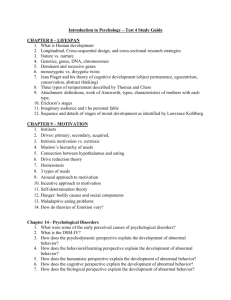
Abnormal Psych project
advertisement

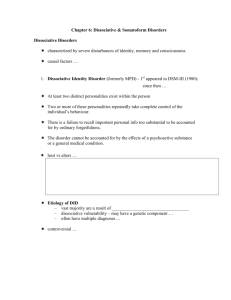
Psychological Disorders By Aaron, Kevin, Jason, and Munch Abnormal Behavior Can be distinguished with three criteria... 1. Deviant - atypical or statistically unusual a. women taking 7 showers a day 2. Maladaptive - it interferes with a person’s ability to function effectively in the world a. isolating yourself because you might be dangerous 3. Involves personal stress over a long period of time a. may cause shame, guilt, or despair Theoretical Approaches ● Biological Approach ○ attributes disorders to organic, internal causes ■ brain, genetics, neurotransmitter functions ● Psychological Approach ○ emphasizes contributions of experiences, thoughts, emotions, and personality characteristics ■ rewards/punishments ● Sociocultural Approach ○ cultural influences on developing psychological disorders ■ social, economic, technological, and religious aspects ● Biopsychosocial Approach ○ a combination of all three listed above Classifying Abnormal Behavior Psychiatrists and psychologists have devised systems classifying abnormal behaviors called the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) classification system. It uses 5 axis. Axis I - All diagnostic categories except personality disorders and mental retardation Axis II - Personality disorders and mental retardation Axis III - General medical conditions Axis IV - Physical and environmental problems Axis V - Current level of functioning Critiques of the DSM-IV The most controversial aspects are… 1. The manual classifies individuals based off of symptoms, using the traditional type of thinking that mental disorders are a type of disease. This implies abnormalities have an internal cause that is independent of the environment 2. It focuses strictly on pathology and problems, instead of emphasizing strengths as well https://www.youtube.com/watch?v=5leB-pmpxek Dissociative Disorders • • • • Dissociative Disorders- Sudden loss of memory or change in identity due to dissociation of conscious and memory Dissociative Amnesia- amnesia caused by intense psychological stress Dissociative Fugue- Amnesia + unexpected travel away from home (sometimes assume a new identity) Dissociative Identity Disorder (DID)- Formerly known as Multiple personality disorder. Individuals develop two or more distinct personalities Symptoms of Dissociative Disorders Symptoms Depression Mood swings Suicidal tendencies Sleep disorders (insomnia, night terrors, and sleepwalking) Anxiety, panic attacks, and phobias (flashbacks, reactions to stimuli or "triggers") Alcohol and drug abuse Compulsions and rituals Psychotic-like symptoms (including auditory and visual hallucinations) Eating disorders • • • • • • • • • Treatment of Dissociative Disorders • • • Treatment- talk therapy or psychotherapy, medications, hypnotherapy, and art or movement therapy. Often anxiety or depression is also present Dissociative disorders may be treated using the same drugs prescribed for those disorders. Antidepressants or anti-anxiety medication Case Studies- Dissociative Amnesia http://emedicine.medscape.com/article/294508-overview Dissociative Amnesia29-year-old female experienced the onset of dissociative amnesia She was found in a hotel bathroom unconscious, with no signs of structural or neurologic abnormalities or alcohol or chemical consumption Could not remember her name, address, family, or any facts about her home life The amnesia persisted for nearly 10 months, until the feeling of blood on the woman's fingers triggered a recollection of events She had witnessed a murder that night in China She recalled being unable to help the victim out of fear for her own safety Most memories returned however some are still lost • • • • • • • Case Study- Dissociative Fugue • • • • • • • • • 28-year old male final year medical student. Declared missing for 10 days He was later seen in a city in South-Western Nigeria, a distance of about 634km from SouthEastern Nigeria where he lived and schooled Ten days before presentation, the patient suddenly saw a full human skeleton reading at the same table with him, sitting at the opposite side. The patient claimed he felt unease and quite uncomfortable. After this he had overwhelming fears and did not know when he left the room. Two days later, he discovered he was with his younger sibling in South-Western Nigeria. The patient had no knowledge of how he made the journey that takes approximately 8 hours by road. He could not remember any of the journey including how he payed for it and where he slept. The patient denied all memory of events for the 2 days from when he left his room at the university to the time he suddenly realized he was at his brother’s house, 634km away The brother, however, reported that the patient appeared unkempt, looked exhausted but was fully conscious and alert on arrival at his house without any assistance. Case study- DID • • • • • • Woman who had experienced physical and sexual abuse from her father Exhibited at least 4 personalities as an adult. Each personality was of a different age– a fearful child, a rebellious teenager, a protective adult, and the woman's primary personality. Only one of the personalities, the protective adult, was consciously aware of the others. When one of the secondary personalities took over, it often led to episodic dissociative amnesia During intensive therapy sessions, each personality was called upon as necessary to facilitate their integration. Schizophrenia • • Severe psychological disorder characterized by highly disordered thought processes, referred to as psychotic because they are so far removed from reality. Individuals with Schizophrenia often see things that are not there, hear voices inside their heads, and live in a strange world of twisted logic (often withdrawn or isolated) ● Positive Symptoms ○ They are “positive” because they reflect something added above and beyond normal behavior. The positive symptoms Include ■ Hallucinations: Sensory experiences in the absence of real stimuli (seeing things that are not there) ■ Delusions: False, unusual, and sometimes magical beliefs that are not part of an individual’s culture. ■ Thought disorder: Unusual, sometimes bizarre thought processes (thoughts often disorganized or confused) ■ ● Disorders of movement: May show unusual mannerisms, body movements, and facial expressions. In some cases this may cause them to become Catatonic (a state of immobility and unresponsiveness that lasts for long Negativeperiods Symptoms of time) ○ Reflect social withdrawal, behavioral deficits, and the loss or decrease of normal functions. One negative symptom is the Flat affect (the display of little or no emotion) ● Cognitive Symptoms ○ Include difficulty sustaining attention, problems holding information in memory, and inability to interpret information and make decisions. Causes of Schizophrenia Biological FactorsHeredity: Research shows that Schizophrenia is at least partially caused by genetic factors (as genetic similarity to a person with Schizophrenia increases, so does a persons risk of developing Schizophrenia) Structural brain abnormalities: Imaging techniques such as MRI scans have shown enlarged ventricles in the brains of those with Schizophrenia (fluid-filled spaces, and the enlargement of the ventricles indicates deterioration in other brain tissue) Small prefrontal cortex, and lower activity in this area of the brain than those who do not have Schizophrenia. changes in the brain most likely occur prenatally because they are not accompanied by glial cells (which are always present when a brain injury occurs after birth) • • • • Association of Genes with Schizophrenia Psychological Factors • Theorists believe that stress may contribute to the development of this disorder • The diathesis-stress model: View of Schizophrenia emphasizing that a combination of biogenetic disposition and stress causes the disorder Sociocultural Factors • Sociocultural background is not considered a cause of Schizophrenia, but • do appear to affect the course of the disorder (influence how Schizophrenia progresses) Across cultures, individuals with Schizophrenia in developing, nonindustrialized nations tend to have better outcomes than those in developed industrialized nations (this may be due to the fact that those in developing nations are more accepting and supportive of individuals with Schizophrenia) Case Study- Schizophrenia ■ young boy wouldn't eat his favorite fast food anymore because he ■ ■ ■ ■ ■ ■ ■ thought his parents put things in his food to make it taste “funny” he zoned out often and laughed out of nowhere starting spending more time alone and his room and became very aggressive when coming in contact with family said that his mom was from a different planet and was sent here to kill him and that his siblings were put on earth to protect him from her used a foreign language often when speaking to his family and told them many times they were going to die paced constantly or would do the complete opposite and not get out of bed for long periods of time started to eventually hallucinate and see things like bugs on his walls was eventually admitted to the hospital by parents Personality Disorders • Chronic, maladaptive, cognitive-behavioral patterns that are thoroughly integrated into an individual’s personality. https://www.youtube.com/watch?v=BViqlxVjRn4 Antisocial Personality Disorder (ASPD) ● A psychological disorder characterized by guiltiness, law-breaking, exploitation of others, irresponsibility, and deceit ○ Biological factors- genetic, brain, and autonomic nervous system differences (like low levels of activation in the prefrontal cortex and an underaroused autonomic nervous system) The criteria for antisocial personality disorder include ■ failure to conform to social norms or obey the law ■ deceitfulness, lying, conning others for personal profit or pleasure ■ impulsivity or failure to plan ahead ■ reckless disregard for safety of self or others ■ irritability and aggressiveness ■ consistent irresponsibility ■ lack of remorse Borderline Personality Disorder (BPD) ● A psychological disorder characterized by a pervasive pattern of instability in interpersonal relationships, self-image, and emotions, and of marked impulsivity beginning by early adulthood and present in a variety of contexts. ○ ○ women make up 75% of those with the disorder many individuals with BPD report experiences of childhood sexual abuse as well as physical abuse and neglect Borderline Personality Disorder is indicated by the presence of 5 or more of the following symptoms ■ ■ ■ ■ ■ ■ ■ ■ frantic efforts to avoid being abandoned markedly and persistently unstable self-image or sense of self impulsivity in at least 2 areas that are potentially self-damaging (ex: spending, sex, substance abuse) recurrent suicidal behavior, gestures, or self-mutilating behavior unstable and extreme emotional responses chronic feelings of emptiness inappropriate, intense anger or difficulty controlling anger temporary stress-related paranoia or severe dissociative symptoms Case Study- ASPD Man hospitalized with symptoms of ASPD ■ had been in several fights by the age of 11 ■ admits that he carried weapons and harmed others and that he lacked remorse ■ said that he stole from his dad and stole comic books from school and then sold them ■ stated that he is full of anger and said the more he hits someone, the more anger builds up inside of him Case Study- BPD ■ Woman tried to overdose multiple times and hoped maybe someone would notice she was in need of help ■ had no hopes for tomorrow ■ tried to run away numerous times ■ felt panic, fear, and anger often ■ wanted to be respected, liked, and approved of but didn't know how to “attain” these privileges and often thought she wasnt worthy of it ■ often overwhelmed by present pain that reminded her of the past ■ in several stressors occured in a sequence she would often start to generalize, negatively. Therapy and Antianxiety Drugs • • Biological Therapies = treatments that reduce symptoms of psych. disorders by altering body function Antianxiety drugs = tranquilizer, reduce anxiety, addictive o Benzodiazepines (fast): Xanax, Valium, Librium Drowsiness, loss of coordination, fatigue, hazards, birth defects, depression o Nonbenzodiazepine (slow): BuSpar o Used for stress and/or anxiety o Symptomatic relief Therapy and Antidepressant Drugs • Antidepressant drugs = regulate mood o Tricyclics (Elavil) - 3 rings, slow, increase norepinephrine and serotonin o Tetracyclics (Avanza) - aka NaSSAs, increase same hormones as tricyclics, “most effective” o Monoamine Oxidase (MAO) inhibitors (Nardil) block MAO, allow norep. and sero. to stay, not common, risky w/ food o Selective serotonin reuptake inhibitors (Prozac, Paxil, Zoloft) - prevent reabsorption of sero., fewer side effects, more common Antidepressants (cont.) • • • 10% take an antidepressant at some pt (2x previous decade) Used for both mood disorders and anxiety disorders (panic, OCD, social phobia, PTSD, eating/sleep, etc), sleeplessness, chronic pain Lithium = lightest of solid elements, used for bipolar disorder (may stabilize norep. and sero. levels) o weight gain effects, nearly toxic Do Antidepressants Increase Suicide Risk in Children? • • Impulsive suicide • 4% of antidepressant users reported suicidal thoughts, vs. 2% of placebo group • FDA “black box” warning, prescriptions dropped • 17% think of suicide, many not on antidepressants, excluded from studies Antipsychotic Drugs • Antipsychotic drugs = powerful, reduce • • • • agitation, tension, hallucination, help behavior, sleep, esp. schizophrenia Neuroleptics = most common, treat schizo., twitching (tardive dyskinesia) Atypical antipsych. meds - lower risk Small doses, combine w/ psychotherapy, social training see Figure 16.2 page 526 Electroconvulsive Therapy (ECT) • ECT = shock therapy, treatment for depression, causes brain seizure • Later resort, in sleep, may relapse • Memory loss, impairment • Deep brain stimulation = implanted electrodes emit signals to alter brain chem, severe depression, OCD Psychosurgery = irreversible surgery of brain tissue Antonio Egas Moniz cut frontal fibers Walter Freeman did prefrontal lobotomies Damaging? Ethical? Now a last resort, minimal invasion • • • • Duties of Group members Kevin- Abnormal Behavior Aaron- Dissociative Disorders Taylor- Schizophrenia and Personality Disorders Jason- Therapy Works Cited http://emedicine.medscape.com/article/294508-overview http://www.jmedicalcasereports.com/content/7/1/143 http://www.webmd.com/mental-health/dissociative-identity-disorder-multiple-personality-disorder https://www.youtube.com/watch?v=5leB-pmpxek https://sites.google.com/site/consultingservicesinfo/mental-illness/anti-social-personality-disorder http://ps.psychiatryonline.org/article.aspx?articleid=81024 http://www.schizophrenia.com/family/perstory5.htm