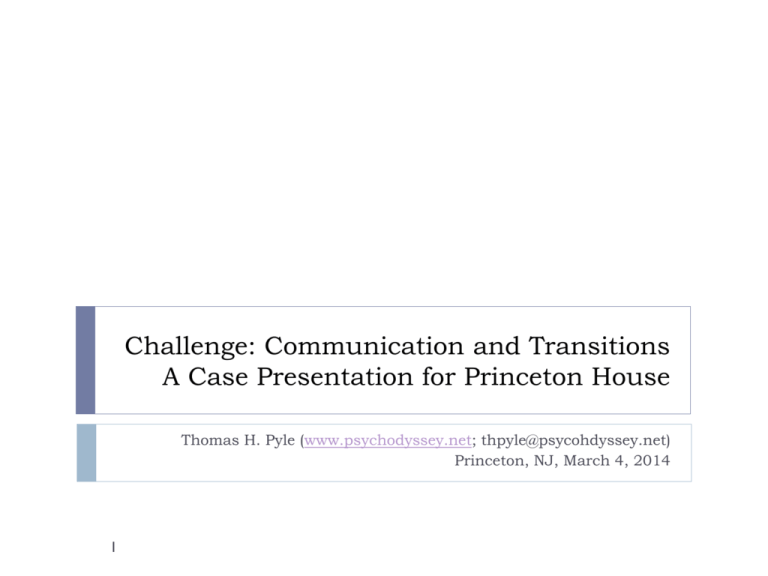
Challenge: Communication and Transitions
A Case Presentation for Princeton House
Thomas H. Pyle (www.psychodyssey.net; thpyle@psycohdyssey.net)
Princeton, NJ, March 4, 2014
1
On my...
...heart
Appreciation
Gratitude
Desire
Hope
2
...mind
Communication
Transitions
Collaboration
“Value”
What’s ahead...
Recovery: the process
Communications & Transitions
4 ideas
3
Who am I?
20 years in banking
10 years in non-profit
In Princeton since 1971
Son of a doctor
Father to a son
7 years navigating the maelstrom
Helper of other families (see: www.psychodyssey.net)
A “lived-experience expert”
4
...schizophrenia
... New Jersey’s mental health system
... Behavioral health treatment centers and programs
More about me...
MBA (Harvard), MS PsyR (UMDNJ), CPRP
PhD candidate, Health Sciences (PsyR)
New Jersey Mental Health Planning Council
Foundation for Excellence in Mental Health Care
Collaborative Support Programs on New Jersey
Consumer Providers Association of New Jersey
NAMI Mercer
Adjunct professor, Rutgers Dept. Psych Rehab
5
The Family
6
The Family
1920 - 2002
Medical Director, Princeton University
1977-1992
7
The Principal
DOB: 8/24/85
Princeton High School
Rutgers, Pratt
Reasonable health
But: asthma; smoker
Since 3/07: 295.30 (DSM IV)
Also: 296.xx, 295.70
GAF: 20 – 50 (in hospitals)
Other factors
8
Something Different: Orthomolecular...
Linus Pauling
9
Abram Hoffer
“The System”: Aspects of Need
Financial
Functional
Legal
Medical
Residential
Psychiatric
Occupational
Spiritual
Educational
Emotional
Political
Social
Mobile
Recreational
Cultural
©T.H. Pyle, 2009. All Rights Reserved.
NJ DeptHumServ
DDS
DMHS
County
DDD
DMAHS DFD
State
NJ DeptState
NJ StCounArtsNJ COAH
NJ DBI
DeptInsur
NJ DOT
NJ Trans
NJ Treas
DivTax
BdSocServices
Disability
Subsidy
US DOL
NJ CasRevFund
NJ DCA
DivHous
Federal ETA
NJ HMFA
SpNdTrFd
NJ DLWD
DVRS
UnivServ
Fund
SocSecAdm US HHS
Medicare
(in 2 yrs)
NJ Medicaid
PAAD
Private Programs
AAMH
GTBH
SERV
CathChrties
Ptn Hse
CathChrties
Plan NJ
SRAP
Banks
Personal
Credit
PrivatePay
Addictions
Living Skills
Social Skills
Carrier
Ptn Hse
Brighter Day
MassGeneral
Beck Inst
Food Stamps
SSD/SSI
PropTax
Rebate
Functional
Guardianship
Private Firms
Advance Directive
Rights
Legal
Police
Inpatient
Doctor
Medication
Medical
Supportive
Residential
Public
HomeOwner
Counseling
Psychiatrist
PACT
Psychiatric
DisAbRtsNJ
ComHealLaw
Legal Aid
Trust Protector
Special Needs
Trust
Financial
Food
Outpatient
Income
Tax
Credits
“S8”
Voucher
CommEntrCorp
IndDev
Acct
HUD (via
US Treas
local PHA) IRS
RIST
Occupational
Sect. 8,
202, 811
Affordable
PrivateAgencies
Therapist
CDC
SERV
Triple C
Cath
Chrties
Towns
Community
Groups
Ticket to Work
Spiritual
Divine Providence
Educational
Emotional
IFSS
NAMI Fam2Fam
TCNJ
Parents
Siblings
Relatives
Clubhouses
Drop-in Centers
Laurel House Support Grps
Life Coaching
NAMI Just Friends
CollSuppProg
Political
Social
Recreational
Mobile
Cultural
Personal
Public
Car
Transport Medical
Transport
“Dollar A Day”
AccessLink
NJ Transit
Stouts
RideShare
Coach
Advocacy
NAMI
Mental Health
Assn NJ
Hobbies
Vacations
Travel
Tutor
Exercise
Equipment
ArtsUnbound
VSA
CulturalAcess
Network
PASS “Cadre”
PASS
CerebPalsyNJ
DVRS; Private
EpilepFound
Contractors
DisabProg
WIPA / NJ WINS
“Navigator”
VoTech
NJ WorkAbility
“One-Stop”
CommColl
Career Centers
MCCC
MCTech
Life
©T.H. Pyle, 2009. All Rights Reserved.
Recovery Goal...
Premorbid “normality”?... Symptom remission?...
Off medications?... Reformulated self-concept?...
Community Integration.
(to live, love, learn, work...
...as, where, and how one chooses)
12
...based on Recovery Principles
(Substance Abuse and Mental Health Services Administration, 2004)
13
Recovery: To Most, An Outcome
time
14
Recovery: Actually, A Process
time
15
Medical
Recovery Process: 3 Components
Medical
Psychiatric Rehabilitation
Individual Empowerment
time
16
Recovery: Empowerment Component
Psychotherapy
Peer Groups & Services
Individual Empowerment
time
17
Recovery: Medical Component
Medical
Hospitals
Doctors
Medical
Psychiatric Rehabilitation
Meds
Individual Empowerment
time
18
Recovery: Rehabilitation Component
Illness Management & Recovery
Medical
Supported Housing
Supported Education
Medical
Psychiatric Rehabilitation
Supported Employment
Assertive Community Treatment
Family Psychoeducation
Individual Empowerment
time
19
Psych Rehab: Evidence-Based Practices
(Pratt, Gill, Barrett, & Roberts, 2007)
Illness Management and Recovery
Integrated Dual Disorder Treatment
Assertive Community Treatment
Family Psychoeducation
Supported Employment
Supported Education
Supported Housing
“Promising” practices
20
So... A Whole Recovery System
Illness Management & Recovery
Supported Housing
Medical
Hospitals
Supported Education
Doctors
Medical
Meds
Psychiatric Rehabilitation
Supported Employment
Assertive Community Treatment
Family Psychoeducation
Psychotherapy
Peer Groups & Services
Individual Empowerment
time
21
Recovery Process: 3 Essential Sciences
Medical
Psychiatric
Psychiatry
Rehabilitation
Psychiatric Rehabilitation
Medical
Psychology
Individual Empowerment
time
22
The Common Misperception of Relativity
23
Tx Planning: The VA’s Framework
Source: Department of Veteran Affairs
Intensity
Level 5
Hospital Setting
(Highly Staffed)
Level 4
Professional Care Setting
(Moderately Staffed)
Level 3
Residential (Treatment)
Setting
Level 2
Partial Hospitalization
(Day Program)
Level 1
Community
(Outpatient)
Very High
RN supervision
Locked unit
Severe symptoms
Specially trained staff
Skilled nursing care, RN
supervision
Supervision w/ specially
trained staff
Highly structured milieu
Symptom reduction
Community re-entry goals
24 hr professional or
paraprofessional
supervision
Highly structured milieu
Intensive case
management
Rehab planning w/ specific
functional goals
15+ hrs/week
Structured groups,
activities all week
and/or weekends
Time limited to stabilize
Crisis management
15+ hrs/week
Crisis management,
stabilization
Intensive case
management
High
RN supervision
Treat. plans w/ goals
Major symptoms
Skilled nursing care, RN
supervision
Treat. plan w/ goals
Highly structured milieu
Community re-entry goal
Symptom stabilization
24 hr onsite supervision
Highly structured daily
milieu
Active case management
Specific rehab goals
9-15 hrs/week
Structured groups or
activities
Ongoing to prevent
hospitalization
9-15 hrs/week or more for
work programs
Intensive case
management
Moderate
RN supervision
Treat. plan w/ goals
Brief respite, med
stabilization
Crisis stabilization
Nursing care, RN
supervision
Moderately structured
milieu
Plan highest functional
level
Secured setting
Rehabilitation focus
24 hr supervision
Moderately structured
milieu
Basic care management
2-8 hrs/wk
Supportive activities w/
case management
1-8 hrs/week or more for
work programs
Basic care management
Psychotherapy
Routine clinical care
Low
Diagnosis or evaluation
Procedures needing high
staffing
Maintenance of self-care
LPN supervision
Partially structured milieu
Emphasis on rehab for
group or independent
living
Non-professional
supervision
No clinical services
No formal structure
Clinical oversight: monthly
24
---
< 1 hr/week
No case management
beyond primary care
Periodic medication
reviews
An Optimal Tx Plan?
Intensity
Level 5
Hospital Setting
(Highly Staffed)
Level 4
Professional Care Setting
(Moderately Staffed)
Level 3
Residential (Treatment)
Setting
Level 2
Partial Hospitalization
(Day Program)
Level 1
Community
(Outpatient)
Very High
High
Moderate
1.
Hospital
2.
Treatment
Residential
3.
Need
Supported
(IDDT)
Residential
4.
Independent
4. IOP
Residential
Low
25
Recent Experience: Tx vs. Need
Intensity
Level 5
Hospital Setting
(Highly Staffed)
Level 4
Professional Care Setting
(Moderately Staffed)
Level 3
Residential (Treatment)
Setting
Level 2
Partial Hospitalization
(Day Program)
Level 1
Community
(Outpatient)
Very High
Hospital
Hospital
High
Gap
(IDDT)
Moderate
Low
Current
Tx
26
Recent Experience: Tx vs. Need
Intensity
Level 5
Hospital Setting
(Highly Staffed)
Level 4
Professional Care Setting
(Moderately Staffed)
Level 3
Residential (Treatment)
Setting
Level 2
Partial Hospitalization
(Day Program)
Level 1
Community
(Outpatient)
Very High
Hospital
High
Moderate
State
Hospital
Clinical
Residential
Therapeutic
Communities
Gap
(IDDT) Group
Homes
Need
Local
Supported PHP
(IDDT)
Housing
Low
Local
IOP
PACT
4.
Independent
4.Current
IOP
Residential
Tx
27
Tx vs. Need: Options
Intensity
Level 5
Hospital Setting
(Highly Staffed)
Level 4
Professional Care Setting
(Moderately Staffed)
Level 3
Residential (Treatment)
Setting
Level 2
Partial Hospitalization
(Day Program)
Level 1
Community
(Outpatient)
Very High
Hospital
Hospital
High
Moderate
TPH
WestBridge
LaPaloma
Spring Lake
Gap
Ranch
CooperRiis
SERV Group
(IDDT)
EarthHouseHome
PACT
Local
IOP
Low
28
Own
4. IOP
Apartment
But Private Resources are Costly…
WestBridge
CooperRiis
Gould Farm
Spring Lake Ranch
Spirit of Gheel
Type
IDDT Specific
Residential treatment
Residential therapeutic
community
Residential therapeutic
community
“Alternative” residential
therapeutic community
Residential therapeutic
community
Location
Manchester, NH
Asheville, NC
Montgomery, MA
Shrewsbury, VT.
Spring City, PA
Handle Dual?
Yes. Specifically those
with SZ and addiction.
Yes, after stabilization
Yes, well after
stabilization
Yes.
Don’t know.
Style
Voluntary.
Open. Voluntary.
Open. Voluntary.
Open. Voluntary.
Open. Voluntary.
Tenor
4-6 months.
Farm: 6-9 months
Farm: 6 months to life.
6 months.
Step down: 6+ months.
Step Down: 6+ months
First month: $32,000
$14,500 per month.
Scholarships possible
after Month 2.
$295 per day, = ~$9000
per month
$285 per day = $8550
per month.
$235 per day = ~$8000
per month.
Work therapy. Workordered day (5 hours).
Don’t know.
Yes.
Don’t know.
Cost
Thereafter: $20,750 per
month.
Modality distinction
Group therapy.
“Enhanced Recovery
Model”: meet person
where he is.
Work with legal
system?
Yes.
Yes. Probations can be
transferred to Polk
County. Also happy to
prepare reports, etc.
29
Not sure. Didn’t ask. I
think not.
Communications & Transitions
Specific disconnects
30
...having in mind...
31
2007: 1st inpatient discharge...
March 30, 2007, 9:30 pm: the earthquake
March 31, 2008, 4:00 am: Dr. Schofield’s news
Carrier: 10 days in zombie land
Discharged too early to Princeton House outpx
Admitting reaction: “He’s not appropriate for outpx”
Transferred to Princeton House inpatient
Back to outpatient, etc.
32
2007: Dear ______,
33
2008: Hospital doctor’s alarming Rx...
“Dad, I think I have a problem...”
Cannabis + amphetamine
Tx plan: wilderness therapy in UT WestBridge in NH
Adderall Rx (50 mg) from a local Princeton doctor...
Abilify (~2 mg?)
Success: off cannabis, off amphetamine
Manchester, NH
34
Ideation ER Psych Ward. No communication?
Psychiatrist prescribes... 50 mg Adderall!
Back at WestBridge: no change...
Manic episode, outburst, termination
Cost to family (UT + NH programs): ~$50,000
2011: Premature release from ER
Prior
2 PH ER intox admissions in previous week
Known history of 295.30
Near death intoxication
35
~12 pm:
2 pm:
2 pm:
4 pm:
11 pm:
4 am:
2 pints vodka
Collapsed. No response. Dilated pupils.
Call to 911. Goal: inpatient admission
BAC = .38
LSW: no psych eval till BAC < .08 ~@ 6 am
Released, with BAC still ~2x limit
2011: Involuntary No. 1
Previous week
Florid symptoms (sertraline: 200 mg; risperidal < 2 mg...)
Intoxication
Prospect Street: “Welcome back Muslims Students!”
Response: hate crime felony charge
Fear: jail?
Then
36
Continuing symptoms, risks.
Father calls Crisis. Goal: inpatient hospitalization
The “horsewhisperer”
But, after 72 hours? Discharge. No tx plan.
2011: Involuntary No. 2
Another ER episode
Doctors call Crisis. Crisis refuses.
Doctors go alternative route. Judge and parents support.
Transfer to Hampton House.
Finally, a sustained inpatient period...
37
Progress for 18 days.
Then, a judge reverses. No consultation.
Hampton discharges to Mercer PACT.
No Mercer PACT! 11 days: no services.
Father arranges PH engagement.
2012: Involuntary No. 3
Morning:
Voluntary admission to PH inpatient
Difficulty with meds
Dr. Kazi asks family’s help to negotiate
Deal: depot dose for extension of voluntary
Agreement!
4 hours later
38
Overridden! No notice. Involuntary invoked.
150 mgs Thorazine injected. Anti-depressants stripped.
2 weeks later: parents support extension of involuntary
2012: State Hospitalization
Involuntary No. 3
Wednesday before Thanksgiving...
> 20 days...
Making progress, with lithium. Good reports all around
Tuesday before Thanksgiving: ordered to TPH
At PH discharge:
At TPH 1 hour later:
SZA, GAF 20
BP I, GAF 35
5 days before first team meeting (normally 48 hrs)
39
Admitting psychiatrist: “Why is he here?”
2013: Involuntary No. 4 (almost)
Struggling with self-medication
On his own, discusses with outpatient psychiatrist
Agree to voluntary inpatient admission
Process begins. Arrives in AM. Releases signed.
PM: Where is he?
In the ER
Inpx doctors initiate involuntary commitment.
40
Outpx doctor has no idea
In Middlesex, not Mercer to Perth Amboy?
Releases not signed. Staff reluctant to inform father.
Next day, 11 am: Involuntary called off. Admitted inpatient.
2011: One person’s care experience...
In a 10Police
month
period in 2011...
encounters
Arrests
Calls to Crisis Center
Hospitalizations
Outpatient programs
Court appearances
Prescribing psychiatrists/APNs
Diagnoses
Meds changes
Outside Therapists
Group sessions
Institutional case managers
Ambulance rides
41
5
1
3
10
3
1
14
3
over 10
2
Innumerable
12
6
Issues...
Transitions
42
Issues...
Communication
43
Psychiatrists as they see themselves?...
44
The Family Burden...
45
References
Citations...
46
Cadigan, K., & Murray, L. (2009). When medicine got it wrong [Documentary Film]: imageReal
Pictures, KQED & the Independent Television Service (TVS), with funding by the
Corporation for Public Broadcasting.
Chambers, M., Ryan, A. A., & Connor, S. L. (2001). Exploring the emotional support needs and
coping strategies of family carers. Journal of Psychiatric and Mental Health Nursing,
8(2), 99-106. doi: 10.1046/j.1365-2850.2001.00360.x
Dixon, L., McFarlane, W. R., Lefley, H., Lucksted, A., Cohen, M., Falloon, I., . . . Sondheimer,
D. (2001). Evidence-Based Practices for Services to Families of People With Psychiatric
Disabilities. Psychiatric Services, 52(7), 903-910. doi: 10.1176/appi.ps.52.7.903
Doornbos, M. M. (2001). The 24-7-52 job: Family caregiving for young adults with serious and
persistent mental illness. Journal of Family Nursing, 7(4), 328-344. doi:
10.1177/107484070100700402
Doornbos, M. M. (2002a). Family caregivers and the mental health care system: Reality and
dreams. Archives of Psychiatric Nursing, 16(1), 39-46. doi: 10.1053/apnu.2002.30541
Doornbos, M. M. (2002b). Predicting family health in families of young adults with severe
mental illness. Journal of Family Nursing, 8(3), 241-263. doi:
10.1177/10740702008003006
Hatfield, A., & Lefley, H. (2005). Future Involvement of Siblings in the Lives of Persons with
Mental Illness. Community Mental Health Journal, 41(3), 327-338. doi: 10.1007/s10597005-5005-y
Kass, M. J., Lee, S., & Peitzman, C. (2003). Barriers to collaboration between mental health
professionals and families in the care of persons with serious mental illness. Issues in
Mental Health Nursing, 24, 741-756.
Laidlaw, T. M., Coverdale, J. H., Falloon, I. R. H., & Kydd, R. R. (2002). Caregivers' stresses
when living together or apart from patients with chronic schizophrenia. Community
Mental Health Journal, 38(4), 303-310.
Lefley, H. (1989). Family burden and family stigma in major mental illness. American
Psychologist, 44(3), 556-560.
Lefley, H. (1996). Family caregiving in mental illness. Thousand Oaks, CA: Sage.
Lefley, H. P. (1998). Families coping with mental illness: The cultural context. Ann Arbor, MI:
Jossey-Bass, Inc.
Lefley, H. P. (2001). Helping families of criminal offenders with mental illness Forensic mental
health: Working with offenders with mental illness (pp. 40-13). Kingston, NJ, US: Civic
Research Institute.
Lefley, H. P. (2005). From family trauma to family support system Understanding and treating
borderline personality disorder: A guide for professionals and families (pp. 131-150).
Arlington, VA, US: American Psychiatric Publishing, Inc.
Lefley, H. P. (2009a). Family psychoeducation for serious mental illness. New York: Oxford
University Press.
Lefley, H. P. (2009b). Family psychoeducation for serious mental illness. New York: Oxford
University Press.
From... The Family Role in Rehabilitation
47
See full course syllabus at http://www.psychodyssey.net/?page_id=4332
The real problem?...
Medications efficacy... 2-4 weeks
Inpatient stays...
48
5-7 days
The real problem?...
Brain vs. mind?
49
DSM III (1980)...
Recommendations
Transitions
A “halfway” intercept?
Communications
Peer-run emergency respite?
Help in training
A true IDDT therapeutic
residential tx?
50
At Hagedorn site?
Partner with Dartmouth?
Private/public?
Family PsyR Institute
Partners: NAMI NJ, Rutgers
PsyR Dept.?
An advisory council
Consumers
Families
PsyR practitioners