Transmission-Based Precautions
advertisement

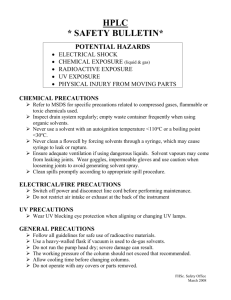
Annual Nursing Competency Updated 2013 1 Appropriate Hand Hygiene Standard Precautions Transmission-based Precautions Wear PPE as appropriate Respiratory Etiquette Get recommended/required Vaccinations: includes Influenza Environmental cleanliness & appropriate waste management Proper cleaning, sterilization and disinfection of patient care equipment Aseptic Practices to prevent device related infections Utilize Resources which include Policies and Procedures 2 Healthcare workers can get 100s to 1000s of bacteria on their hands by doing simple tasks like: pulling patients up in bed taking a blood pressure or pulse touching a patient’s hand rolling patients over in bed touching the patient’s gown or bed sheets touching equipment like bedside rails, over bed tables, IV pumps Casewell MW et al. Br Med J 1977;2:1315 Ojajarvi J J Hyg 1980;85:193 3 Hand Hygiene is performed on ungloved hands using: Hospital-approved hand sanitizer (foam or gel) OR Water and soap at sinks located throughout the hospital. Use soap and water when hands are visibly dirty or contaminated with blood or body fluids. Alcohol foam or gel is appropriate if your hands are not visibly soiled. 4 At DRaH, performance of hand hygiene is measured at TWO basic and important patient care moments. “Before Patient Interaction” immediately before or at the time of entering a patient room or area* & “After Patient Interaction” immediately after or at the time of exiting a patient room or area* * i.e. PACU, radiology or ambulatory area 5 Clean your hands: before donning sterile gloves or exam gloves inserting invasive devices into patients moving from a contaminated body site to a clean body site eating or drinking touching your face after contact with patients’ intact skin contact with patient equipment, linen, supplies contact with body fluids, excretions, mucous membranes, non-intact skin, and soiled dressings after removing gloves using the restroom coughing or blowing your nose 6 Soap & Water: Apply hospital-approved soap to hands Rub hands together vigorously, paying particular attention to between fingers, under fingernails, and backs of hands, for 15 seconds Rinse hands in a stream of warm water (avoid extreme hot or cold water) Dry hands with paper towel Use towel to turn off water Alcohol Foams, Gels, & Liquid Alcohol Hand Rub Apply the manufacturer’s recommended amount of alcohol-based product to palm of one hand (for foam that’s about the size of a golf ball; for gels or liquids that’s one push on the dispenser lever) Rub hands together, covering all surfaces of hands, fingers, & wrist until hands are dry. 7 Reminders : Alcohol Hand Rubs Are Not Indicated: If hands are visibly dirty or contaminated with blood, body fluids, or other material After contact with patients with Clostridium difficile (C. diff) After exposure to known or suspected Bacillus anthracis (anthrax) Direct patient care providers must keep natural nail tips equal to ¼ inch long or less. No artificial nails, gels, overlays etc. for direct care givers. The hands, including the nails and surrounding tissue should be free from infection and /or inflammation for personnel having patient contact. Healthcare workers with dermatitis or areas of broken, non-intact skin or potential infection shall refrain from all patient care activities. 8 Before & After Hand Hygiene: 9 Require that blood, body fluids, secretions and excretions(excluding sweat), mucous membranes and non-intact skin of all patients be treated as potentially infectious. Requires putting the appropriate barrier (i.e. gloves, gown, mask, eye protection) between the healthcare worker and the blood or body fluids of any patient. “If it is wet and not yours, then use a barrier.” 10 Handle all blood/body fluid as if infectious Handle all items contaminated with blood or body fluid as if infectious Follow appropriate Hand Hygiene Practices Follow Cough/Respiratory Etiquette Follow Safe Injection Practices Use a surgical mask when performing spinal procedures(LP, epidural) Handle all sharps with care Discard sharps in rigid containers Wear appropriate PPE Report exposures ASAP Enforce designated eating areas (in clinical setting to prevent contamination of food/beverages from blood or body fluids) Standard Precautions are designed to reduce the risk of transmission 11 Choose PPE appropriate for the activity to prevent exposure, PPE includes: Gloves Gowns Face Masks Eye Protection 12 Standard Precautions Include: Respiratory Etiquette Instruct symptomatic persons to: cover mouth/nose when sneezing/coughing use tissues and dispose immediately after use clean hands after contact with respiratory secretions wear surgical mask if tolerated or maintain spatial separation, >3 feet if possible. 13 To prevent the transmission of infections in a healthcare setting Safe Injection Practices require: Use a sterile, single-use, disposable needle and syringe for each injection given Dispose of needle and syringe properly after one use Whenever possible, use of single-dose vials is preferred over multiple-dose vials Do not use single bags or bottles of IV solution as a common source for multiple patients 14 Do not recap, bend, break, or hand-manipulate used needles. If recapping is required, use a one-handed scoop technique only. Use safety features when available and place used sharps in an OSHA approved punctureresistant container. 15 All specimens of blood and body fluids should be placed in a well constructed DUHS approved container with a secure lid to prevent leaking during transport. A clean outer container / bag must be utilized in transport to prevent exposure. This container / bag should be labeled with a biohazard symbol for identification. 16 17 Follow established procedures for routine care, cleaning, and disinfection of environmental surfaces, especially frequently touched surfaces in patientcare areas. Only hospital approved cleaning products should be used Follow manufacturer directions for cleaning equipment Ensure all patient care items, bedside equipment, and frequently touched surfaces receive daily disinfection. Privacy curtains are changed/cleaned when visibly soiled, and at discharge for Contact Isolation rooms. Immediately clean spills of any blood or body fluids with approved DRaH disinfectant. 18 Transmission-based Precautions are designed for patients with suspected or documented infection with microorganisms that are highly transmissible. Should be used in addition to Standard Precautions. Refer to Standard & Transmission-based Precautions Policy located on the DRAH Intranet 19 In addition to the physician the RN can initiate transmission-based precautions The patient’s physician is to be notified and an order written in the medical record Contact Infection Prevention for assistance with isolation requirements Educate the patient & their family on: The reason for precautions How to adhere to appropriate isolation practices Don’t Forget…Document in the medical record that education was provided! Place Signage on door or cubical entrance to patient’s environment Enter order in Medical Record Communicate isolation precaution at all levels of handoff between care givers Signage should remain in place until room is cleaned at discharge or transfer 20 21 22 23 24 Educate the patient & their family on: The reason for precautions How to adhere to appropriate isolation practices Document in the medical record that education was provided Patient Education is currently available on all units: FAQs MRSA FAQs VRE FAQs Clostridium difficile Understanding Isolation Precautions Understanding Multi-drug Resistant Organisms Hand Hygiene for Patients & Visitors 25 Patients on transmission-based (isolation) precautions should not leave their room unless medically necessary (i.e. part of plan of care). Whenever feasible, the patient’s procedure shall be done in the patient’s room. If a procedure cannot be done in the patient’s room, then it is preferred that the patient’s procedure be scheduled as the last patient. PPE is not to be worn in transport unless: healthcare worker transporting the patient is providing direct patient care during transport. A second healthcare worker assists in transport, is considered “clean” and shall not wear PPE. shall proceed ahead of patient and transport staff to open doors, press elevator buttons, etc. 26 When ambulation/transport is necessary: Upon leaving room, patient to perform hand hygiene. A clean gown should be placed on the patient. Clean linens shall be placed over the patient on the stretcher or wheelchair to serve as a barrier. Patients with draining wounds shall have a clean/dry dressing. Patients on Droplet or Airborne precautions shall wear a surgical mask when outside their room. Personnel in the receiving area shall be notified of the isolation status of the patient prior to transport. Isolation status shall be communicated in patient care handoff 27 Visitors who cannot comply with wearing of required PPE may not visit with patient(s) on transmission-based (isolation) precautions. Children less than 12 years old should not visit patients on transmission-based (isolation) precautions due to potential inappropriate PPE use. Exceptions may apply for special circumstances with Infection Prevention input and physician approval. Visitors of patients on Airborne Precautions should be limited to immediate adult household members who have had recent contact with the patient Visitors shall wear a N95 respirator while in the patient’s room. Visitors are not fit-tested for the N95; however, healthcare staff shall demonstrate how to wear the N95 respirator. (Refer to Patient Care Manual: Tuberculosis Control Plan attachment for fitting a respirator). Provide education and document completion 28 Contact- Wear gown and gloves. Used for patients with known or suspected MRSA, VRE, ESBLs, RSV, Bedbugs, Shingles, etc. Contact /Special Enteric- Wear gown and gloves. Used for patients with known or suspected Clostridium difficile, Norovirus, etc. (soap and water only for Hand Hygiene) Droplet- Wear Surgical mask. Used with patients with known or suspected Meningitis, Influenza, Pertussis, etc. Airborne- Wear N95 mask or PAPR. Used for patients with TB or r/o TB, active Chickenpox, Measles, etc. Special Airborne/Contact-Wear gown, gloves, mask(N95 or PAPR). Used for patients with emerging infectious agent of unknown cause/origin 29 Contact Precautions are used for patients who are suspected or known to be infected with organisms that can be transmitted by: direct contact with the patient (hand or skin-to-skin contact that occurs when performing patient care activities that require touching the patient’s dry skin) indirect contact with environmental surfaces or patient-care items in the patient’s environment. This isolation category requires the use of gloves and gown to enter the room regardless of patient contact. Examples: MRSA VRE Rashes ESBLs (Extended-spectrum Beta-lactamase resistance) KPC (Klebsiella pneumoniae Carbapenem-resistance) Varicella (Chicken Pox) Scabies Bedbugs Draining Wounds Shingles (non disseminated) Use in addition to Standard Precautions! 30 Special Enteric Precautions are designed to reduce transmission of organisms that can easily survive in the environment once shed from the human body. Special Enteric Precautions include Contact Precautions plus hand hygiene by soap and water. Examples: Clostridium difficile (C.diff) Norovirus Hand hygiene with soap and water must be used when leaving the patient’s room / environment in order to remove the organism and/or spores. Use in addition to Standard Precautions! 31 Droplet Precautions are for known or suspected infections with microorganisms transmitted by droplets (large-particle droplets greater than 5 µm in size). Droplets are generated by the patient during: Coughing Sneezing Talking Performance of procedures involving the respiratory tract. Examples: Meningitis Influenza Mumps Pertussis Transmission can occur by: direct contact with droplets contact with objects recently contaminated with respiratory secretions. Use in addition to Standard Precautions! 32 Airborne Precautions are used for known or suspected infections with microorganisms transmitted by airborne droplet nuclei (small particle residue of 5 µm or less in size). Place the patient in a private room that has monitored negative air pressure in relation to the surrounding areas. If negative air pressure room in unavailable, portable HEPA filter units should be used. Examples: Mycobacterium Tuberculosis (TB) Varicella (Chicken Pox) Measles HEPA should remain in use in the room for 40 minutes after patient discharge and before admitting another patient (CDC TB Guideline, 2005). Keep the room door closed and the patient in the room. Use in addition to Standard Precautions! 33 This isolation category requires the use of respiratory protection: Positive Air Purifying Respirator (PAPR) or N95 mask that has been fit-tested on the user for entry into the patient’s room. Remember, you must be fit-tested ANNUALLY for the N95 mask. A Seal Check should be performed to ensure a proper fit once N95 applied). If a proper fit cannot be achieved, do NOT enter the area requiring respiratory protection. In the case of varicella or measles, the individual does not require a PAPR/N95 if immunity is documented. 34 Pathogen/Disease New Diagnosis Arrived with Clostridium Difficile Infection Contact isolation along with Contact isolation along with special (CDI) special enteric precautions should enteric precautions should be be continued in all hospitalized continued in all hospitalized patients Note: DUHS guidelines patients with known CDI until the with known CDI until the time of differs from current time of hospital discharge. hospital discharge. CDC recommendations (i.e. is stricter than CDC) Patients hospitalized longer than 2 Patients hospitalized longer than 2 weeks following resolution of weeks following resolution of symptoms and treatment of CDI symptoms and treatment of CDI may may be removed from contact be removed from contact isolation isolation and special enteric and special enteric precautions with precautions with Infection Infection Prevention approval when Prevention approval when there the patient has no signs and are no signs and symptoms of symptoms of CDI. CDI. ***** Refer to DRAH Standard & Transmission Precautions Policy for complete list of discontinuation criteria. The patient’s room is then The patient’s room is then terminally terminally cleaned (may need to cleaned (may need to transfer transfer patient to new room). patient to new room). 35 Pathogen/Disease New Diagnosis Arrived with Methicillin Resistant Patients with a NEW (+) positive culture for MRSA or Patients arriving with or readmitted with a previous culture-positive for MRSA (< 1 year ago) Staph Aureus (MRSA) a positive culture (+) within the past year are to remain on contact precautions until they: should be placed on contact isolation until the criteria for discontinuation of isolation is met. Are discharged from our facility or they are shown to be MRSA negative by meeting ALL of the following criteria: Are discharged from our facility or they are shown to be MRSA negative by meeting ALL of the following criteria: • • • • • ***** Refer to DRAH Standard & Transmission Precautions Policy for complete list of discontinuation criteria. Off all antibiotics for 24 hours Have three (3) consecutive negative nasal swabs, each one obtained no less than a week apart (i.e., swabs must be at least 7 days apart). Have three (3) consecutive negative cultures from the original site, each one obtained no less than a week apart. If unable to obtain culture from original site, this is not necessary. • Off all antibiotics for 24 hours Have three (3) consecutive negative nasal swabs, each one obtained no less than a week apart (i.e., swabs must be at least 7 days apart) Have three (3) consecutive negative cultures from the original site, each one obtained no less than a week apart. If unable to obtain culture from original site, this is not necessary Note: Most patients infected or colonized with MRSA Patients with a (+) positive MRSA culture > 1 remain colonized with MRSA for months after initial year ago should be placed on contact isolation until infection despite treatment; thus routine cultures to they are shown to be MRSA negative by meeting demonstrate resolution of colonization are generally ALL of the following criteria: not advisable. These patients should automatically • The patient must be off antibiotics be placed on contact isolation. active against MRSA. • One (1) negative culture from nares. • All signs of the original site of infection have resolved, and if possible obtain culture from original site. 36 Central Line Associated Infections (CLABSI) Catheter Associated Urinary Tract Infections (CAUTI) Surgical Site Infections (SSI) 37 CRUSH CLABSI 38 COUNTER CAUTI 39 SILENCE SSI 40 Perform proper HAND HYGIENE 41 Infection Prevention & Control Department: John Engemann, MD Connie Clark BSN, RN, CIC (x3166) Brittain Wood BSN, RN (x3076) Please feel free to contact us 24/7! 42 Now it is time to review your knowledge. Please click next to begin. 43 PROPERTIES On passing, 'Finish' button: On failing, 'Finish' button: Allow user to leave quiz: User may view slides after quiz: User may attempt quiz: Goes to Next Slide Goes to Previous Slide After user has completed quiz After attempting quiz 2 times