.47 i.e. difference between partial pressures of gas (N2O) & liquid (blood) indicates how quickly agent crosses the pulmonary membrane & enters the blood stream. It is an insoluble drug & remains unchanged in blood & does not combine with any blood elements. Since N2O does not break down, so peak clinical effects may be seen within 3-5 minutes. There is no biotransformation & 99% of gas is rapidly eliminated by the lungs. Very small amounts may be found excreted in body fluids and intestinal gas. PHARMACODYNAMICS OF N2O: It produces nonspecific CNS depression. Although classed with inhalational GAs, it produces limited analgesia, & thus surgical anesthesia is unlikely unless concentrations producing anoxia are reached. So, O2 is given along with it, because its sole purpose is to avoid anoxia. To minimize the effect, the patient should be oxygenated for 3-5 minutes after a sedation procedure. At concentrations 30-50%, N2O will produce a relaxed & dissociated patient who is easily susceptible to suggestion. Amnesia, but there is little alteration of learning or memory. Moderate sedation is achieved when N2O concentration is 50% . At concentrations greater than 60%, patients may experience discoordination, ataxia, giddiness, and increased sleepiness. Concentrations greater than 50% are not to be used in dental practice. The gas is nonirritating to the respiratory tract and can be given to patients with asthma without fear of bronchospasm. ADVERSE EFFECTS AND TOXICITY Nausea and vomiting are the most common adverse effect experienced with N2O sedation. Increases with more than 50% conc or lengthy procedures. Middle ear pressure can increase pain in patients with acute otitis media. It gets entrapped in gas-filled spaces such as the middle ear, sinuses, and GIT. Neurotoxicity, impotence, and renal/liver toxicity. The greatest concern regarding toxicity centres on exposure of dental personnel to high ambient air levels of the gas during its use for patient sedation (i.e. longer than 3 hours per week Second gas effect : When N2O is being given at 70-80% concentration initially, though it has low solubility in blood, about 1l/min of N2O enters blood in first few minutes higher than minute volume. So, if another anesthetic is given at same time ,it will be delivered to the blood at same rate i.e. 1l/min which is higher than minute volume & induction effect will be faster, called as SECOND GAS EFFECT. DIFFUSION HYPOXIA- Reverse occurs when N2O is discontinued after prolonged anesthesia. Since N2O has low blood solubility it rapidly diffuses into alveoli & dilutes O2 in alveoli (due to PP of O2 in alveoli is reduced), thus O2- CO2 exchange is disrupted & a period of hypoxia is created. This can be prevented by continuing 100% O2 for 5 minutes at termination of procedure. Diffusion hypoxia is not significant with other anesthetic agents because they are given at low conc (0.2-0.4) & are not able to dilute alveolar air. EQUIPMENT: The machine should be of the continuousflow design, with flowmeters capable of accurate regulation. A fail-safe mechanism that provides automatic shutdown if O2 falls below 25% and audible and visual alarms that are activated. There should be a flush lever for easy and immediate flushing of the system with 100% oxygen. Efficient “SCAVENGER SYSTEM” is an important component of any hose-mask system. The double mask type is the most efficient type of scavenger. These systems exhaust into the vacuum waste system, which is vented to the outside. Nasal hoods should be of good design & be available in pediatric & adult sizes both. Schematic diagram to show components of a N2O/O2 delivery & scavenging system TECHNIQUE- After a thorough inspection of the equipment, the mask should be introduced to the patient with an explanation, and then the mask should be carefully placed over A-Poorly fitting mask with leakage under the nose. nares. B-Well -fitting mask. The delivery tubes are tightened behind the chair back in a comfortable position. Bag is filled with 100% oxygen and delivered to the patient for 2/3 minutes at an appropriate flow rate of 5-6 L /minute. With an appropriate flow rate, slight movement of the mixing bag should be apparent with each inhalation and exhalation. Too high flow rate, the bag will be overinflated, movement will not be seen with each breath. Too low flow rate will deplete the bag of mixed gases. Once the proper flow rate is achieved, the N2O can be introduced by slowly increasing the concentration at increments of 10% to 20% to achieve the desired level. The operator should encourage the patient to breathe through the nose with the mouth closed. SENSATIONS- Felt are floating, giddy feeling with tingling of digits. The eyes will take on a distant gaze with sagging eyelids. When this state is reached, the local anesthetic may be given. Once this is completed, the concentration can be reduced to 30% nitrous oxide and 70% oxygen or lower. The patient can now be maintained and monitored & procedure carried out. The dentist should communicate with the patient throughout the procedure, paying particular attention to the maintenance of an open, relaxed airway. An emesis basin should be readily available, and if vomiting does occur, the head should be rotated to the side. However, the laryngeal reflex is not obtunded with nitrous oxide, and so aspiration of vomitus is unlikely. Recovery can be achieved quickly by reverse titration. Once the sedation is reversed, the patient should be allowed to breathe 100% oxygen for 3-5 minutes. The patient should be allowed to sit. Even though psychomotor effects return to normal within 5 to 15 minutes, it is not advisable to allow teenage patients to drive themselves. Guidelines on Appropriate Use of Nitrous Oxide for Pediatric Dental Patients: 1. Must be given by licensed individuals only. 2. Informed consent of parents & documented in patients record before administration. 3. Preoperative & postoperative vital sign values are to be recorded. 4. Select the nasal hood according to the size of individual & make sure it fits snugly. This can decrease patient anxiety & increase trust. 5. Determine flow rate of each person, 5-6 L/min is acceptable for most patients. 6. Titration of N2O in intervals is recommended for children because they exhibit signs & symptoms of sedation so it important to remember to allow time between increments so drug can reach its peak effect before adding more, this will reduce oversedation. 7. During treatment visual monitoring of the patient’s respiratory rate & level of consciousness. 8. 9. Pulse oximeter used when high concentrations of N2O are used. Once the N2O flow is terminated, 100% O2 should be delivered for a minimum of 5 minutes. 10.Patient should return to pretreatment responsiveness before he/she is dismissed. (AAP / AAPD GUIDELINES, 2006) The acronym “SOAPME” offers a routine for preparing for sedation. SUCTION FUNCTIONING SUCTION APPARATUS OXYGEN ADEQUATE OXYGEN SUPPLY & FLOWMETERS TO ALLOW ITS DELIVERY AIRWAY APPROPRIATE AIRWAY (ENDOTRACHEAL TUBES, FACE MASK) PHARMACY ALL BASIC DRUDS NEEDED TO SUPPORT LIFE DURING AN EMERGENCY MONITORS FUNCTIONING PULSE OXIMETER EQUIPMEN T SPECIAL EQUIPMENT OR DRUGS FOR A PARTICULAR CASE (E.G. DEFIBRILLATOR) ( AAP/ AAPD GUIDELINES , 2006) Conscious Sedation that is carefully planned and carried out by a thoughtful, well-trained health care team will allow both caregivers and patients to have a positive experience rather than a bad memory… DENTISTRY FOR THE CHILD & ADOLESCENT; 9th edition; R E McDonald, D R Avery, J A Dean. ESSENTIALS OF MEDICAL PHARMACOLOGY; 5th edition; KD Tripathi PEDIATRIC DENTISTRY; INFANCY THROUGH ADOLESCENCE;5th edition; Casamassimo, fields, Mctigue, Novak TEXTBOOK OF PEDODONTICS; 2nd edition; Shobha Tandon PAEDIATRIC DENTISTRY; 3rd edition; R R Welbury,. AAP journals ,dec 1,2006,vol 118,no-6 Guideline for Monitoring and Management of Pediatric Patients During and After Sedation for Diagnostic and Therapeutic Procedures,AAPD,2006. Guideline on Use of Nitrous Oxide for Pediatric Dental Patients,2005,VOL 35,no 6 HANDBOOK OF NITROUS OXIDE & OXYGEN SEDATION; 3rd edition; M S Clark, A L Brunick Textbook of pedodontics; 2nd edition; Shobha Tandon