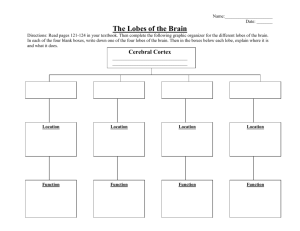
Left parietal lobe
advertisement

Venous system Cerebral venous system • Superficial system: – Drains into the venous synuses • Central system – Drain in a large, short venous trunk – the great vein of Galien • Basal system – Drains the blood into the basilar vein and then to the great vein of Galien • Jugular veins Cerebral venous trombosys • Causes: • Infectious – significantly decreased since antibiotics – Local – General • Non infectious – Local: trauma, surgical interventions, tumors, arterialtrombosys, malformations – General: surgicale, pregnancy, post partum/post abortum, drugs, dehydration, advanced liver or kidney disease • Idiopatic Cerebral venous trombosys • Venous synus thrombosis: – Increased pressure in the preceding veins (depending on the anastomosys system) – increased intracranial pressre • Superior longitudinal synus: role in resorbtion of the CSF • Cerebral veins thrombosys – Secondary hemorrhage is more frequent – Cerebral edema, venous infarcts – Seizures Cerebral venous trombosys • Clinical picture: – Increased intracranian pressure (headache, nausea, papillary edema, consciousness abnormalities) – Focal or generalized seizures – Meningean syndrome – Focal signs – Septic CVT: fever, other signs of severe infection Cerebral venous trombosys • Cavernous synus thrombosys – Staphilococcus infections of the face, orbitary, synuses, teeth other ENT infections – Trauma – Usually the clinical picture is marked by the septic syndrome – Venous stasis: • Palpebral edema, chemosis, exoftalmia • VI-th and then IIIrd, IV-th, and ophtalmic ramus of the Vth nerves palsies – Often clinical signs are bilateral – the 2 synuses are conected Cerebral venous trombosys • Investigations – CT, MRI • Thrombus image • Empty vessel (CT with contrast substance) • Infarctus or hemorrhages images – Arteriography – CSF analysis – differential diagnosys of an infection – EEG, funduscopy • Treatment: • Etyologic treatment • Antithrombotic treatment (anticoagulants) • Treatment of cerebral edema, raised intracranian pressure, seizures Brainstem alternate syndroms Medullary alternate syndromes • A combination of the following, in various degrees, depending on the exact position and size of the lesion: • On the same side with the lesion – Nucleus ambigus, vagus nerve nucleus, hipoglossal nerve nucleus, accesory nerve nucleus • Palatal weakness, bitonal voice, • Tongue atrophies • sternocleidomastoidian and trapesus muscle palsy, • On the opposide side – Loss of temperature and pain sensation – Hemiparesis Lateral medullary syndrome (Wallenberg syndrome) • This is the commonest of the brain stem strokes • Vertebral artery or posteroinferior cerebellar artery • Sudden onset – Intense vertigo, vomit, balance problems, hiccup • Most of the times: favourable evolution Lateral medullary syndrome (Wallenberg syndrome) • On the same side with the lesion: – Involvement of the descending nucleus and tract of Vth nerve results in loss of pain and temperature sensation on the face – Vestibular syndrome – Swallowing problems, palatal weakness and dysphagia - bitonal voice (involvement of the nucleus ambiguus, IXth, Xth, XIth nerver palsy) – Horner’ syndrome (involvement of descending autonomic fibers ) – Involvement of the inferior cerebellar peduncle (restiform body) causes ipsilateral ataxia • On the opposite side: – Loss of pain and temperature sensation – Sometimes discrete hemiparesis Infarction of the base of the pons • In bylateral lesions: corticospinal and corticobulbar tracts in the basis pontis are interrupted • Locked in syndrome – Tetraplegia, billateral facial palsy, billateral palsy of the abducens nerve – Vertical gaze is maintained – Consciousness/higher functions are maintained, but the patient is unable to speak or move • Lesion spares the reticular formation above the caudal pons, and therefore the patients remain awake • The only way to communicate with these unfortunate patients is to ask them to move their eyes in response to questions. Millard-Gubler syndrome (pontine inferior) • On the same side with the lesion – Peripheral facial palsy – External oculomotor (VIth nerve) palsy • On the opposite side – hemiplegia Pontine lesions • Lesions of the sixth nerve nucleus – paralysis of gaze to the side of the lesion. – Internuclear palsy (fibers from the opposite 6th nerve nucleus are involved as they cross to the MLF, there is also weakness of the ipsilateral medial rectus muscle). • The ipsilateral seventh nerve can be involved since its fibers course around the sixth nerve nucleus. • Involvement of the medial lemniscus – contralateral loss of position and vibration sense • descending corticospinal fibers in the base of the pons – contralateral hemiparesis Midbrain syndromes: Weber syndrome • Are involved – the descending corticospinal and corticobulbar fibers in the cerebral peduncle, and – the fibers of the third nerve that traverse the peduncle on exiting the midbrain. • On the opposite side: hemiparesis • On the lesion’s side: third nerve palsy (ptosis, inability to move the eye up, down or medially, and [if fibers from the EdingerWestphal nucleus are involved] pupillary dilitation). Red nucleus syndromes • Third nerve palsy on the same side, cerebellar syndrome on the opposite side, chorea, thalamic sensory syndromes • Chorea • Benedikt's syndrome – homolateral third nerve palsy – contralateral ataxia, – midbrain stroke involving the third nerve as it travels near the red nucleus. A lesion of the red nucleus interrupts fibers from the opposite cerebellar hemisphere (dentate nucleus of the cerebellum superior cerebellar peduncle crossing in midbrain red nucleus VA/VL thalamus). Cerebral lobe syndromes Frontal lobe Frontal lobe • Highest level of brain evolution • Involved in many functions • Lesions in different parts lead to different syndromes Frontal lobe Frontal lobe syndrome • Lesions of the motor area lead to motor deficits of the opposite half of the body – Irritative lesions – jacksonian motor seizures • Lesions of premotor areas – less important motor deficit – Irritative lesions in premotor areas – “adversive” seizures, or supplementary motor area seizures – Supplementary motor area seizures: cessation of all activity, tonical contractions of proximal muscles, repetitions, pallilalia – Premotory areas lesions: diminishment of spontaneous movements, delay of voluntary actions (movements), eventually hyopkinesia, akinesia, tremor – Forced prehension – Gait and posture abnormalities; frontal ataxia Frontal lobe syndrome • Prefrontal areas lesions – Alteration of personality – Diminishment of spontaneous activity - the patient does not feel the need to do anything, is not able to plan the future events, may be agitated – Attention deficits – memory is normal, but the patient doesn’t bother to use it – Loss of abstract thinking – Perseveration – Afffective changes – either apathic, “flat”, either excessively exuberant and childish; may show lack of inhibition, eventually sexually improper actions Frontal lobe syndrome – Prefrontal dorsolateral cortex lesions • Diminished fluency (verbal & nonverbal), reasoning problems, reduction of spontaneous responses inhibition, perseveration, attention deficits – Orbitofrontal cortex lesions – desinhibition, anosmia – Mezial frontal cortex, anterior cingullary cortex lesions – apathy, abulia, memory impairments Cognitive function testing in frontal lobe lesions – MMS does not approach these problems – Frontal lobe tests: • “go-no go” tests – patient is told to lift 2 fingers, but the evaluator lifts only 1 • Speech fluency – patient is asked to produce as many words he can starting with letter “Z” – normally more than 8 words/ 1 min • Motor tests for perseveration – patient is asked to execute series of 3 movements (fist, edge-palm tests – Luria) Parietal lobe Parietal lobe • Anterior somatosensory area, posterior association area • 4th neuron of sensory tracts (3, 1, 2 areas – primary somatosensory cortex • 5, 7, 39, 40 areas – somatosensory association areas; areas 5 and 7 are important for stereognosis • Parietal regions appear when the singers are used for more than just mobility (catching, throwing) Parietal lobe syndromes • Controlateral hemihypestesia (diminished sensation) • Astereognosis (5 & 7 areas lesions) • Sensory epilepsy (paresiae and sometimes paroxistical pain) • Asomatognosia (left hemisphere lesions lead to one side asomatognosia, anosognosia, anosodiaforia, neglect of left body half) • Right parietal lobe – spatial component of activities – Apraxia – loss of the ability to execute or carry out learned purposeful movements, despite having the desire and the physical ability to perform the movements – Finger agnosia – Left-right agnosia Parietal lobe syndromes • Left parietal lobe – symbol and experiences comprehension – ideomotor (inability to carry out a motor command or a learned gesture, for example, "act as if you are brushing your teeth" or "salute") • limb apraxia when movements of the arms and legs are involved, • nonverbal-oral or buccofacial (inability to carry out facial movements on command, e.g., lick lips, whistle, cough, or wink), – ideational (inability to create a plan for or idea of a specific movement, for example, "pick up this pen and write down your name") – Inability to use the informations on spatial relations • Constructive apraxia • Topographic agnosia • Prosopagnosia Parietal lobe syndromes • Speech problems – frequently associated with writing problems • Motor abnormalities (diminishment of spontaneous movements, unstable hand, syncynesia) • Balance problems • Taste problems (area 43) • hemianopia Parietal lobe syndromes • Gerstmann syndrome (left angulary girus) • Digital agnosia • Left-right confusion • Agraphia • Acalculia Parietal lobe syndromes • Balint syndrome (bilateral posterior parietal lesions) – Patient looks only at 35-40 degrees to the right, and describes only the objects in that area – Can look at only one object a time – Neglect of left hemispace – Tactile functions impairment – Visual or tactile agnosia – Apraxia – Speech problems (alexia, aphasia) – Dyscalculia – Immediate memory impairment – Body scheme abnormalities – Left-right confusion – Problems with space orientation – Eye movements problems Parietal lobe Constructive apraxia • Adaptative possibilities of parietal lobes – blind boy “reads” with the tip of his nose Temporal lobe Temporal lobe • Below the sylvian sulcus, extends up to the limits of the parietal and occipital lobes • Primary and secondary auditory areas (41, 42), association areas (38, 20, 21, 22); – Taste (area 38) – Areas 41 and 42: perception and comprehension of sounds, comprehension of words • Lymbic system (hyppocampic uncus, hypocampus, girus cinguli, subcallosal areas, olfactory areas)- emotions and affect • Optic radiations • Left temporal lobe – comprehension and recognition of words, language • Right temporal lobe – intonation, music Sindroame de lob temporal • Lezarea lobului temporal – – tulburari de auz, echilibru, gust, miros, limbaj, vedere, memorie, comportament alimentar, comportament sexual. Convulsiile cu originea in aceste arii se manifesta ca si asocieri de tulburari ale ratiunii, halucinatii, comportament anormal, detasat sau violent, necontrolabil • Afectarea auzului – lezarea ariei 41; leziune unilaterala – hipoacuzie; leziuni bilaterale – surditate corticala. Leziunile iritative (epilepsie temporala) apar iluzii auditive, halucinatii auditive • Tulburarile de echilibru – atacuri de vertij, uneori cu ataxie • Tulburarile de gust si miros – halucinatii olfactive pot apare ca parte a crizelor epileptice. Distrugerea ariei olfactive din uncusul hipocampic si extinderea leziunilor spre girusul hipocampic duc la anosmie. Halucinatiile olfactive pot uneori precede convulsiile (aura) • Afectarea vizuala – hemianopsie, afectarea memoriei vizuale • Tulburari de vorbire de tip afazic receptiv (afazie Wernicke) – leziuni ale ariei posteroinferioare a girusului temporal superior stang Sindroame de lob temporal • Tulburari de memorie – – – – – – Tulburarile memoriei recente – leziuni hipocampice inferioare bilaterale. Lezarea bilaterala a corpilor mamilari duce la afectarea memoriei pe termen scurt Afectarea memoriei pentru cuvinte Afectarea memoriei pentru cuvinte in leziunile hipocampice inferioare bilaterale Afectarea memoriei de lunga durata – leziuni mamilotalamice sau leziuni corticale bilaterale Inmagazinarea de elemente noi si intelegerea acestora se realizeaza prin intermediul circuitului lui Papez (hipocamp, corpi mamilari, talamus, girus cinguli) • Tulburari ale comportamentului alimentar si sexual – nu numai in leziuni ale lobului temporal, ci si in leziuni hipotalamice • Epilepsia de lob temporal – – – Diagnostic electroencefalografic Halucinatii psihosenzoriale simple sau complexe, episoade de afazie, halucinatii olfactive sau auditive Tulburarile de recunoastere si amintire – déjà vu, deja pense, jamais vu Papez circuit • • • • James Papez in 1937 One of the major pathways of the limbic system Chiefly involved in the cortical control of emotion. Role in storing memory. Sindromul Kluver Bucy • Heinrich Kluver si Paul Bucy, 1939 • Lobectomie temporala bilaterala – prima dovada experimentala a implicarii circuitului luii Papez in expresia emotionala • Lipsa de afect, agnozie vizuala, expresie sexuala nediscriminata, pierdere severa a memoriei Occipital lobe Lobul occipital • O mica parte a portiunii dorsolaterale a emisferelor • Functiile sunt legate de vedere – – – – Perceptie vizuala Recunoastere in relatie cu spatiul si timpul Ariile 17, 18 si 19 Brodmann Aria 17 (striata) este localizata la nivelul scizurii calcarine si in vecinatatea acesteia; este centrul de receptie al informatiei vizuale (culoare, dimensiuni, forma, miscare, iluminare, transparenta) – Aria 18 (parastriat) si aria 19 (peristriat) ocupa restul suprafetei interemisferice la nivel occipital, avand rol de cortex de asociatie • Tulburarile care rezulta din lezarea lobului occipital pot fi de natura iritativa sau datorate unui deficit, cu simptomatologie uni sau bilaterala Sindroame de lob occipital • • Leziuni iritative: Halucinatii vizuale – simple (elementare) sau complexe, avand aspecte senzitive si cognitive – Halucinatiile elementare includ stele, flashuri luminoase, culori, lumini forme geometrice (cercuri, patrate, hexagoane), care pot fi mobile sau stationare (zigzag, oscilatii, vibratii, pulsatii) – Halucinatiile complexe include obiecte, persoane, animale de dimensiuni normale, foarte mici sau foarte mari. Pacientul poate constientiza natura ireala a acestora sau poate fi convins ca sunt reale. • Iluzii vizuale (metamorfopsia) – distorsionarea obiectelor (forma, dimensiuni, culoare, miscare) – Imaginile pot sau nu sa evoce amintiri vizuale. Efectul cumulat este asemanator cu starea de vis care apare in epilepsia temporala. – Micropsie, macropsie sau megalopsie, obiecte in miscare spre subiect, alungite, umflate, modificari ale dimensiunilor orizontale sau verticale – Coloratii iluzorii (erithropsia), lipsa culorilor (acromatopsia), vedere inversa, iradierea contururilor, poliopie (un obiect apare multiplicat), diplopie monoculara, iluzii de miscare a obiectelor stationare – Pierderea vederii spatiale, reaparitia periodica a unor imagini dupa ce ele au incetat sa se mai afle in campul vizual (palinopie sau palinopsie), o falsa orientare a obiectelor in spatiu (allestezie optica) • Epilepsia de lob occipital – halucinatii vizuale elementare, care se misca sau nu in campul vizual Sindroame de lob occipital • Sindroame de deficit • Agnozia pentru culori – pierderea perceptiei corecte pentru o culoare, imposibilitatea denumirii culorilor, a identificarii lor • Leziunile distructive unilaterale duc la hemianopsie controlaterala omonima (pierderea partiala sau completa a vederii care se proiecteaza in aria corticala occipitala primara • Cecitatea corticala apare atunci cand ambele arii vizuale primare din lobul occipital sunt lezate. – Pacientul nu este capabil sa proceseze informatia vizuala si se comporta ca si in cazul unei cecitati periferice. – Unii pacienti incearca totusi sa se comporte ca si cum ar vedea (nu isi recunosc cecitatea). Acest tip de cecitate corticala se numeste sindromul Anton, si are asociate leziuni parietale si neglijare senzitiva, in unele cazuri si pentru alte modalitati ale sensibilitatii. Sindroame de lob occipital • • • • Leziunile ariilor 18 si 19 din emisferul dominant duc la agnozie vizuala pentru obiecte (acestea pot fi recunoscute prin intermediul altor simturi); de obicei este insotita de agnozie verbala si hemianopie omonima. Dislexia – tulburari de recunoastere a cuvantului scris. Cecitatea pentru cuvinte este o tulburare rara (cortexul vizual primar este intact, leziunea se afla in cortexul occipital de asociere pe partea stanga) Prosopagnozia – leziunile sunt localizate in regiunile de asociere ventromediala si occipitotemporala; frecvent insotita de agnozie pentru culori Sindromul Balint – Lezarea bilaterala a lobilor occipitali, cel mai frecvent in ariile de granita (19 si 17) ale regiunii parieto occipitale – Imposibilitatea dirijarii corecte a oculomotricitatii in timpul explorarii spatiului; imposibilitatea privirii voluntare si a scanarii spatiului periferic, imposibilitatea de a apuca si de a atinge un obiect cu ghidare vizuala. – Inatentia vizuala care afecteaza in primul rand periferia campului vizual