assesment of the Reproductive System
advertisement

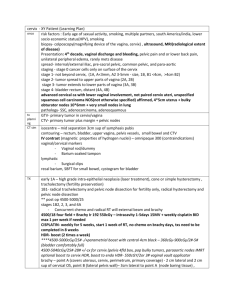
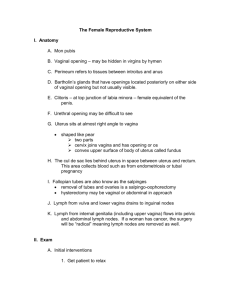
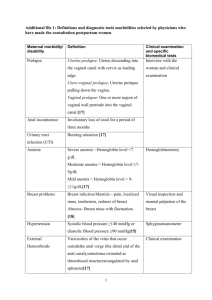
Assessment of the Reproductive System • The nurse is often the first health care professional to assess the client with a reproductive system disorder. Basic assessment of the reproductive system should be part of every complete physical examination. Assessment techniques • History • The nurse uses data about client’s age, sex, and culture to assess the risk for certain diseases. The nurse considers the client’s age in evaluating the reproductive system. • Personal history( the nurse assesses he client’s health habits, such as diet, sleep, and exercise patterns.) • Family history helps to determine the client’s risk for conditions that affects reproductive system functioning. • Diet history is often critical for the correct interpretation of presenting symptoms of the reproductive system. • Social history of the client provides insight into the whole person, including stressors, job history, education. Menstrual History • • • • • • • • • • Age at menarche Interval, regularity, duration and amount of flow Date of most recent menstrual period Was most recent menstrual period normal? Dysmenorrhea Premenstrual symptoms (e.g., swelling, headache, mood swings, pain) Abnormal uterine bleeding Symptoms of menopause Age at menopause Postmenopausal bleeding Obstetric History • Number of pregnancies, live deliveries, stillbirths, abortions • Difficulties with pregnancies, deliveries • Birth weight of babies • Problems with infertility Use of Contraception • Type used (past and present) • Difficulties with method, suitability • If discontinued, reasons for doing so Sexual History • Sexual orientation • Regularity of intercourse • Number of partners in the past 12 months • Associated symptoms (e.g., pain, postcoital bleeding) • Sexual dysfunction Current health problem • If a client seeks medical attention for a problem related to the reproductive system, the nurse asks additional questions to explore the chief complaint. 1. Onset (sudden or gradual) 2. Chronology 3. Current situation (improving or deteriorating) 4. Location 5. Radiation 6. Quality 7. Timing (frequency, duration) 8. Severity 9. Precipitating and aggravating factors 10.Relieving factors 11.Associated symptoms 12.Effects on daily activities 13.Previous diagnosis of similar episodes 14.Previous treatments 15.Efficacy of previous treatments Most complaints concern • pain, • discharge, masses, •and reproductive functioning Pain • Onset, location, radiation, character, severity • Relation to menstruation • Aggravating and relieving factors • Use of analgesics and their effect • Associated gastrointestinal, urinary or vaginal symptoms • Are symptoms related to an encounter with a new sexual partner? • The nurse should not assume that the initial medical diagnosis is conclusive Vaginal Discharge • • • • The nurse asks about: Onset, color, odor, consistency, quantity Relation to menstrual period Associated symptoms (e.g., rectal or urethral discharge, vaginal itch or burning, urinary symptoms, malaise, abdominal pain, fever) • Relation to medication use (e.g., antibiotics, steroids) • History of previous vaginal or pelvic infections and their treatment Masses any reported masses in the breast should be evaluated • Soreness, tenderness and their relation to menstrual cycle • Redness, swelling, nipple discharge • Change in contour, presence of masses • Is client breastfeeding? Bleeding • Heavy bleeding or lack of bleeding may concern the woman. • The possibility of pregnancy is considered in any sexually active woman with amenorrhea. Any postmenopausal bleeding needs to be evaluated. • The nurse asks when the bleeding occurs in relation to certain events, such as the menstrual cycle or menopause, intercourse, trauma. In additional, the nurse notes the presence of associated symptoms Other Associated Symptoms • Ulcerations • Persistent lesions • Sense of pelvic relaxation (pelvic organs feel as though they are falling down or out) • Infertility • Pelvic infection Examination of the Female reproductive System • General 1. Apparent state of health 2. Appearance of comfort or distress 3. Color (e.g., flushed or pale) 4. Nutritional status (obese or emaciated) 5. Match between appearance and stated age Breast Examination • Inspect breasts with client in sitting and then in supine position • Assess symmetry, contour, skin color, thickening, dimpling or retraction of overlying skin, veins, redness, streaking • Examine nipples for symmetry, discharge, erosion, crusting, color • Palpate breast and axilla for consistency, tenderness, masses Lymph Nodes • Palpate the following areas and identify enlargement, tenderness, mobility and consistency: • Upper extremity: supraclavicular area, infraclavicular area, axilla, epitrochlear nodes • Lower extremity: inguinal nodes Lymphatic System • Enlarged, painful nodes (in axilla, groin) • • Lymph Node Areas Adjacent to Breast Area A Pectoralis major muscle B Axillary lymph nodes: levels I C Axillary lymph nodes: levels II D Axillary lymph nodes: levels III E Supraclavicular lymph nodes F Internal mammary lymph nodes Examination of the Female Pelvis Equipment Needed • Exam Table Equiped with Stirrups • Flexible Light Source • Vaginal Specula in Various Sizes • Warm Running Water • Lubricating Jelly General Considerations • The patient must have an empty bladder. • The patient must be appropriately gowned and draped. • Use non-sterile gloves on both hands. Double-glove your dominant hand if you intend to perform a rectal or rectovaginal exam. • Properly dispose of soiled equipment and supplies. • Both male and female examiners should be chaperoned by a female assistant. • Always tell the patient what you are about to do before you do it. • The breast exam is usually done just before routine pelvic exams. Examination of the External Genitalia Positioning the Patient • • • • Start with the patient lying supine on the exam table with the head elevated 30 to 45 degrees. Assist the patient to place her heels in the stirrups. Adjust the angle and length to "fit" the patient. Have the patient slide her hips down until she contacts your hand at the edge of the table. Have the patient relax her knees outward just beyond the angle of the stirrups. Vulvar Self-Examination • The examination of the external female genitalia is an excellent time for teaching about vulvar self-examination. • Perform a vulvar self-examination monthly between menstrual periods if you are older than 18 years or if you are sexually active. • Sit in well-lighted area on a soft surface (bed ). • Use a handheld mirror to visualize your external genitalia. • Examine the area around the vaginal opening from the mons pubic to the perianal area. • Feel and visually inspect the area. • Report to your health care provider new nodes, warts, growths of any type, ulcers, sores, blisters, change in skin color, painful areas, areas of itching or inflammation, or any change in vaginal discharge. • • • • • • Pelvic examination A pelvic examination is recommended every 1 to 3 years for women older than 18 years or younger, sexually active adolescents. The woman should not be douche for at least 24 hours before the pelvis examination, because doing so may prevent an accurate evaluation of smears, cultures, and cytologic data. • Speculum Exam Warm and lubricate the speculum by holding it under running tap water. Announce what you are going to do and then touch the patient on the thigh with the speculum before proceeding. Expose the introitis by spreading the labia from below using the index and middle fingers of the non-dominant hand (peace sign). Insert the speculum at a 45 degree angle pointing slightly downward. Avoid contact with the anterior structures. Once past the introitis, rotate the speculum to a horizontal position and continue insertion until the handle is almost flush with the perineum. • • • • • • Open the "bills" of the speculum 2 or 3 cm using the thumb lever. Position the bills so that the cervix "falls" in between. Secure the speculum by turning the thumb nut (metal speculum) or clicking the ratchet mechanism (plastic speculum). Do not move the speculum while it is locked open. Observe the cervix and vaginal walls for lesions or discharge. Obtain specimens for culture and cytology as indicated. Withdraw the speculum slightly to clear the cervix. Loosen the speculum and allow the "bills" to fall together. Continue to withdraw while rotating the speculum to 45 degrees. Again, avoid contact with the anterior structures. Replace the drape while you prepare for the rest of the exam. Reassure the patient, if the exam is normal so far, say so. Vagina • • • • • • • Inflammation Atrophy Discharge Lesions, ulcerations, excoriation Masses Induration or nodularity Relaxation of perineum (ask client to bear down and observe for any bulging of vaginal walls) Cervix • Position, color, shape, size, consistency (see below) • Discharge • Erosions, ulcerations • Cervical tenderness • Bleeding after contact Consistency of cervical tissue: normal cervix is pink and feels firm, like the tip of the nose; in pregnancy, the cervix is bluish and feels softer, like the lips of the mouth Bimanual Exam • • • • • • Apply a small amount of lubricant to the index and middle fingers of your dominant hand. Uncover the vulva and lower abdomen by moving the center of the drape away from you. Announce what you are going to do and then touch the patient on the thigh with the back of your hand before proceeding. Spread the labia and insert your lubricated index and middle fingers into the vagina. Avoid contact with the anterior structures. Place your other hand on the patient's lower abdomen. Examine the cervix: – Palpate the cervix with your index finger noting size, shape, and consistency. – Gently move the cervix side to side between your fingers and note mobility and tenderness. – Gently lift the cervix forward and note mobility and tenderness. Examine the anterior uterine fundus: Continue to lift the cervix with the vaginal hand. Press downward with the abdominal hand and palpate the uterus (if possible). Note consistancy and tenderness. Attempt to estimate uterine size. Examine the adnexal structures: Pull back vaginal hand to clear cervix. Reposition vaginal hand into the right fornix, palm up. Sweep the right ovary downward with the abdominal hand 3 or 4 cm medial to the iliac crest. Gently "trap" the ovary between the fingers of both hands (if possible). Note its size and shape along with any other palpable adnexal structures. Pull back and repeat on the left side. Replace the drape and assist the patient to remove her feet from the stirrups and sit up. Reassure the patient, if the exam is normal, say so. Leave the room and allow the patient to dress before continuing with the consultation. Uterus • • • • • • Position Size Contour Consistency of uterine tissue Mobility Pain on movement Adnexa • Ovaries cannot usually be felt unless the client is very thin or the ovaries are enlarged. • Tenderness • Masses • Consistency • Contour • Mobility • Adnexal pain on movement of cervix or uterus (Chandelier's Sign): Extreme pain elicited with movement of the cervix during bimanual pelvic examination. Indicates pelvic inflammatory disease. • Tenderness with cervical motion is an important sign of pelvic disease. You should both observe the patient's face and ask her if the examination is painful in any way. • Your ability to palpate the uterus and ovaries will depend on the patient's anatomy, the size of your hands, and your level of skill. Diagnostic Assessment • Laboratory tests • The Papanicolaou Test (Pap smear) is cytologic study that is effective in detecting precancerous and cancerous cells from the cervix. You will obtain a (Pap) smear and other specimens as part of most pelvic exams Blood studies • • • • Pituitary gonadotropin Steroid hormones Serologic test Syphilis detection Microscopic Studies • Wet preparation (wet smears). The examiner can obtain secretion from the vaginal pool at the beginning of a speculum examination. Specimens also can be obtained from the vaginal walls, labia, or vulva during the examination. The specimens are placed on glass slides and are treated with a wet preparation such as potassium hydroxide (KOH). The slides are examined under microscope to confirm or rule out the presence of a pathogen. Radiographic examination • General X-ray Studies • Pelvic masses, calcified tumors or fibroids, dermoid cysts, and metastatic bone changes may be evident. No specipic client preparation is nedded. • Computer tomography (CT) scans can detect and evaluate masses and lymphatic enlargement from metastasis. This scan can differentiate silid tissue masses cystic or hemorrhagic structures. Hysterosalpingography • is an x-ray study of the cervix, uterus, and fallopian tubes and it is performed after the injection of a contrast medium. This test is used in infertility workups to evaluate tubal anatomy and patency and uterine abnormalities. The client is placed in the lithotomy position. A speculum is inserted, and the cervix is visualized. Radiopaque oil is inserted through the cervix, uterus, and fallopian tubes. If the fallopian tubes are patent, the contrast material spills into the peritoneal cavity Mammography • Is the x-ray study of the soft tissue of the breast. It asses differences in the density of breast tissue. It usually necessitates two low-dose x-ray views of each breast:a view from the side and a view from above. • Follow-up care. If the result are not communicated at the time of the mammogram, the woman should know when to expect the result. She should be assessed for her knowledge of breast selfexamination. Other diagnostic tests • Ultrasonography is a nonradiographic diagnostic technique. The client should have a full bladder to enable visualization of the uterus with abdominal ultrasonography; a full bladder is not necessery for tranvaginal scans. There is no specific follow-up care for the client after this procedure. • Magnetic Resonance Imagine(MRI).this scan effectively distinguishes between normal and malignant tissues. Endoscopic Studies Colposcopy is suited for inspection of the cervical epithelium, vagina, and vulvar epithelium. This procedure can locate the exact site of precancerous and malignant lesions for biopsy. The woman is placed in the lithotomy position. The clien should not douche or use vaginal preparations for 24-48 hours before the examination. The physician locates the cervix, or vaginal site, through a speculum examination. Cervix has to be cleaned from secretions. Acetic acid, 30%, applied to the cervix acts as a mucolytic agent to acceptuate important morphologic features. The physician uses a colposcope or microscope to inspect the area in question.a biopsy also may be taken if abnormal cells are seen. After the procedure, the nurse assists the woman as for a pelvic examination and provides suplies to clean perineum. Laparoscopy • is highly accurate diagnostic tool for exploring the pelvic cavity. It is preferable to a laparotomy for minor surgical procedures. • After the procedure the client requires postoperative care similar to that for other clients after general anesthesia but is usually discharged on the day of the surgery. Hysteroscopy • is endoscopic examination that permits visualization of the interior of the uterus and the cervical canal. the client receives the same preparation as for pelvic examination. • Care is the same as that after a pelvic examination. Biopsy studies • Cervical biopsy. Cervical tissue is removed for additional cytologic study. a • Endometrial biopsy and aspiration.Both are used to obtain cells directly from the lining of the uterus in women at risk for cancer of the endometrium. Breast biopsy and aspiration • An incisional biopsy is the surgical removal of tissue from a breast mass. An excisional biopsy removes the mass itself for hystologic(cellular) evaluation. Aspiration biopsy is the removal of fluid or tissue from the breast mass through a largebore needle. • Postoperative discomfort is usually mild and is controlled with analgesic administration or the use of the heating pad.