BREATHING - The Asthma Foundation
advertisement
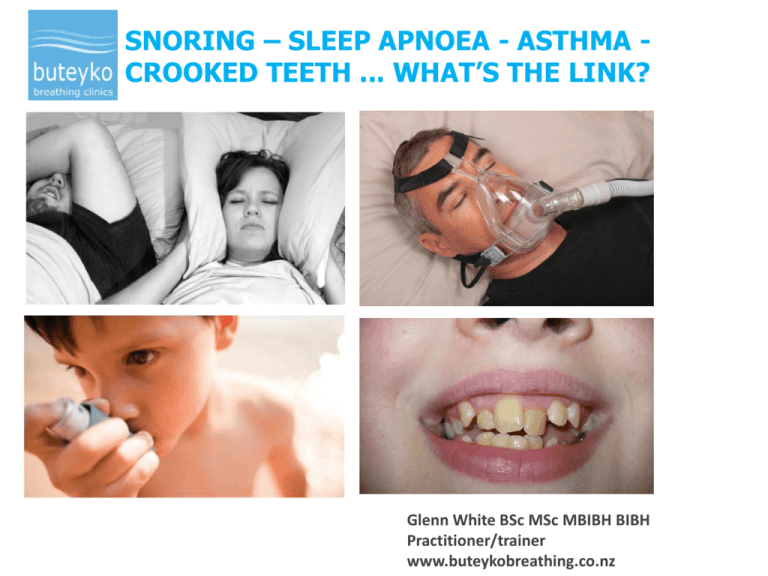
SNORING – SLEEP APNOEA - ASTHMA CROOKED TEETH ... WHAT’S THE LINK? Glenn White BSc MSc MBIBH BIBH Practitioner/trainer www.buteykobreathing.co.nz FUNCTIONAL BREATHING Breathing Parameter Normal characteristics Route Nose: rest, physical exercise, sleep Location (dominant) Diaphragm Respiration rate 8-12 breaths per minute Minute volume 4-6 litres per minute Tidal volume 500 ml per breath Feel of breathing Easy, comfortable, satisfying Rhythm Regular, smooth Sound Inaudible; at rest, sleep Heart rate 60-80 beats per minute After Graham, T 2012, Relief from snoring and sleep apnoea DYSFUNCTIONAL BREATHING Breathing Parameter Characteristics Route mouth breathing or heavy nose breathing Location (dominant) Thoracic dominant Respiration rate > 14 breaths per minute Minute volume > 9 litres per minute * Appearance of breathing obvious upper chest or abdominal movement Feel of breathing Heavy, windy full breaths Rhythm Irregular: sighs, yawns, coughs, sniffs Sound Audible; at rest, sleep (snoring) After Graham, T 2012, Relief from snoring and sleep apnoea DAYTIME SYMPTOMS OF DYSFUNCTIONAL BREATHING Blocked or runny nose Throat clearing Open-mouth breathing Short of breath on exertion Heavy laboured breathing Upper chest breathing pattern Wheezing, asthma, chest tightness Anxiety/ panic attacks Sighing or frequent deep breaths Dry mouth Frequent yawning Difficulty swallowing Irritable cough Gastric reflux HOW BREATHING CAN DISRUPT SLEEP • difficulty getting off to sleep • restless sleep, frequent waking • waking up-tired www.buteykobreathing.co.nz SYMPTOMS OF BREATHING DISORDERED SLEEP Snoring restless sleep sleep apnoea restless leg syndrome insomnia increased nasal congestion vivid dreams-nightmares teeth grinding night-time cramps sleep-walking, sleep-talking frequent urination, bed wetting morning headache night thirst, dry mouth on waking blocked nose on waking groggy on waking morning thirst asthma, night-time coughing high morning pulse night-time anxiety/panic attacks messy bed on waking www.buteykobreathing.co.nz MORNING BREATH THE LUNGS AND CARBON DIOXIDE (CO2) One of the lung’s primary functions is to maintain optimum levels of O2 and CO2 in airways and blood Mouth breathing and over-breathing result in CO2 loss resulting in CO2 deficit (hypocapnia) The Importance of CO2 • An optimal level of CO2 is essential in airways and blood for oxygen delivery to brain and body tissues • CO2 is a broncho/ vaso dilator • Optimal PaCO2 is essential for the release of oxygen 1 from blood to body tissues (The Bohr Effect) 1 DAVIS FREED Am.J.Respir.Crit. Care Med.2001, 785-789 OVER-BREATHING AND CO2 LOSS REDUCES BRAIN OXYGEN MRI SCAN red - yellow = highest oxygen dark blue = least oxygen The right hand image shows a 40% reduction in brain oxygen after one minute of big volume breathing. This explains the sensation of dizziness that often accompanies a panic attack. (source Litchfield 1999) Dysfunctional breathing = hyperventilation Hyperventilation = breathing more than the medical norm Normal resting minute volume for a 70-kg human 4-6 litres/min for older physiological textbooks 6-9 litres/min for some modern textbooks > 9 litres/min is defined as hyperventilation www.buteykobreathing.co.nz STRESS MAKES US BREATHE MORE If the stress is prolonged over-breathing becomes habitual • stress in workplace, school, home, bereavement, financial • illness, infection • lack of exercise, athletes over-training • over-eating, skipping meals, too much refined carbs, low protein • some medications; e.g. bronchodilator medications • caffeine, nicotine, alcohol, recreational drugs • promotion of deep breathing techniques • computer games, excessive use of personal technologies IN SUMMARY LIFE www.buteykobreathing.co.nz HUMAN BREATHING VOLUMES HAVE DOUBLED IN FIFTY YEARS Minute Ventilation, litres per mniute 14 12 12 11 12 12 10 8 6.9 6 6 4.9 5.3 7.8 4.6 4 2 0 Norm 1929 1939 1939 1950 1980 1990-96 1997 1998-99 Information sourced from 24 medical studies – Rakhimov 2005 2000s CONSEQUENCES OF OVER-BREATHING: • • • carbon dioxide deficit – hypocapnia • • • disruption in breathing regulation • • • • reduced oxygenation • histamine production dehydrated and inflamed airways increased mucus production smooth muscle constriction - bronchial, cardiovascular, gastrointestinal, urinary - broncho-spasm, vaso-constriction, Verigo-Bohr Effect pH disturbance bigger breathing volume = more inhaled irritants www.buteykobreathing.co.nz MOUTH BREATHING • The teeth sit in the neutral position between the cheeks and the tongue. • During nasal breathing the tongue rests in the roof of the mouth. • During mouth breathing the tongue drops to the floor of the mouth and the cheeks then exert force on the teeth causing constriction of the maxilla. MOUTH BREATHING AND TONGUE POSITION • Nasal breathing with tongue in the roof of the mouth helps iiiensure wide dental arches and straight teeth • The tongue is one of the strongest muscles in the body, capable of exerting 500 grams of pressure. • It only takes 1.7 grams of pressure to move a tooth. • Mouth breathers carry the tongue in the floor of the mouth potentially leading to narrow dental arches, crowded teeth, receding chin, smaller jaw and risk of sleep apnoea Normal wide arches Narrow arches No room for tongue here Lateral airway views of a Mouth breather Nasal breather Note low tongue posture Note correct tongue posture CT SCANS nose breather mouth breather Mandibular advancement showing opening of airway MOUTH BREATHER Uncorrected open-mouth breathing is likely to result in: • crooked teeth • narrow dental arches • receding chin • protruding nose • narrow airway • and high risk of developing obstructive sleep apnoea by the age of thirty DENTAL DISORDERS LINKED TO OPEN MOUTH BREATHING • dental decay • malocclusion • narrowing of dental arch • dental crowding, crooked teeth • cross-bite • anterior open bite • gum disease, bad breath • inflammation of adenoids and tonsils • TMJ dysfunction www.buteykobreathing.co.nz MOUTH BREATHING AND UPPERAIRWAY DISORDERS Uncorrected open-mouth breathing can result in: • enlarged adenoids • tonsillitis • nasal polyps • sinusitis • chronic nasal congestions HYPERVENTLATION – SLEEP APNOEA - ASTHMA Average tidal volumes of 950ml and average minute volumes of 15 litres per minute during the day were recorded in males diagnosed with sleep apnoea 1 CPAP reduces hyperventilation while applied 2 Asthma improves with breathing control, through application of Continuous Positive Airways Pressure 3, 4 1 Radwan et al., Eur Resp J 1995 2 Naughton M, Benard D, Rutherford R, Am J Respir Crit Care Med 1994; 3 Pellegrino R, J Appl Physiol 111: 343-4 2011 4 Chan C, Woolcock A, Sullivan C. Am Rev Respir Dis 1989 SNORING - SLEEP APNOEA AND BRAIN HYPOXIA MRI scan red - yellow = highest oxygen dark blue = least oxygen This might also provide a clue to the higher incidence of cancer 1 and Alzheimer’s 2 in people with sleep apnoea. Dr. F. Javier Nieto 2 Osorio et al 2013 1 SNORING AND SLEEP APNOEA EXPLAINED - it’s your breathing breathing stimulated blood pH normalising O2 release to cells snoring over-breathing inflame/narrow airways vibration noise suction effect CO2 increase obstructive sleep apnoea CO2 deficit (hypocapnia) CO2 < apnoeic threshold cellular hypoxia central sleep apnoea A BRIEF HISTORY OF ASTHMA Asthma from the Greek aáζɛιν (aazein), which translates as “to breathe with open mouth or to pant”. It first appeared in Homer's Iliad and the term was probably first used in a medical sense by Hippocrates. Asthma was not considered to be associated with increased mortality until the 1930s with the advent of bronchodilator medications www.buteykobreathing.co.nz ASTHMA Genetic Factors: • stronger thicker smooth muscle lining airways 1 • five times as many mast cells as non-asthmatics 2 • more mucus producing cells lining the airways 3 Epigenetic Factors: Anything that promotes hyperventilation 1 Dail DH & Hammar SP. Pulmonary Pathology, 1988 2 Jurasek G. Respiratory Reviews V 7 No. 9 3 Lamb AB. Nunn’s Applied Respiratory Physiology, 2000 www.buteykobreathing.co.nz Hyperventilation (over-breathing) - a mechanism that is often overlooked in asthma. Average MV measured for asthmatics in Brisbane Buteyko trial - 15 litres per minute (normal 10 litres) 1 Hyperventilation whether spontaneous or exercise induced, is known to cause asthma 2, 3, 4 Loss of CO2 through hyperventilation can trigger bronchoconstriction in asthmatics 4, 5 1 Bowler S, Green A, Mitchell C, Medical Journal of Australia 1998; 169: 575-578 Demeter & Cordasco The American Journal of Medicine, (1986), vol 81 pp 989. 3 Clarke PS, Gibson, JR Aust Fam Physician. 1980 4 Sterling, GM., Clin Sci, (1968), vol 34, pp 277-285 5 van den Elshout, FJJ et al., Thorax, (1991), vol 46, pp 28-32 2 HYPERVENTLATION - HYPOCAPNIA AND ASTHMA Hyperventilation and hypocapnia (CO2 deficit) are common in asthma 1, 2, 3 Hypocapnia is the rule in asthma until respiratory failure sets in 3 1 Tobin, MJ et al. Chest, 1983; 84:287-294. Hormbrey, J. et al., European Respiratory Journal, 1988;1: 846-852. 3 Clarke, PS., Australian Family Physician. 1980; Vol 9, October 2 HYPERVENTLATION - HYPOCAPNIA - INFLAMATION Hypocapnia can trigger mast cell de-granulation and histamine release • airways – asthma, hay fever • skin – eczema • gut – food allergies, irritable bowel (IBS) Perera, J. The hazards of heavy breathing. New Scientist, Dec 1988 Kontos et al. American Jnl of physiology 1972 Coakley et al. Jnl of Leukocyte Biology 2002:71 Strider et al., Allergy 2010 www.buteykobreathing.co.nz BREATHING - BUTEYKO AND ASTHMA trigger increased hyperventilation airways cool & dry out CO2 deficit (hypocapnia) increased mucus production bronchoconstriction compensation ASTHMA www.buteykobreathing.co.nz increased exposure to irritants increased histamine inflammation BUTEYKO STUDIES FOR ASTHMA Published studies 1998 - 2012 - Reductions in asthma reliever medication of 85-100% - Reductions in inhaled steroid medication of 40-50% - Symptom reduction (improved quality of life scores) - No deterioration in lung function despite medication reduction Bowler et al., Medical Journal of Australia 1998 169 Opat et al., Journal of asthma 2000 37 McHugh, et al., New Zealand Medical Journal Dec 2003 V 116 Cooper et al., Thorax 2003 58 McHugh et al., New Zealand Medical Journal May 2006 V 119 Slader et al., Thorax 2006 61 Cowie et al., Respiratory Medicine, May 2008 V 102 Zahra et al., Egyptian Journal of Chest Diseases and Tuberculosis (2012) 61 Links to published Buteyko studies: http://www.buteykobreathing.nz/webapps/i/76035/133168/579348 www.buteykobreathing.co.nz A small clinical study of Buteyko Method shows a 70 per cent reduction in Rhinitis symptoms Adelola O.A etal Clinical Otolaryngology 2013 www.buteykobreathing.co.nz BUTEYKO BREATHING RETRAINING Who are our clients: • Asthma • Chronic nasal congestion • Allergic rhinitis • Sleep apnoea, chronic snorers • Panic attack • Dental disorders resulting from open-mouth breathing www.buteykobreathing.co.nz BUTEYKO BREATHING RETRAINING To normalise each aspect of the breathing pattern: • Rate • Rhythm • volume • Mechanics - correct use of breathing muscles • Use of the nose - inhale/exhale - For all situations: awake, asleep, at rest, when eating, speech and physical exercise Tess Graham – Relief from Snoring and Sleep Apnoea p 80 www.buteykobreathing.co.nz OVER- BREATHING -WHAT TO LOOK FOR: • • • • • • • • • • • • habitual mouth breathing audible breathing nasal congestion/ mucus upper chest breathing pattern poor posture, shoulders high, forward, slouching frequent sighing or yawning large inhalations through mouth when speaking rapid breathing rate > 15 breaths/minute paradoxical (reverse) breathing irregular breathing pattern, breath-holding cold hands and feet dry skin: face, lips, hands and feet www.buteykobreathing.co.nz THE NOSE YOUR PORTABLE AIR CONDITIONER • warms • filters • humidifies • disinfects (germicidal action of NO in paranasal sinuses 1 • nasal breathing increases arterial CO2 by 20% and O2 by 8% 2 1 Lundberg Anat Rec 2008 2 Swift et al Lancet 1988 www.buteykobreathing.co.nz NOSE UN-BLOCKING EXERCISE 1. 2. 3. Breathe in and out normally through nose Hold on the out breathe for as long as is comfortable Then gradually resume very gentle breathing It may help to pinch the nose and nod your head a few times Keep your mouth closed throughout the exercise In stubborn cases or when the blockage is due to a cold, the exercise may need to be repeated several times www.buteykobreathing.co.nz DIAPHRAGM BREATHING EXERCISE • sit with upright posture on a stable firm chair • move to the front edge of the chair, upper legs parallel with the floor, knees directly over the ankles • practise breathing gently into the belly Breathe slowly, rhythmically and gently making each breath as small as you can • Do this for 3-5 minutes a few times a day to help tone the diaphragm and reduce upper chest breathing www.buteykobreathing.co.nz Small movements HOW MUCH AIR DO YOU BREATHE? Try this test to see how much air you are breathing • Hold your index finger under your nose to feel how much air goes in and out. • When you are breathing normally you will feel warm air across your finger on the out-breath and cool air on the in-breath. • Try slowing your breathing down until you hardly feel any air across your finger. • If you have a healthy breathing pattern you should be able to maintain this sensation of no air on your finger for five minutes or more. can FEATHER BREATHING Soft invisible breathing as practised by the Samurai TWO TO FIVE BREATHING EXERCISE You can use this breathing exercise to de-stress, help overcome an anxiety/panic attack, relieve breathlessness, chest tightness or asthma and to help you sleep. This exercise can be done sitting, standing or lying down. Try to breathe gently through your nose and breathe from the belly. BREATHE WELL – SLEEP WELL Breathe well by day and you will breathe well by night • Nose breathing by day and you are more likely to nose breathe during sleep; try to sleep with mouth closed • Do some nose clearing and breathing exercises prior to sleep • Sleep with upper body slightly elevated • Avoid sleeping on back, left is best • Avoid stimulating foods, drinks and activities at least 90minutes before sleep • Turn screens off at least 60 minutes before sleeping • Sleep in a dark, well ventilated room, do not get over-heated www.buteykobreathing.co.nz Foods that adversely affect breathing and may trigger asthma, nasal congestion, snoring, poor sleep or headache • Foods containing refined white flour, sugar: refined breakfast cereals, pasta, noodles, cakes, cookies • Drinks with added sugar: soft drinks, fruit juice ... • Milk and milk products, goats milk, soy milk, protein shakes • Soft cheeses, cottage cheese, ice cream, yoghurt • Chocolate • Caffeine, alcohol • Food additives; MSG, sulphites, sodium benzoate, nitrites, aspartame Note: over-eating leads to over-breathing BREATHING AND SPEAKING Breathing tips for speaking: • Try to talk less • Talk more slowly • Breathe in through your nose at the start of each sentence • Do not take a big breath in before speaking • Breathe more gently and quietly when talking • Speak in shorter sentences BREATHING GUIDELINES FOR ASTHMA RELIEF Guidelines for reducing minute volume and normalisation of the breathing pattern • Instruct to nasal breathe if possible • Slow the breathing rate and try to reduce breathing volume • Instruct on diaphragmatic breathing • Reduce or eliminate dairy products • Reduce or eliminate refined carbohydrates especially foods and drinks with added sugar • Sleep on the left side with head elevated ASTHMA AND SPORT • Instruct to breathe through the nose, whenever possible to help maintain the natural broncho-dilating effects of CO2 in airways • • • Adjust intensity to allow comfortable nasal breathing Drop shoulders and breathe from diaphragm Slow the rate and volume of breathing during breaks in play and after physical exertion to boost cellular O2 and reduce lactic acid • Buteyko practitioners instruct not to pre-dose with reliever medication but to carry at all times and use if needed. 1 1 Any changes to prescription medication, where appropriate, are undertaken by the clients’ prescribing doctor. SIX THINGS YOU CAN DO: 1. Instruct on the importance of nasal breathing for ADL 2. To maintain nasal breathing at rest, during physical exertion, sleep 3. Correct tongue posture; with tongue in roof of the mouth 4. To supress yawns and the urge to sigh, gasp, cough, snort, sniff 5. Instruct on nasal clearance using the nose un-blocking exercise 6. Instruct on diaphragmatic breathing exercises BUTEYKO BREATHING CLINIC PROGRAM • Four consecutive 90-minute breathing retraining sessions • Two follow up sessions within six weeks • Telephone support and additional sessions if required for six weeks • Breathing exercises practised for six weeks • Life-long awareness of the concepts is recommended • course fee $605 • Ages four and up • Referral not essential * Buteyko clinic practitioners teach the Buteyko Institute Method of breathing retraining. * THE TEAM- BIBH PRACTITIONERS Glenn White Practitioner trainer Auckland Tricia Enriquez-Gault Auckland Olga Horne Auckland Susan Allen Wanaka Viv Smith Queenstown OUR TRAINEES Melody Sloggett Auckland Pia Schroeter Auckland Eddie Johnson Auckland Arisa Shioda DS Japan Ines Steward Auckland Dina Ceniza Auckland Our practitioners teach to Buteyko Institute of Breathing and Health (BIBH) standards. The BIBH is ISO 9001:2008 Certified BUTEYKO BREATHING CLINICS For information about the Buteyko breathing retraining programme: • • • • Consultations Introductory seminars Courses Workshops for health professionals Tel: 09-360 6291 info@buteykobreathing.co.nz www.buteykobreathing.co.nz SNORING – SLEEP APNOEA - ASTHMA CROOKED TEETH ... WHAT’S THE LINK? REFERENCES Abnormal facial development linked to mouth breathing http://www.buteykobreathing.nz/webapps/i/76035/133168/579346 Asthma stress and hyperventilation http://www.buteykobreathing.nz/uploads/76035/files/Asthma_stress_and_hyperventilation.pdf Supporting evidence for the use of breathing training for asthma http://www.buteykobreathing.nz/webapps/i/76035/133168/579348 Glenn White BSc MSc MBIBH BIBH Practitioner/trainer www.buteykobreathing.co.nz