National Regulatory Issues Battle Plan
advertisement

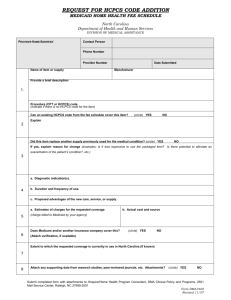
Introduction Competitive Bidding/MPP • Work for the passage of legislation that would create a MPP Demonstration Project (Rep. Tom Price) • Work with key members of Congress on legislative proposal to address reimbursement cuts in non-CB areas starting on January 1, 2016. Audit Reform / Legislation • Work for the reintroduction of the AIR Act (Reps. Ellmers and Duckworth) • Participated in review of Senate Finance Committee Audit Legislation Chairman’s Mark Language • Participated in GAO Study on Prepay/Postpay Audits and the appeals process Prior Authorization • Work with House and Senate on legislative language to make the PMD Demo permanent and nationwide. 21st Century Cures Act contains demonstration extension and expansion Goal: include all power mobility devices and accessories and options; and begin expanding the PMD prior authorization nationally. This legislation exempts suppliers for audits if they receive prior approval. • H.R. 2437 Introduced by Blackburn – Exempts from audits – Requires prompt review process CRT/Separate Benefit Legislation • H.R. 1516 introduced on March 19, 2015, Reps Sensenbrenner (R-WI) and Crowley (D-NY) Bricks and Mortar State Legislative Effort • Work with the Executive Committee and state associations to assist state associations that are seeking bricks and mortar licensure requirement. CB/Binding Bid Update – Requires the bidders to obtain a bid bond, which is set up similarly to a surety bond. – Requires CMS and their contractors to verify all licensure PRIOR to accepting a bid. – Requires suppliers to accept contracts if the price is at or above their bid – If supplier does not accept contract, bond $$ is paid to CMS – Bond company will pursue supplier for bond payment • Called the HME Audit Key, this new audit tracking system will quantify the impacts of audits and present compelling data that policymakers cannot ignore. • This is a massive, long term commitment that will benefit the entire industry and AAHomecare is committed to making sure it is given the resources it needs to succeed. STATE OF THE AUDIT KEY • First phase of testing complete – focus on functionality • Second phase of testing in process now – 25 companies participating with real data • Challenges with phase II, access to data and completion – Going back to 2014 – Suppliers actually tracking data in this format – Challenges within current software applications • Potential to develop audit and appeal application • Develop quarterly reports FACTS OF THE AUDIT KEY • Web based application with validation, anonymity and security • Compiles audit activity and data going back to January 2014 • Requires suppliers be able to track audit activity cumulatively • Includes operational questions to be able to report based on size of an organization DATA ELEMENTS OF THE AUDIT KEY • # of unique patients • # of unique Medicare fee for service patients • Net revenue (aggregate audit impact on small businesses) • # of claims submitted to Medicare fee for service • # of patients setup by product category (establish universe) • # of audits received from MAC and RAC contractors pre and post pay • # of appeals to redetermination, reconsideration and ALJ • Status of appeal activity at redetermination, reconsideration and ALJ How to Register Data Collection Phase II Testers – Thank you! A Plus Medical Advanced Homecare Apria Healthcare BLACKBURN’S Fairmeadows Home Health Center, Inc. Fairmont Home Medical Har-Kel, INC. HomeMed, LLC. Hoveround Corporation Inogen, Inc. Laurel Medical Solutions Liberty Medical Specialties Medical Service Company Reliable Medical Supply Roberts Home Medical Seeley Medical Shield Healthcare Centers, Inc. AAHomecare Regulatory Goals 2015 • Focus on issues associated with Medicare’s (ACA) WOPD requirements identifying issues, prioritizing and actively pursuing changes that would benefit AAH members and the beneficiaries they serve. – Signature date on electronic orders – WOPD Definition – 5 elements – Date Stamp – Face to Face Requirement Only on Initial Order – Face to Face HCPCs Recommendation • Improve/influence CERT oversight, understanding framework of CERT contractor and authority. Develop relationship with CMS oversight contacts. – Control what we can Control – Written Order Prior to Delivery – Detailed Written Order – Proof of Delivery AAHomecare Regulatory Goals 2015 • Focus on issues with Medicare’s documentation requirements related to accessories and supplies identifying issues, prioritizing and actively pursuing changes. Repair documentation Change of supplier documentation for supplies • Evaluate, review and respond to all issues advanced notices of proposed rules, proposed rules within the timeframe specified. Expansion CB pricing non-CB areas/bundling EHR IT Certification Anticipate additional proposed rule on CB pricing expansion AAHomecare Regulatory Goals 2015 • Participate in HCPCS coding initiatives with HCPCS Coding Alliance, working with the PDAC and Dr. Hughes, researching coding history, etc. HCPC annual coding meeting May 2015 Met with Dr. Hughes • Identify key CMS contacts on Medicaid oversight issues and work to meet with them on identified Medicaid issues. • Medically Unlikely Edit (MUE) requests from CMS to be evaluated and responded to in a timely manner by the Medical Supplies Council. AAHomecare Regulatory Focus 2015 • Sale replacement PMD components on group 2 chairs capped • Timely filing limit exemption where initial claim in audit status • RAC oversight with new dedicated contractor • Proof of delivery requirements when payer change • Clarification on filing oxygen claim for denial when patient does not qualify • Repair documentation requirements AAHomecare Regulatory Focus 2015 • CMN/DIF requirements removed • OMHA appeals backlog recommendations and follow-up • OIG competitive bidding report on access to care for beneficiaries • GAO study on pre-pay/post-pay audits and appeals backlog • EHR limitations and Medicare DMEPOS requirements • ICD10 implementation AUDIT REFORM CONTINUED EFFORTS • Remove ability for MACs to issue ‘clarifications’ • Enhance review of DME suppliers who do not respond to audit requests • Limit the number of audits a DME supplier can receive • Reinstate “clinical inference” and “clinical judgment” • Require that electronic health records include DMEPOS medical necessity documentation • Mandate use of a template in power mobility device (PMD) prior authorization demonstration. Final Rule on CB Pricing Expansion • Established 8 BEA regions in the country • Allowables based on the un-weighted average of SPAs from CBAs that are In each region • National ceiling and floor limits would be based on 110 percent and 90 percent, of the average of the RSPAs weighted by the number of contiguous states per region • Any RSPA above the national ceiling would be brought down to the ceiling and any RSPA below the national floor would be brought up to the floor • Rural area” means a geographic area represented by a zip code of at least 50 % of the total geographic of the area estimated to be outside a metropolitan area (MSA) and not included in a CBA AND includes a geographic area represented by a postal zip code that is a low population density area excluded from CBA Final Rule on CB Pricing Expansion • Phase in reduction of allowables: 1/1/16 50% of the difference between current allowable and RSPA 7/1/16 100% reduction to the new RSPA • Example an area where the adjusted fee is the RSPA rate - $100 and the current state fee schedule amount is $200, the rate will be $150 for 1/1/16 – 6/30/16 and then $100 for 7/1/16 forward • Adjustments to the fee schedule amounts for areas outside the contiguous United States would be based on the higher of the average of SPAs for CBAs in areas outside the contiguous United States (Honolulu) or the national ceiling limit • Payment adjustments for HCPCS included in no more than ten competitive bidding programs an items no longer included in CB to 110 percent of the unweighted average of the SPAs to be implemented throughout the entire country Final Rule on CB Pricing Expansion • Established only 1 RSPA for items (hcpcs) included in more than 1 product category – wheelchair accessories • Payment amounts will be the weighted average of the single payment amounts for the code computed for each CBA based claims payment data • Defines unbalanced bidding when there are more than one item in a category with additional features or functions (enteral pump with alarm and without alarm) • Limit the allowable to the lower level SPA for enteral pumps and group 1 and 2 power wheelchairs • CRT accessories to be paid at SPA, no longer exempt Pricing Examples RURAL AREAS RURAL % RURAL % HCPCS CODE CURRENT RURAL 1/1/16 REDUCTION 1/1/16 RURAL 7/1/16 REDUCTION 7/1/16 A6550 $25.86 $25.86 0% $25.86 0% A7000 $10.25 $9.40 8% $8.54 17% A7030 $177.80 $145.31 18% $112.82 37% A7034 $110.87 $90.28 19% $69.68 37% B4034 $6.17 $4.86 21% $3.55 42% B4035 $11.77 $9.16 22% $6.55 44% B4036 $8.08 $6.50 20% $4.92 39% B4150 $0.69 $0.57 18% $0.44 36% B4154 $1.23 $1.02 17% $0.80 35% B9002 $119.90 $95.75 20% $71.60 40% E0143 $20.35 $13.13 36% $5.90 71% E0255 $110.73 $96.45 13% $82.16 26% E0260 $132.39 $105.36 20% $78.33 41% E0277 $663.03 $465.25 30% $267.47 60% E0431 $29.97 $25.73 14% $21.49 28% E0470 $241.85 $185.72 23% $129.59 46% E0601 $105.29 $78.59 25% $51.89 51% E1390 $178.24 $140.81 21% $103.38 42% E1392 $51.63 $49.27 5% $46.90 9% E2365 $105.72 $92.66 12% $79.60 25% E2402 $1,617.82 $1,256.89 22% $895.96 45% K0001 $58.25 $43.73 25% $29.20 50% K0003 $97.98 $71.51 27% $45.03 54% K0738 $51.63 $49.27 5% $46.90 9% K0822 $565.17 $462.17 18% $359.16 36% K0823 $568.89 $442.01 22% $315.13 45% K0825 $626.80 $525.27 16% $423.74 32% Pricing Examples Georgia (Southeast Region) HCPCS CODE HCPCS DESCRIPTION CURRENT SOUTHEAST SOUTHEAST 1/1/16 SOUTHEAST % REDUCTION AVERAGE % REDUCTION 1/1/16 1/1/16 24% E1390 OXYGEN CONCENTRATOR $ 180.92 $ 137.91 E1392 OXYGEN CONCENTRATOR, PORTABLE $ 51.63 $ 46.77 E0431 OXYGEN PORTABLE SYSTEM, GAS $ 30.42 $ 24.84 K0738 OXYGEN, PORTABLE GAS, USED TO FILL $ 51.63 $ 46.77 E0601 CPAP $ 100.96 $ 74.18 E0470 RAD, BILEVEL $ 240.01 $ 178.83 A7030 PAP, FULL FACE MASK $ 180.47 $ 141.39 A7034 PAP, MASK NASAL INTERFACE $ 112.53 $ E2402 NPWT PUMP $ 1,642.09 A6550 NPWT WOUND CARE SET $ 26.25 A7000 NPWT CANNISTER DISPOSABLE $ 8.90 $ 8.47 5% E0255 HOSPITAL BED, HI LO $ 102.86 $ 87.87 15% E0260 HOSPITAL BED, SEMI ELECTRIC $ 134.38 $ 102.60 24% E0277 LOW AIR LOSS MATTRESS $ 670.91 $ 459.49 32% E0143 WALKER, WHEELS $ 107.19 $ 80.22 K0001 MANUAL WHEELCHAIR STANDARD $ 54.88 $ 41.32 K0003 MANUAL WHEELCHAIR LIGHT WEIGHT $ 94.37 $ B4150 ENTERAL FORMULA, CATEGORY 1 $ 0.70 $ B4154 ENTERAL FORMULA, CATEGORY 4 $ 1.25 B4034 ENTERAL SUPPLY KIT, SYRINGE $ B4035 ENTERAL SUPPLY KIT, PUMP $ B4036 ENTERAL SUPPLY KIT, GRAVITY $ 8.20 B9002 ENTERAL PUMP WITH ALARM $ 121.70 E2365 BATTERY, POWER WHEELCHAIR $ 124.49 K0822 POWER WHEELCHAIR, GROUP 2 SLING SEAT $ 573.65 K0823 POWER WHEELCHAIR, GROUP 2 CAPTAINS CHAIR $ K0825 POWER WHEELCHAIR, GROUP 2 CAPTAINS CHAIR HEAVY DUTY $ SOUTHEAST 7/1/16 SOUTHEAST % REDUCTION AVERAGE % REDUCTION 7/1/16 7/1/16 24% $ 94.89 48% 48% 9% 9% $ 41.91 19% 17% 18% 18% $ 19.25 37% 36% 9% 9% $ 41.91 19% 17% 27% 27% $ 47.39 53% 54% 25% 25% $ 117.65 51% 49% 22% 22% $ 102.30 43% 43% 87.81 22% 22% $ 63.09 44% 44% $ 1,237.77 25% 25% $ 833.45 49% 51% $ 25.26 4% 4% $ 24.27 8% 8% 6% $ 8.04 10% 10% 15% $ 72.88 29% 31% 24% $ 70.81 47% 47% 32% $ 248.07 63% 63% 25% 26% $ 53.25 50% 52% 25% 27% $ 27.76 49% 54% 68.62 27% 29% $ 42.86 55% 57% 0.56 21% 22% $ 0.41 41% 43% $ 1.00 20% 21% $ 0.74 41% 42% 6.26 $ 4.79 24% 24% $ 3.31 47% 49% 11.95 $ 9.10 24% 25% $ 6.24 48% 51% $ 6.40 22% 23% $ 4.60 44% 46% $ 94.68 22% 23% $ 67.65 44% 47% $ 98.53 21% 20% $ 72.56 42% 38% $ 451.34 21% 22% $ 329.03 43% 43% 577.42 $ 438.53 24% 25% $ 299.65 48% 51% 636.20 $ 515.23 19% 20% $ 394.27 38% 40% Final Rule on Bundling • CMS has discretion to establish rules on whether covered items are paid for on a purchase or rental basis as long as total payments to contract suppliers are expected to be less than the total amounts that would otherwise be paid • Bundling will occur in no more than 12 new CBAs • Only for CPAP devices and standard power wheelchairs • Suppliers retain the title to the equipment and be responsible for repair and maintenance • No exact timeframe for when the special payment rules will be implemented. CBPs would be phased in as early as 2017 • As part of the process of allowing the rental agreements to continue, the grandfathered supplier would be paid based on existing rules • Non-contract suppliers have the option to continue rental agreements Final Rule on Bundling • Comparator CBAs will be located in the same state as the CBA where bundling CBAs are established • Selected based on factors that could include geographic location, general population, beneficiary population, patient mix, and utilization of items • Analysis strongly suggests that the benefits associated with paying on a continuous monthly rental basis outweigh the potential of increased copayments for the beneficiary • Subsequent rulemaking would be necessary to adopt special payment rules for other items or in more than 12 CBAs • The process for documenting medical necessity for items would be addressed outside the rulemaking process VENTILATOR CODING CHANGES EFFECTIVE JANUARY 1, 2016 Codes to be added effective January 1, 2016 (numbers not yet assigned): Exxx1 Home ventilator, any type, used with invasive interface (e.g., tracheostomy tube) Exxx2 Home ventilator, any type, used with non-invasive interface (e.g,. mask, chest shell) Codes to be discontinued effective December 31, 2015: E0450 E0460 E0461 E0463 E0464 The Medicare fee schedule amounts for code E0450 will be used to establish the fee schedule amounts for both new code Exxx1 and Exxx2, thereby restoring payment to the levels mandated by the statute for ventilators in general. VENTILATOR CODING CHANGES EFFECTIVE JANUARY 1, 2016 CMS intends to closely monitor use of new codes Exxx1 and Exxx2 to ensure that items used for the treatment of OSA are not being billed under these codes. Comments submitted: Pricing concerns Authority to make the pricing change Pricing based on obsolete equipment Lack of appropriate notice and comment requirements Special note: CMS removed the inclusion of E0464 in round 1 2017 CMS Proposes HCPCS Changes for Miscellaneous DME CMS is proposing to revise the coding used to describe miscellaneous durable medical equipment (DME) E1399. Likewise, HCPCS code K0108 describes a “wheelchair component or accessory, not otherwise specified” and is currently being used to bill for inexpensive DME, other covered DME, and replacement parts of wheelchairs. To promote more accurate payment of Medicare DME claims HCPC # UNITS ALLOWED $ PAID $ E1399 74,809 $4,720,843.18 $3,665,892.50 K0108 153,571 $21,510,709.52 $16,725,059.51 CMS is proposing replace HCPCS codes E1399 and K0108 with the following HCPCS codes KXXX1 DME, Miscellaneous, Purchase Price Does Not Exceed $150 -- CMS calculates that the 2015 fee schedule amount would be $97.94 KXXX2 DME, Miscellaneous, the Purchase Price Exceeds $150 -- CMS determines that the 2015 capped rental fee schedule amounts would be $80.60 for rental months 1 thru 3 and $60.45 for months 4 thru 13 KXXX3 Wheelchair Component or Accessory, Miscellaneous, the Purchase Price Does not Exceed $150 - CMS calculates that the 2015 fee schedule would be $72.56 KXXX4 Wheelchair Component or Accessory, Miscellaneous, the Purchase Price Exceeds $150 – CMS calculates that the 2015 fee schedule amounts for items in this code would be $53.41 for months 1 thru 3 and $40.06 for months 4 thru 13 KXXX5 Repair Part For Use With Beneficiary Owned DME, Other Than Wheelchair - Not Otherwise Specified – Payment individual consideration KXXX6 Repair Part For Use With Beneficiary Owned Wheelchair, Not Otherwise Specified – Payment individual consideration AAH Comments Submitted July 9, 2015 • The Agency reserves the right to make internal coding changes as necessary without notice. • AAH Comments: • Did not give the public sufficient notice of the Agency’s plan to adopt new codes and assign new payment amounts. • Proposes to create a new HCPCS coding logic that radically departs from the one the Agency has used over the last 25 years. • Uses a payment methodology that does not follow the structure Congress established for the DME fee schedules under the Social Security Act (SSA). • Trying to effect payment adjustments by way of coding determinations. • Will result in gross under or overpayment. Additional AAH Comments Submitted July 9, 2015 • CMS created miscellaneous codes for items that are unique or used infrequently and that generally do not warrant their own codes. These items are fundamentally different from other DME items and from each other so they cannot be grouped together under one code and code descriptor. • CMS’ rules for assigning HCPCS codes state clearly that the Agency considers products based on their similarity in function or therapeutic effectiveness among other criteria. • CMS’ decision to depart from the coding methodology that the Agency itself created and instead designate HCPCS code descriptors based on the price of DME products rather than their clinical function or features of the technology, is arbitrary and undermines the fee schedule statute. • AAHomecare recommends that CMS withdraw the proposal to create new codes for miscellaneous DME based on the item’s price and retain the current miscellaneous codes and pricing methodology based on the contractor’s individual • consideration. How You Can Help • Email or call the DC office of your Representative and Senators asking for support for a specific issue. • Action.AAHomecare.org has everything you need to email or call your elected officials. • Share your personal story and emphasize the specific role of homecare in your community. • Don’t give up. Keep up the volume. You Can Do Even More on Social Media • Just by sharing AAHomecare or Save My Medical Supplies information on your Facebook page, you are helping build awareness about our issues in your community. This is priceless PR and just one post can have a dramatic effect. • A recent Save My Medical Supplies Facebook post was shared 39 times- it reached more than 7,000 people. • Imagine if 20 more HME companies had shared that on their Facebook pages? Going Further: Engaging and Mobilizing Your Patients • Providers cannot be the only voice in the homecare debate. • We need our patients to speak up! They have the numbers that can prompt action. • AAHomecare has an entire campaign devoted to mobilizing patients- Save My Medical Supplies. Contact Information: Kim Brummett Vice President, Regulatory Affairs Kimb@aahomecare.org (202) 372-0750 Welcome