PATHOLOGICAL BEHAVIOR AFTER BRAIN INJURY
advertisement

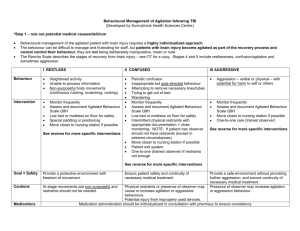
MANAGING AT RISK BEHAVIORS AFTER BRAIN INJURY Darryl L Kaelin MD Medical Director Frazier Rehab Institute BEHAVIORAL CHANGES • • • • Arousal / Attention Affect / Depression Psychosis Delirium / Agitation AGITATION • A heightened state of (cortical) activity marked by a complex of deficits in… • Cognition (Attn., Memory) • Behavior (Aggressive, Impulsive, Restless) • Affect (Emotionally Labile) DELIRIUM AFTER ABI • Difficulty in focusing, shifting, and sustaining attention • Agitation • Disturbed Sleep – Wake Cycle • Memory Impairment – Always happens during period of PostTraumatic Amnesia Agitation after TBI: Impact •Adults 3x more likely in first 6 months after head injury to show aggression than those with multiple traumatic injuries without head injury • •25% of adults showed aggressive behavior 60 months after discharge from inpatient rehabilitation unit for TBI • •70% of adults during inpatient TBI rehabilitation experience agitation • •Agitation has been shown to negatively affect rate of recovery in acute inpatient rehabilitation INCIDENCE • • • • Levin / Grossman (1978) – 30% Reyes (1981) – 50% Brooke (1992) – 11-35% Keyser / Kreutzer – 9% QUANTIFICATION • • • • • Neurobehavioral Scale Overt Aggression Scale Agitation Behavior Scale Behavior Log Sleep Charting AGITATION BEHAVIOR SCALE THE CALL • Johnny is screaming out that he wants to go home now. He is very confused and restless. Can I have some Ativan or Seroquel to calm him down please. • How do you respond? MANAGEMENT • R/O visual, hearing, and communication deficits • R/O medical causes (pain, metabolic, neurologic) • R/O pharmacological causes • R/O environmental causes CAUSES OF AGITATION •Identify and address possible cause/contributors including: • –Sleep disruption / alteration of sleep wake cycle • –Sources for discomfort • •Lines/catheters • •Unidentified injury (fracture, etc) • •Inadequate pain control • •Gastrointestinal distress (reflux, constipation, ileus) • Seizures • •subclinical epilepsy can present as intermittent aggression CAUSES OF AGITATION • – Electrolyte abnormality – Na+, Glucose, Calcium • Infection – UTI, Pneumonia, wound • –Neuroendocrine dysfunction • –Post-traumatic hydrocephalus • –Drug withdrawal (pain medications, other meds from ICU) • –Polypharmacy Environmental Management ENVIRONMENTAL MODIFICATION • Goal: Provide the least restrictive environment c/w safety of the patient • Adequate staff : patient ratio • Adequate Behavior Modification Training • Means of Implementation • Physical environment needs PHYSICAL ENVIRONMENT • • • • • • • Locked unit Alarm system Enclosure beds Minimize stimulus Room / Roommate assignment Sitter for supervision Restraints if necessary RESTRAINTS • Team determined • Physician prescribed • Documentation / Weaning • • • • Type Reason Goals for use Reevaluation daily BEHAVIOR MODIFICATION PROGRAM • Interdisciplinary approach • Documentation • • • • Cause of behavior Purpose of program (Goal) + or – Reinforcement Examples of responses to appropriate and inappropriate behavior NEUROTRANSMITTER THEORY • • • • • • Noradrenergic Serotonergic Dopaminergic Cholinergic Gabaminergic Peptidinergic PHARMACOLOGIC AGENTS • • • • • • • Neurostimulants Anticonvulsants Anticholinergics B – lockers (sympatholytic) SSRI Atypical Antipsychotics Lithium Fugate Et al. • Study of 129 physicians divided into brain injury experts or nonexperts surveyed. • Experts either had published two or greater articles on pharmacological interventions for TBI in the last 5 years, or had > or = 70% of their practice devoted to treating TBI • Experts most frequently prescribed carbamazepine, beta blockers, TCA’s • Nonexperts chose Haldol four times more frequently than experts Pharmacologic Tx •Cochrane review last updated 2008 • •6 studies met criteria (RCT’s) for metaanalysis • –Propranolol (2) • –Pindolol (2) • –Methylphenidate (1) • –Amantadine (1) • •Research supports use of -Blockers • •Effect seen within 2-6 weeks • •Response similar in both subacute and chronic timeframe HOW DO YOU DECIDE? • Observation • Theory • Trial and error BENZODIAZIPINES •Work on GABA molecule to create: • –Anxiolytic, sedative, antispasticity, anticonvulsant and AMNESTIC effects • •Effect duration varies based on medication – Short (1-8 hour half life) – e.g. midazolam, alprazolam – Intermediate (8-40 hour half life) – e.g. lorazepam – Long (>40 hours) – e.g. Diazepam, clonazepam BENZO: Side Effects •Side effects include the following: – Amnesia/memory loss – Increased daytime fatigue – Decreased concentration – Decreased alertness • •TBI causes the above effects as well • •Repeated use of benzodiazepines may slow/impair neuronal recovery after focal injury ANTIPSYCHOTICS Mechanism of Action • –Typical antipsychotics block D2-dopamine receptor • –Atypical antipsychotics have less D2 receptor activity • •Atypicals likely act on other neurotransmitter pathways, including serotonin, dopamine, 1-adrenergic, muscarinic, and histamine pathways Side Effects •Movement disorders • –Akathisia – one of more common movement disorders seen • a subjective sense of restlessness often accompanied by involuntary movements of the limbs or trunk • • Confusion • – Extrapyramidal Symptoms • – Tardive Dyskinesia – choreoathetotic or other involuntary repetitive movement • • Weight gain / Metabolic Syndrome • • Neuroleptic Malignant Syndrome (NMS) • • Seizures • • Prolonged QT COGNITION Cognitive impact of Antipsychotics • –Multiple animal studies have demonstrated either slowed cognitive improvement or reduced cognitive return with use of antipsychotic medications (both typical and atypical) • –One human study demonstrated negative cognitive impact with use of antipsychotics after TBI that improved with discontinuation of medication (Stanislav et al, 1997) TAKE HOME •Though atypicals may be relatively safer, likely all antipsychotic medications have detrimental effects with long term use (NMS, Tardive Dyskinesia, etc) • •May be appropriate to use atypical antipsychotics for short-term limited (PRN) use in agitation after TBI during the acute period when sedation is not a barrier Timing of Drug 100% 80% 60% Series 3 40% Series 2 Series 1 20% 0% Category Category Category Category 1 2 3 4 Beta-Blockers •Proposed mechanism of reducing hyperadrenergic activity • •Commonly used for periodic autonomic instability and dystonia (Storming) • •In retrospective studies shown to improve survival when used acutely after ABI • •Current prospective placebo study looking at effect of adrenergic blockade acutely after brain injury on survival and functional outcomes (clonidine and propranolol) B-Blockers: Research – 2 randomized placebocontrolled trials (Brooke 1992, Greendyke 1986) show benefit with propranolol for agitation in the weeks after injury (Brooke) and for aggressive behavior months and years after injury (Greendyke). ANTICONVULSANTS Various mechanisms based on medication: • – Decrease excitatory neurotransmitter activity • – Increase inhibitor neurotransmitter activity • – Reduce sub-clinical epileptic activity • •Seizures can be a source for aggression/confusion/disorientation • – Provide mood stabilization ANTICONVULSANTS Adult Research (all studies without controls) • –Valproic Acid • •Retrospective study of 28 patients with age range 13-89 demonstrated reduction of agitation symptoms with valproic acid in 26 (90%) patients • •Authors concluded it may be appropriate for alert, labile, impulsive, and disinhibited patients (Chatham Showalter et al, 2000) ANTICONVULSANTS –Carbamazepime • Prospective open trial in 8 patients (400-800 mg daily) had improved Agitated Behavior Scale (Azouvi et al, 1999) • 7 patients showed reduction in combativeness within 4 days (Chatham Showalter et al, 1996) ANTIDEPRESSANTS Proposed mechanism for decreasing agitation: • – Treatment of depression/anxiety that contribute to agitation/irritability • –Mood stabilization ANTIDEPRESSANTS •Very few studies looking at use of antidepressants with primary outcome of reduction of agitation • Multiple studies (including one prospective RCT) in adults addressing post-TBI depression noted reduction in symptoms of depression as well as reduction in agitation with treatment • A pilot study demonstrated improved mood, and improved attention and working memory with fluoxetine Kaelin’s Theory of Agitation • Two distinct foci of Agitation • Internal – Restless and more agitated when left alone and quiet • External – Aggressive and more agitated when stimulated or challenged Kaelin’s Theory of Agitation • Treatments • Internal cause of Agitation may be better treated with membrane stabilizing agents like anticonvulsants – CBZ, V. Acid • External causes of Agitation may be better treated with stimulants to improve attention and cognitive processing • Some may need both Kaelin’s Theory of Agitation • Beta-Blockers may be most beneficial when there appears to be sympathetic overdrive (HR, BP, sweating, outbursts) • SSRIs may be most beneficial when there is a clear emotional component ( depression, anxiety). Summary: Little evidence to guide us so: • –Identify and treat contributors to agitation when possible • –Treatment should include nonpharmacologic environmental and behavioral management • –Monitor response to intervention • •Agitated Behavior Scale (may be most appropriate for adult patients) • –Avoid Polypharmacy • • if something doesn’t work, stop it before adding more Questions ? • Darryl Kaelin, MD • 502-584-3377 • THANK YOU !!