Chemistry PPT Flashcards Unit 2
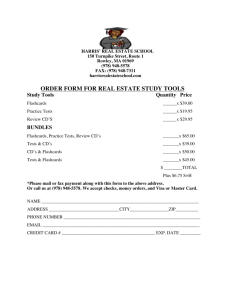
advertisement

Chem PPT Flashcards Unit 2 Mass spectrometry is: A mass spectrometer is: A mass spectrometer consists of the following five elements: A vacuum system is used to prevent collision of ions during interaction with: It requires the use of a vacuum from 10-3 to 109 torr one of two sources: Class of spectrometer where the ions make one trip through the instrument and then strike the detector, where they are destructively detected is 3 types of the above: Trapping mass spectrometers: What does MS/MS stand for? What is also called MS/MS? What is characterized by a highly selective detection technique used for quantitative analyses, characterization and compound identification? What does GC-MS stand for? What is used by the NIST as a definitive method of qualifying standard reference materials and assigning certified values to many clinical analytes? What is used as confirmatory tests for drug testing presumptively found to be positive by immunochemical analyses? What does LC-MS stand for? What is used for analysis of polar and non polar analytes and large molecular weight compounds? What is used in screening and confirmation of genetic disorders and inborn errors of metabolism? The study of matter through the formation of gas phase ions that are characterized using mass spectrometers by their mass, charge, structure, and/or physico-chemical properties An analytical instrument that first ionizes a target molecule and then separates and measures the mass-to-charge (m/z) ratio of these molecules or their fragments Ion souce, vacuum system, mass analyzer, detector, computer Magnetic or electrical fields Mechanical vacuum or efficient high vacuum pump Beam type Quadrupole mass spectrometer, magnetic sensor mass spectrometer, time of flight mass spectrometer Are based on the trapping of ions to capture and hold ions for an extended time in a small region of space Mass spectrometry/mass spectrometry Tandem mass spectrometry Tandem mass spectrometry Gas chromatography mass spectrometry GC-MS GC-MS Liquid chromatography mass spectrometry LC-MS LC-MS 1 Chem PPT Flashcards Unit 2 Matrix-assisted laser desorption/ionization – Time-of-flight mass spectrometry What is MALDI-TOF-MS used for? For the detection of specific compounds, identification of proteins, or identification of an organism What are proteins with catalytic properties? Enzymes What are protein catalysts of biological origin? Enzymes What is a substance that modifies and increases Catalyst the rate of a chemical reaction without being permanently changed or consumed? How are individual enzymes identified? By using the name of the substrate or group upon which they act and then adding the suffix -ase. The type of reaction involved is identified TRUE when naming enzymes. What are the different structures of proteins? Primary, secondary, tertiary, quaternary Biological activity is affected by denaturization Elevated temperatures, extremes of pH, due to what factors? changes in ionic strength, and chemical addition What is one of a group of enzymes catalyzing Isoenzyme the same reaction by different molecular structures and characterized by varying physical, biochemical, and immunologic properties? What is a substance that modifies and increases A catalyst the rate of a particular chemical reaction without being consumed or permanently altered? What are protein catalyst of biological origin? Enzymes What can enzymes convert? Enzymes can convert substrate molecules that can be used for the measurement of their activity What defined as the quantity of enzyme that International unit (IU) catalyzes the reaction of 1 µmol of substrate per minute? What is the International System of Units (SI)- Katal unit (KU) derived unit for catalytic activity? What unit defined moles converted per second? Katal unit (KU) How enzyme concentration governs the rate of The rate of reaction is generally proportional to Enzyme-Catalyzed Reactions? the amount of enzyme present in the system and is the basis for the quantitative determination of enzymes by measurement of reaction rates. What is substrate concentration? A reactant in an enzyme-catalyzed reaction that binds to the active center of an enzyme. What does MALDI-TOF-MS stand for? 2 Chem PPT Flashcards Unit 2 What is first order kinetics? What is zero-order kinetics? What is a constant for a given enzyme acting under given conditions; the experimentally determined substrate concentration at which the enzymatic reaction velocity equals ½ of the maximum velocity of the enzymatic reaction? What is a plot of the reciprocal of the velocity of an enzyme catalyzed reaction (ordinate; yaxis) against the reciprocal of the substrate concentration (abscissa; x-axis)? What shows maximum activity in vitro in the pH range of enzymes in plasma? What are the activity values observed in pH as low and high? What can be controlled by the use of buffer solutions? When does enzymes inactivation and denaturation occurs? What is the accepted measuring temperature for enzymes in the clinical laboratory? What is a substance that reduces the rate of an enzymatic reaction and is classified as reversible or irreversible? What is a structural analog of the substrate that combines with the free enzyme and competes with the normal substrate for binding at the active site? What is structurally different from the substrate, it binds at a site on the enzyme molecule that is different from the substratebinding site? in an enzymatic reaction, as more substrate is consumed, the reaction rate declines and becomes dependent on substrate concentration; this is a phrase of first-order dependence on substrate concentration when the rate of the reaction is proportional to the concentration of substrate or when the enzyme concentration is fixed and the substrate concentration is varied. In an enzymatic reaction, when the reaction rate is constant at maximum value, the reaction rate depends only on enzyme concentration and is independent of substrate concentration; the rate of reaction is proportional to the zero power of the substrate concentration. Michaelis-Menten constant (Km) Lineweaver-Burk plot pH range from 7 to 8 Low as 1.5 (pepsin) High as 10.5 (ALP) Pronounced effects of pH on enzyme reactions. Occurs at temperature of 60 degrees Celsius to 70 degrees Celsius. 37 degrees Celsius Inhibitor Competitive inhibitor Noncompetitive inhibitor 3 Chem PPT Flashcards Unit 2 What is the small molecule or ion that increases the rate of an enzyme-catalyzed reaction by promoting formation of the most active state of the enzyme or of other reactants such as the substrate? When used as analytical reagents for measuring metabolites, they increase the specificity of the substance being determined What is a Coenzyme NAD and NADH are examples of? What is a Prosthetic group What is a poenzyme H What is a oloenzyme The rate of an enzyme catalyzed-reaction is directly proportional to the amount of _____ present in the system Fixed-time and continuous-monitoring methods are used to measure ______. Progress of an enzyme reaction is monitored by measuring in time the decreasing concentration of the ______ or the increasing concentration of the _____. The amount of substrate transformed into products during an enzyme-catalyzed reaction can be measured by? Immunoassays are used to measure ______instead of _______. What assay is capable of identifying all molecules with the antigenic determinants necessary for recognition by the antibody and has been found to be significant in the determination of some digestive enzymes, such as trypsin, when inactive precursors and inhibitors of catalytic activity are present in plasma When enzymes are used as analytical reagents for the measurement of metabolites there is a great increase of _____ for the substance being determined. Activator Enzymes A small molecule (some contain structures derived from vitamins) that is required for some enzyme-catalyzed reactions to occur; is temporarily or permanently bound to the enzyme Coenzymes a tightly bound, non-peptide structure required for the activity of an enzyme The protein component of an enzyme An active enzyme formed by combination of a coenzyme and an apoenzyme active enzyme reaction rates substrate, product Spectrophotometry Fluorometry Chemiluminescence protein mass, catalytic activity Immunoassay Specificity 4 Chem PPT Flashcards Unit 2 Enzymatic methods that allow all substrate Equilibrium methods present in a reaction mixture to be completely converted into a measurable product before measurement, are referred to as Enzymatic methods which demonstrate that the Kinetic Methods change in substrate concentration over a fixed time interval is directly proportional to its initial concentration What is an immunoassay? An assay based on the reaction of an antigen with an antibody specific for the reaction. What is antigen? 1) Any material capable of reacting with an antibody without necessarily being capable of inducing antibody formation. 2) Analyte being detected by the immunoassay. What are antibodies? An immunoglobulin (Ig) class of molecule (IgA, IgG, IgM) that bins specifically to an antigen or hapten Which immunoglobulin is the most widely Immunoglobulin G (IgG) used reagent? What is an Immunogen? A protein of a substance coupled to a carrier cable of introducing an immune response. What is a hapten? A chemically defined determinant that by itself will not stimulate an immune response. It is an incomplete antigen What is affinity? 1) It refers to the thermodynamic quantity defining the energy of interaction of a single antibody-combining site and its corresponding epitope on the antigen. 2) It is a property of the substance bound (antigen) What is avidity? 1) Refers to the overall strength of the binding of antibody and antigen and includes the sum of the binding affinities of all individual combining sites on the antibody. It is a property of the binder (antibody) What are factors affecting antigen-antibody 1) Binding forces binding? 2) Reaction mechanism 3) Precipitin reaction 4) Chemical factors: 1)Ion species and ionic strength effects 2) Polymer effect 5 Chem PPT Flashcards Unit 2 In the binding forces, what are 3 major contributing forces? 1) Electrostatic van der Waals-London dipole-dipole interactions 2) Hydrophobic interactions 3) Ionic coulombic bonding 1) Phase 1:Initial reaction of a multivalent antigen and a bivalent anitbody 2) Phase 2: Subsequent growth of the complexes 3) Phase 3: Precipitation of the complex before after a critical size is reached. In the reaction mechanism, what are the 3 phases? These soluble complexes have all antigenic sites that are covered with antibody, and lattice formation is inhibited. This insoluble complexes (optimal proportion) state occurs when 2 to 3 antibody molecules are present for each antigen molecule; produces maximum lattice formation and therefore maximum precipitate. These soluble complexes have all antigenic sites that are saturated by antigen. Triplets (2 antigen + 1 antibody) are maximum size attained by particles. no precipitate is formed. Anion and cationic salts can affect the binding of antibodies by what 2 chemical factors? What are 3 examples of polymer effect in terms of having high molecular weight, high degree of linearity and aqueous solubility that can significantly increase the rate of immune complex growth and enhances precipitation of immune complex? What are 2 types of qualitative methods regarding passive gel diffusion that use semisolid medium (e.g., agar agarose), and that the initial concentration of antigen and antibody are critical? The term for an analytical technique that combines separations of antigens by electrophoresis with immunodiffusion against an antiserum? Also known as two-dimensional immunoelectrophoresis, what is the term describing to drive the antigen into a gel containing antibodies specific for the antigens of interest. This technique involves an electrophoresis step, followed by transfer of the separated proteins onto on overlying strip of nitrocellulose or nylon membrane by a process called? This electrophoresis step involves DNA blotting onto a membrane. This electrophoresis step involves RNA blotting onto a membrane. Antibody Excess Equivalence Zone Antigen Excess 1. 2. 1. 2. 3. Ion species Strength effects Dextran Polyvinyl alcohol polyethylene glycol Raidal immunodifussion (RID) (single immunodiffusion) and Ouchterlony technique (double diffusion) Immunoelectrophersis (IEP) Crossed immunoelectrophoresis Electro-blotting. Western/Southern blotting Northern RNA 6 Chem PPT Flashcards Unit 2 What does RID stand for? What is the definition for RID? Radial Immunodiffusion A passive diffusion method which a concentration gradient is used for a single reactant During RID, what happens when antibody is A well defined ring of precipitation around the added? well indicates presence of antigen What is also known as the “rocket” technique? Electroimmunoassay What is the definition of electroimmunoassay? A type of immunoassay where a single concentration gradient is established for the antigen and an applied voltage is used to drive the antigen from the application well into a homogenous suspension of antibody in the gel Turbidimetric and Nephelometric assays are The rate of formation of immune complexes in convenient techniques to measure what? vitro using their light scattering abilities What are some examples of radioactive and Competitive, Noncompetitive, and non-isotopic labels? heterogeneous immunoassays What is a Heterogeneous immunoassay? Immunochemical assay that require separation from the bound label What does RIA stand for? Radioimmunoassay Define RIA Used radioactive isotopes of iodine, 125I and 131I and tritium (3H) as labels What does EIA stand for? Enzyme Immunoassay What does ALP stand for? Alkaline phosphatase What does HRP stand for? Horseradish peroxidase Give some examples of enzymes that are used ALP, HRP, Glucose-6-dehydrogenase, Bin EIA? galactosidase What are 3 Examples of Enzyme Immunoassay Enzyme-Linked Immunosorbent Assay (EIA)? (ELISA) Enzyme Multiplied Immunoassay Technique (EMIT) Clone Enzyme Donor Immunoassay (CEDIA) What does Fluoroimmunoassay (FIA) use? Uses a fluorescent molecule What is fluorescent used as in FIA? as an indicator label to detect and quantify immunological reactions What is Chemiluminescent immunoassay? a chemiluminescent molecule, such as acridinium What is Chemiluminescent immunoassay used is used as an indicator label to detect and for? quantify immunological reaction What is Electrochemiluminescent an elecrochemiluminescent molecule, such as immunoassay? ruthenium What is electrochemiluminescent is used as an indicator label to detect and immunoassay used for? quantify immunological reaction What is one definition of automation? The process whereby an analytical instrument performs many tests with only minimal involvement of an analyst 7 Chem PPT Flashcards Unit 2 What is another definition of automation? What is Random-access analysis? What is Continuous-flow analysis? What is Single-channel analysis? What is Multiple-channel analysis? What is multiple-channel analysis similar to? What is Parallel analysis? What is Discrete analysis? How many types of the specimen identifiers? What are the technologies used for automatic identification and data collection? What are the delays in preparation of specimen? What are the methods of delivery specimen? How reliable is a courier service? How does pneumatic tube system transport? controlled operation of an apparatus, process, or system by mechanical or electronic devices without human intervention analyses are performed on a collection of specimens sequentially and each specimen is analyzed for a different selection of tests. it specimen in a batch passes through the same continuous stream at the same rate and is subjected to the same analytical reactions each specimen is subjected to a single process so that only results for a single analyte are produced. each specimen is subjected to multiple analytical processes so that a set of test results is obtained on a single specimen. Similar to random access analysis all specimens are subjected to a series of analytical processes at the same time and in a parallel fashion the sample is aspirated into the sample probe and then is delivered, often with reagent, through the same orifice into a reaction cup or another container. These are: specimen labels, serial number, part number, manufacturer, and assigned patient number There are technologies used for automatic identification and data collection as barcoding, optical character recognition, magnetic stripe and magnetic ink character recognition, voice identification, radiofrequency identification touchscreen, light pen, handprint tablets, optical mark reader, smartcards. -Clotting of blood in specimen collection tubes -Subsequent centrifugation -Preparation of serum and plasma -Transfer of serum the secondary tubes Courier service, pneumatic tube systems, electric track vehicles, and mobile robots. Courier service is usually reliable but costly and may require batches, but risk of specimen breakage or loss Pneumatic tube systems provides rapid specimen transportation, risk of misrouting or hemolysis 8 Chem PPT Flashcards Unit 2 How does specimen delivery as an electric track vehicle? How does specimen delivery as a mobile robot? Once collected into a red top tube what is the first thing one must do before specimen preparation for routine tests can begin? Once a red top tube is allowed to clot what is the next step in specimen preparation for routine testing? Once a red top tube has been allowed to clot and centrifuged until separated what is the next step in preparing the specimen for routine testing? What are two common ways to get specimens from site of collection to the lab? What are the pros and cons of currier service. What are the pros and cons of the pneumatic tube system? What is an electric track vehicle? Larger capacity than pneumatic tube systems makes use of dry ice or refrigerator packs possible Easily adapted and programmable, but need for batching and personnel to load robots. Red top tubes have no anticoagulant and therefore must be allowed to clot before preparing them for routine tests. Centrifuge the specimen for at 1200g for 10 minutes then separate serum from the cells, labeling the secondary tube appropriately. Currier service and Pneumatic tube system Pros•Reliable •best way to get specimens to the lab if from a site across cities or even states. Cons•costly •require multiple specimen batch collections and deliveries throughout the day •risk of specimen breakage •risk of specimens becoming too warm or cold if left outside in collection box. Pros•Rapid specimen transport Cons•Risk of specimens being sent to the wrong place and becoming lost •tube traffic may occur causing tubes to collide possibly shutting the system down -this could cause hemolysis or leaking specimens A form of specimen delivery similar to the pneumatic tube system in which specimens are carried on a track, not within a tube system, and in a specimen carrier box which can be larger and more versatile in the type of specimen being transported. Also can utilize ice packs or dry ice to keep specimens under the correct temperature conditions. 9 Chem PPT Flashcards Unit 2 Mobile robots are being utilized for what laboratory service? Having instrumentation that is capable of sampling directly from a primary tube or centrifuging and aliquoting the plasma or serum into a secondary tube on its own will reduce what and increase what? Three processes of removing protein and other interferents are? In immunochemistry, instrumentation is capable of separating bound and free fractions via which methods? Define carryover in regards to specimen transport during analytical testing What sample introduction system utilizes a peristaltic pump? What sample introduction system utilizes pipets and is highly automated. Instrumentation must have what capability to store reagents? Instrumentation must have this to identify patients and tests to be performed on each sample. Rate of transport of reaction mixture through the system to the measurement station affects what? on-time events on reagent addition (or activation) relative to measurement will affect what? What are the five main means of mixing reactants in instrumentation? Some temperature control and efficient heat transfer methods seen in instrumentation are… Mobile robots are being used for specimen transport within hospitals. They are loaded with a schematic blue print of the hospital and can be programmed to go from area to area to collect and transport specimens to the proper lab. Reduce-Specimen evaporation, turn around time, risk of disease transmission, specimen contamination Increase-efficiency Dialysis Column chromatography Filtration •coated beads •coated tubes •microtiter plates •magnetic and nonmagnetic microparticles The transport of a quantity of analyte or reagent from one specimen reaction into and contaminating a subsequent one. Continuous-flow system Discrete systems Refrigeration Bar code scanner Timing of the reaction Timing of reaction Forceful dispensing magnetic stirring vigorous lateral displacement a rotating paddle the use of ultrasonic energy Air baths water baths contact with warm plates 10 Chem PPT Flashcards Unit 2 Analyzers can employ different types of optical Photometers measurement devices, list five. Spectrophotometers Reflectance photometers Fluorometers Luminometers One way computers have impacted the clinical all functions are performed uniformly, in a laboratory is: repeatable manner and in the correct sequence The computer controls the electromechanical operation of the analyzer. This means? Having the computer control the automated reproducibility equipment, calculation of results and monitoring of operation will increase the ___ of results. One way computers have impacted the clinical Computers can monitor instrument functions laboratory is: for correct execution and record the sites and Improved acquisition, processing and storage nature of a malfunction so the tech can of operational data from the analyzers. This troubleshoot and repair the problem. means? One way computers have impacted the clinical The instrument operator is alerted to changes laboratory is: in analyzer by the computer directly (ie Computer interfacing with the instrument problems, errors, low reagents, etc) so the tech operator. Explain this. can troubleshoot the problem, if needed, and the issue can be fixed. One way computers have impacted the clinical This allows for LIS and instrument to be linked laboratory is: so results can be transferred directly to the Computer facilitation of communication with patients records. mainframe computer. Explain this. One way computers have impacted the clinical This allows the tech to work on multiple laboratory is: analyzers simultaneously Computer integration of the monitoring functions of one or more analyzers with a single workstation Explain this? Instrument cluster When several different instruments are set up to be controlled by one tech. Work cell A robotic specimen processor monitored by a tech. The work cell performs what tasks? Centrifuge, aliquot, label, transport and store specimens Optical measurement devices includes: - Photometers - Spectrophotometers - Reflectance photometers - Fluorometers - Luminometers 11 Chem PPT Flashcards Unit 2 Impact of integration of computers into automated analyzers and analytical systems are: Features of advanced analytical systems include: Work Cells consist of: Automated Specimen Transport include: Automated Speciment Processing include: Name the three approaches that have been used to automatically sort specimen? Name the automated specimen modules which store specimens refrigerated in specific locations that are logged into a database and Adaptation of other industries’ systems to the laboratory? How many types of conveyor sorting system have been used? What is advantage of conveyor system in the first approach? - Computer control of the electromechanical operation of the analyzer - Computer acquisition, processing and storage of operational data from the analyzers - Computer interfacing with the instrument operator - Computer facilitation of communication with mainframe computers - Computer integration of the monitoring functions of one or more analyzers with a single workstation • Workstations • Equipped for a defined task • Manual specimen transport • Built-in diagnostics • Instrument clusters • Control of several instruments by one technologist • To reduce labor costs - Robotic specimen preparation (Centrifuge, aliquot, label, transport and store specimens) - Technologist as monitor - Conveyor belts - Robot arms - Stand-alone specimen-processing systems - Integrated and modular automation system - Role of process control software - Workload - 13 components of integrated systems 1) A conveyor belt, 2) automated sorter using racks and 3) stand-alone sorters. Automated specimen storage and retrieval Three types Direct sampling from a conveyor track in a loop configuration eliminates the need for separation equipment to sort specimens. 12 Chem PPT Flashcards Unit 2 What is disadvantage of conveyor system in the first approach? What is the second approach of automated processing conveyor system? What is the third approach of automated processing conveyor system? What are Practical Considerations that influence a laboratory’s decision to automate part or all of its operations? List evaluation of requirement in practical considerations ? List Problems of integration in practical considerations? What is Point-of-Care Testing (POCT)? What are other terms for POCT? In what types of environments would POCT be employed? What are some advantages to POCT? What are the main objectives when designing a Point-of-Care instrument? What are key components of POCT device design? Direct sampling may limit the rate of specimen movement on the track to the sampling speed of the slowest workstation. It sorts specimen into group according to their destination in the laboratory such as for hematology or chemistry. The sorter is integral to the conveyor system, and specimens are sorted as they are transported. Evaluation of requirements and, Problems of integration Must be first step in decision to automate Mapping of workflow (Box 16-4) 80% rule of thumb Visits with vendors CLSI standard AUTO03-A Functional control model Device integration Integration of process controllers and software It is a method of clinical laboratory testing in which the analysis is performed at the site close to where the healthcare is provided to the patient. Other terms used to describe POCT included: bedside, near patient, physician's office, extra laboratory, decentralized, off-site, ancillary, alternative site and unit-use testing. POCT would be encountered at home, community pharmacy, retail clinics, and more Reduced turnaround time, improved patient management, reduction in process error and reduction in time delays The main objectives of the design are to: 1. Enable the required reaction to take place that facilitates recognition of the analyte of interest 2. Ensure reliable performance of the device over a specified period of time 3. Minimize the risk of error associated with the use of the device Operator interface, bar code identification systems, sample and reagent delivery mechanisms, reaction cell, sensors, control and communications systems, data management and storage 13 Chem PPT Flashcards Unit 2 What are the POCT devices classified as? Dipsticks, complex strips, and immunostrips are examples of what type of in vitro POCT devices? What are some single-use quantitative cartridge and strip tests with a monitoring devices? What are the analytical principles of in vivo POCT technology? What are the analytical principles of ex vivo POCT technology? What are the analytical principles of noninvasive POCT technology? What are the analytes used in in vivo POCT technology? What are the analytes used in ex vivo POCT technology? What are the analytes used in noninvasive POCT technology? How to POCT devices interface with laboratory information systems? What does CIC stand for? What is CIC? What are POCT01-A2 user requirements? What is the formula for an amino group? What is the formula for a carboxyl group? What is an amino acid? Peptides and proteins are made of which basic structural unit? What is the definition for ampholyte? What is another term for ampholyte? Amino acid metabolism is synthesized from what? What is the daily requirement for protein intake for adults? What is the primary source of amino acids for protein synthesis? What is another source of free amino acids? What happens when the is an absence of protein uptake? In vitro, in vivo, ex vivo, minimally invasive Single-use qualitative strip or cartridge and/or strip devices Glucose monitoring device, cardiac markers, allergy tests, fertility tests, drugs of abuse Optical fluorescence and electrochemistry Optical fluorescence and electrochemistry Electrochemistry/ iontophoresis, and multi wavelength spectrophotometry pH, blood gases, subcutaneous glucose pH, blood gases, electrolytes, glucose Transcutaneous glucose, bilirubin Electronic transfer of data from the analyzers to the LIS and into the patient's electronic medical record Connectivity Industry Consortium Developed point-of-care communication standards which facilitate linking of devices to information management system CLSI connectivity standards to ensure that the POCT devices meet critical user requirement NH2 COOH Organic compounds containing both amino and carboxyl functional groups Amino acids A zero net charge as the negative and positive charge balance at a neutral pH Zwitterion Alpha-keto acids About 0.8 g/kg body weight Dietary protein Endogenous protein Breakdown of muscle protein serves as a source of amino acids 14 Chem PPT Flashcards Unit 2 What are essential amino acids? Where are essential amino acids usually obtained from? How many essential amino acids are there? Name all the essential amino acids What is Kwashiorkor? How is Kwashiorkor obtained? How is Kwashiorkor characterized? Deficiency of both calories and protein is known as? What causes marasmus? What is caused by marasmus? What is the clinical implication known as primary aminoaciduria? Where can the defect be located? What is secondary aminoaciduria? What is the main clinical use of amino acid analysis? What is the most abundant amino acid? What type of specimens are used for the analysis of amino acids? When do amino acids exhibit high diurnal variations? When do amino acids exhibit low diurnal variations? The analysis of amino acids require a normal diet for how many days before collection? True or False? Blood and urine specimen should be collected simultaneously True or False? All medications don’t have to be noted Why should specimen be processed rapidly and frozen rapidly? Amino acids that are not synthesized by humans and are essential dietary constituents for maintaining health or growth Meat, milk, eggs, and fish 8 Isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan, and valine A diet with adequate calories with low protein intake Through malnutrition due to protein deficiency Decreased serum albumin, edema, ascites, growth failure, immune deficiency, and apathy Marasmus Protein-calories malnutrition Generalized muscle wasting A disease due to an inherited enzyme defect In the pathway which a specific amino acid is metabolized or in a transport system for an amino acid Disease of an organ such as the liver which an active site of an amino acid metabolism, or generalized renal tubular dysfunction Detection and monitoring of inherited disorders Glycine Heparanized plasma, urine, and CSF During mid-afternoon In the early morning 2-3 days True False, all medications need to be noted To preserve glutamine 15 Chem PPT Flashcards Unit 2 Why does plasma need to be separated from whole blood rapidly? How do most procedures entail removal of proteins? What does TLC stand for? Name 3 screening tests for the analysis of amino acids What does LC-MS/MS stand for? What does CE stand for? What does GC stand for? Name quantitative tests for the analysis of amino acids What is a protein? How are amino acids linked? Proteins contain a group of complex organic compounds that contain which elements? Which is the characteristic element? What is proteome? Proteome defines the filed of? A peptide is a compound that consists of how many amino acids linked in a chain? Define a peptide bond True or False Proteins act as structural components Proteins facilitate catalysis of what kind of reaction? How can proteins generate energy? True or False Proteins can serve as ion channels and pumps What kind of molecules can proteins act as? True or False? Proteins can effect immune defense Proteins can act as what for intercellular communication? True or False? Proteins constitute signaling networks for extracellular communication So homocysteine can be measured accurately By precipitation or ultrafiltration Thin-layer Chromatography TLC, Guthrie test, and liquid chromatography-tandem mass spectrometry Liquid chromatography-tandem mass spectrometry Capillary electrophoresis Gas chromatography Ion exchange chromatography with postcolumn reaction with ninhydrin, reversedphase high-performance liquid chromatography, LC-MS/MS, CE, and GC A polymer of amino acids By peptide bonds with a specific sequence that folds into a defined structure Carbon, hydrogen, oxygen, nitrogen, and usually sulfur. nitrogen The total complement of proteins present at the time in a call or cell type expressed by the genetic material of an organism proteomics Two or more via peptide bonds The amide bond that is formed between the carboxyl group of one amino acid and the amino group of another True Chemical reactions including synthesis of DNA, RNA and proteins Through electronic transfer True Carrier molecules True Receptors, hormones, and cytokines False, proteins constitute signaling networks for intercellular communication 16 Chem PPT Flashcards Unit 2 Proteins are covalently linked how? the α-amino group of one amino acid is link covalently bonded to what? What is the amino acid with the free amino group in the peptide termed? What is the amino acid with the free carboxyl group termed? Where does protein synthesis begin? What are peptides named from? What are Primary structure? by peptide bonds with the α-carboxyl of a second amino acid N-terminal residue C-terminal residue with the N-terminal residue the N-terminal residue sequence of amino acids in a peptide or protein deoxyribonucleic acid (DNA). What is the sequence of amino acids comprising the polypeptide chain that is genetically encoded? The following are extra questions from 18:22-38 What does the secondary structure of a protein The recurring formations along the describe? polypeptide chain caused by intramolecular forces such as hydrogen bonding What are the three parts of the secondary α-helix,β-pleated sheets, and random coil structure? What does random coil refer to? The segments of protein that lack secondary structure. What does tertiary structure of a protein refer The folding of the chain of amino acids into a to? three dimensional structure How can the tertiary structure be described? Folded, three-dimensional conformation of the protein that is stabilized by both covalent bonds and non-covalent forces mainly involving amino acid R group What has a great effect on a proteins tertiary The proteins environment structure? What can cause denaturation of proteins? Mechanical agitation, heat or extreme chemical treatment What does quaternary structure of a protein The association of multiple peptide bonds refer to? Association of what forms a functional protein Two or more polypeptide chains, or subunits. complex? What happens to molecular size of proteins Size increases when they are denatured? How can proteins be separated? gel filtration chromatography gradient pore gel electrophoresis ultracentrifugation polyacrylamide gel electrophoresis Mass spectrometry What factors can affect protein solubility? pH, ionic strength, temperature, dielectric constant of the solvent. 17 Chem PPT Flashcards Unit 2 Is albumin soluble in water? What else is albumin soluble in? What is albumin insoluble in? What is globulin soluble in? Is globulin soluble in water or saturated and concentrated salt solution? What is the solubility of albuminoids? What enables proteins separation by electrophoresis, isoelectric focusing, and ion exchange chromatography? On what basis does differential adsorption separate polypeptides and other molecules? What are two examples of differential adsorption? What is affinity chromatography? What may Affinity purification of antibodies or proteins be used as? What is density gradient ultracentrifugation used for? What are the physical methods of quantitative analysis? What are two other types of quantitative analysis? What are the methods of qualitative alalysis of proteins? What is the Kjeldahl method in measurement of total protein? What is the standard reference for N2 in the Kjeldahl method? What is the principle of biuret method? Yes dilute and moderately concentrated salt solution (ammonium sulfate) saturated and concentrated salt solution hydrocarbon solvents weak salt solution No Insoluble in most common reagents The variable charge and isoelectric points On the basis of their affinity for a hydrophobic stationary phase Liquid chromatography, and reversed-phase chromatography Highly specific molecular interactions to bind a protein or a peptide to a stationary phase, while other proteins and peptides are removed A preparative technique to prepare specific antibodies or proteins as assay components Used to separate some protein complexes that have a different density when compared with most proteins, such as lipoproteins with low density but with high lipid content Dye binding Direct absorbance measurements Measurement of protein ligands Selective precipitation Mass spectrometry Activity measurements and immunoassays Electrophoresis Chromatography Genetic analysis Functional assays Mass spectrometry A standard reference method based on nitrogen determination 1 gram N2 = 6.25 grams of protein Cupric ions in the alkaline copper tartrate reagent react with peptide bonds to form a blue violet complex proportional to the number of peptide bonds present. 18 Chem PPT Flashcards Unit 2 What does the analysis depend on in the biuret method? What is the composition of the biuret reagent? What is direct spectrophotometric measurement of total protein? What is the principle of the dye-binding method for measuring total protein? What are the commonly used dyes? For measurement of total protein, what is the method of direct spectrophotometric? How is the dye-binding method for measurement of total protein? What dyes are commonly used? What is the Folin-Ciocalteu (Lowry) method? What is a refractometry method for measurement of total protein? How are the turbidimetric and nephelometric methods based on the formation of aggregates or precipitation when every agent? What are precipitation reagents? What is the formula to calculate for normal A/G ratio? What is the A/G ratio if albumin is greater than globulin? What is the A/G ratio if globulin is greater than albumin? What is Serum Protein Electrophoresis (SPE) performed at pH 8.6 in the low ionic strength buffer? The presence of peptide bonds Alkaline copper tartrate as a source of cupric ions Rochelle salt (NaK tartrate) is a complexing agent to keep copper in solution Sodium hydroxide for alkalinity Potassium iodide which prevents autoreduction of copper Measurement of protein content using absorbance of ultraviolet (UV) light at 200 to 225 nm and 270 to 290 nm. Dye binds to protonated amine group of amino acids with absorption at 595 nm Pyrogallol red (for urine and CSF) Coomassie brilliant blue Measurement of protein content using absorbance of ultraviolet (UV) light at 200 to 225 nm and 270 to 290 nm. Dye binds protonated amine group of amino acids with absorption at 595 nm Pyrogallol red (for urine and CSF) Coomassie brilliant blue That is a measurement of refractive index to measure total solutes in urine specimen That is a measurement of refractive index to measure total solutes in urine specimen These are added to lower protein solubility or when an antibody is added to a protein Trichloroacetic acid (TCA) Sulfosalicylic acid (SSA) Sulfosalicylic acid combined with sodium sulfate Benzethonium chloride Benzalkonium salts under alkaline conditions Normal A/G ratio = 1 – 2.5:1 A/G = Albumin/Globulin: 1 A/G = 1: Globulin/Albumin (Inverted A/G ratio) Proteins with a negative charge at pH 8.6 move toward the anode (positive pole) Proteins with a positive charge moved towards the cathode (negative pole) 19 Chem PPT Flashcards Unit 2 How many types of supporting media in SPE are there? What are stains used in serum protein electrophoresis? What are silver stains used for? These are papers, garose gel, cellulose acetate, starch gel and acrylamide gel Amido black and ponceau S Coomassie brilliant blue Silver stains are used for nanogram concentrations of proteins and nucleic acid, they are more sensitive than Coomassie blue stain They are also used for CSF and urine proteins, shades of green, yellow, blue and red What is the intensity of staining individual It is proportional to the amount of protein in a bands of protein generally? band What is a quantitative assessment in SPE Quantitative assessment is done by done? densitometry of stained hands In electrphoresis, when the protein is too high a Each band in the stained pattern should be concentration, what is each band appearance? uniformly colored; holes or doughnut-like appearance within a band occurs How is the order of migration in SPE? The order is following Albumin, Alpha1globulin, Alpha2-globulin, Beta-globulin, Gamma globulin What is a serum preferred? Serum is the preferred specimen Where extra fraction will show if plasma is It will show in the beta-gamma region, and used? fibrinogen is a beta globulin What is the main application of SPE? The main current application of SPE is for the detection or quantification of monoclonal immunoglobulins that occur in disorders, such as multiple myeloma. How does monoclonal immunoglobulins Monoclonal immunoglobulins usually appear usually appear? as sharp bands in the gamma (γ) or beta (β) region How different between monoclonal Monoclonal immunoglobulins differ from immunoglobulins and normal normal immunoglobulins, which migrate as a immunoglobulin’s? diffuse zone, mainly in the gamma region What are 5 types of supporting media for Paper serum protein electrophoresis (SPE)? Agarose gel Cellulose acetate Starch gel Acrylamide gel 3 Stains used for SPE’s include ? Amido black Ponceau S Coomassie brilliant blue What silver stain used for? - nanogram concentrations of proteins and nucleic acid - more sensitive than Coomassie blue stain - used for CSF and urine proteins - shades of green, yellow, blue and red 20 Chem PPT Flashcards Unit 2 Serum Protein Electrophoresis (SPE) What is the order of migration? What if plasma is used as a specimen? What is the preferred specimen in protein electrophoresis? What is the main current application of SPE? What do Monoclonal immunoglobulins usually appear as? What do Monoclonal immunoglobulins differ from normal immunoglobulins? In regards to electrophoresis, the abbreviation IFE stands for? With the application of specific antibodies, IFE can be directed against which immunoglobins/ light chains? IFE is used on what type of gel? Electrophoretic separation of urinary proteins is used to detect what? What is another term for the presence of free monoclonal immunoglobulin light chains? The detection of Bence-Jones proteins can be indicative of what disease? Fill in the Blank: relies on the separation of ions in an electrical field in a vacuum? In mass spectrometry, separation of molecules is purely based on what? -the intensity of staining individual bands of protein generally is proportional to the amount of protein in a band -quantitative assessment is done by densitometry of stained hands -In electrophoresis, each band in the stained pattern should be uniformly colored; holes or doughnut-like appearance within a band occurs when the protein is too high a concentration. Remedy : Dilute elevated specimens before re-running the electrophoresis 1.Albumin 2.Alpha1-globulin 3.Alpha2-globulin 4.Beta-globulin 5.Gamma globulin - extra fraction will show in the beta-gamma region - Fibrinogen is a beta globulin Serum is for the detection or quantification of monoclonal immunoglobulins that occur in disorders, such as multiple myeloma. sharp bands in the gamma(γ) or beta(β) region normal immunoglobulins, which migrate as a diffuse zone, mainly in the gamma region Immunofixation Electrophoresis (IFE) Immunoglobins: IgG, IgM, IgA Also kappa (κ) and lambda (λ) light chains Agarose gel The presence of free monoclonal immunoglobulin light chains or other lowmolecular-mass proteins Bence-Jones Proteins Multiple Myeloma Mass Spectrometry Mass-to-charge (m/z) ratio 21 Chem PPT Flashcards Unit 2 In what case would a mass spec. be ideal? What is an Acute Phase Response (APR)? Proteins affected or increased by APR are known as? Known Positive APPs include: Proteins not affected or decreased by APR are called? Known Negative APPs include: What is Prealbumin (Transthyretin)? Ideal for highly precise qualitative analysis of peptides A systemic response to infection, tissue injury or inflammatory processes resulting in fever, increased WBC count, and changes in the concentration of many plasma proteins. Positive acute phase proteins (APPs) α1-antitrypsin Fibrinogen α1- acid glycoprotein C-reactive protein Haptoglobin Serum amyloid Ceruloplasmin C4, C3 Negative acute phase proteins (APPs) Transthyretin Albumin Transferrin A transport protein of thyroid hormones and RBP A hollow core containing T3 and T4 binding sites Negative cooperativity Prealbumin/ Transthyretin is composed of four identical subunits that associate to form what? Binding of one hormone molecule decreases the binding affinity of the second so that only one site is normally occupied. This is known as what? Where is prealbumin/ transthyretin In the liver and to a lesser extent in the choroid synthesized? plexus of the central nervous system, accounting for the relatively high concentration in CSF Synthesis of prealbumin/ transthyretin is stimulated by what hormones and drugs? Prealbumin/ Transthyretin is often used as indicator of? Prealbumin/ Transthyretin is increased during what conditions? Prealbumin/ Transthyretin is decreased during what conditions? Synthesis is stimulated by glucocorticosteroid hormones, androgens and many nonsteroidal anti-inflammatory drugs (NSAIDs) including aspirin Protein Nutrition With corticosteroid or NSAID therapy Hodgkin Disease Inflammation and malignancy Cirrhosis of the liver Protein-losing diseases of the gut or kidneys 22 Chem PPT Flashcards Unit 2 What is the migration pattern for prealbumin/ transthyretin on Serum Protein Electrophoresis (SPE)? Name 2 methods that can measure prealbumin: What is Retinol-Binding Protein (RBP)? What element is required for the synthesis of RBP? What is required for RBP to transport out of the Golgi apparatus? Where is RBP absorbed in the body? Fill in the Blank: Serum concentration of RBP is chronic renal disease. RBP is increased with? What is the most abundant protein in the plasma from mid-gestation until death? Albumin is a major protein component of most extra vascular body fluids including? Albumin is increased during? Albumin is decreased in? Immunoturbidimetric or immunonephelometric methods A transport protein bound to prealbumin Zinc Retinol It is absorbed by the proximal renal tubular cells and catabolized Increased in RBP is decreased in? Albumin is synthesized by? Albumin is a major transporter of? Migrates as a minor band anodal to albumin Corticosteroid NSAID therapy And in Hodgkin Disease Liver disease, protein malnutrition, and acute phase response (APR) Albumin CSF Interstitial fluid Urine Amniotic fluid The hepatic parenchymal cells Free fatty acids, bilirubin, calcium, thyroid and steroid hormones, drugs and thiol-containing compounds Dehydration Prolonged application of the tourniquet Specimen evaporation before analysis Analbumemia – a rare genetic deficiency with plasma albumin concentration less than 0.5 g/L Inflammation – Albumin is a negative APP. Acute and chronic inflammation are common causes of hypoalbuminemia Hepatic disease 23 Chem PPT Flashcards Unit 2 How does hepatic disease decrease the concentration of albumin? How is albumin decreased in urinary loss? How is albumin decreased in Gastrointestinal loss? How is albumin decreased in protein energy malnutrition (Marasmus)? How is albumin decreased in burn injury? How is albumin decreased in Edema and ascites? Whsat are two ways for Albumin Determination? What is High-Density Lipoprotein? Loss of parenchymal cells function by 50% Nutritional deficiency Increased distribution into the extravascular space Direct inhibition of synthesis by toxins such as alcohol - Small increases in albumin excretion to >30 mg/d indicate early stages of glomerular or tubular injury and risk of progression to more severe kidney disease (Microalbuminuria) - Severe glomerular injury produces the nephrotic syndrome, which is characterized by excretion of >3.5 g/d of protein (mainly albumin). Inflammatory disease of the intestinal tract is associated with increase gastrointestinal loss of albumin Albumin concentration help to detect and monitor protein nutritional status Burn patients experience severe loss of albumin from wounds due to the combined effects of epithelial losses, accelerated catabolism and the APR Edema and ascites are usually secondary to increased vascular permeability, and albumin levels are decreased as a result of redistribution of albumin into extravascular space - Dye-Binding methods • Bromcresol green (BCG) • Bromphenol blue (BPB) • Bromcresol purple (BCP) • Hydroxyazobenzenebenzoic acid (HABA) - Immunoturbidimetric and nephelometry Also called alpha lipoprotein or good cholesterol Characterized by high density because of its protein and phospholipid content Apolipoprotein A1 the major protein, is a negative APP that is considered to have antiinflammatory properties 24 Chem PPT Flashcards Unit 2 What is α1-Acid Glycoprotein? What factors does α1-Acid Glycoprotein increases in? What factors does α1-Acid Glycoprotein decreases in? How is electrophoresis used for α1-Acid Glycoprotein Determination? How is α1-Acid Glycoprotein Determination quantified? What is α1-Antitrypsin (AAT)? - Also known as orosomucoid One of the highest concentration proteins in the alpha-1 globulin religion - Amember of the lipocalin family of proteins that bind lipophilic substances, such as progesterone and basic drugs including propanolol, chlorpromazine, quinidine, cocaine and benzodiazepine. - It is synthesized mainly by hepatic parenchymal cells - A positive APP - G.I. inflammatory disease - Malignant neoplasms - Corticosteroids and NSAIDs medication - Estrogen medication - Protein-losing syndrome such as nephrotic syndrome Using periodic acid Schiff or other carbohydrate stains By immunochemical methods, including turbidimetry and nephelometric. - Is a serpin (serine proteinase inhibitor) that inactivates serine proteases such as neutrophil elastase - Synthesize primarily by hepatic parenchymal cells - It is the most important inhibitor of leukocyte elastase, as release by neutrophils - Levels are elevated by the APR and by estrogen oral contraception - Levels are low in individuals with neonatal respiratory distress syndrome, severe pancreatitis and protein-losing disorders - Quantified by immunoturbidimetry or immunonephelometry - Phenotyping of AAT is performed by isoelectric focusing 25 Chem PPT Flashcards Unit 2 What is α -Fetoprotein (AFP)? - - What is Haptoglobin (Hp)? - - - What is α2-Macroglobulin (AMG)? - - - - - - Is the most abundant plasma proteins in the early embryonic life Homologous to albumin but differs in having about 4% carbohydrate Serum concentration serves as a tumor marker for Hepatocellular and germ cell carcinoma Maternal serum concentrations are analyzed as indicators of fetal trisomy of chromosome 18 or 21 Concentrations are increased by glucocorticosteroids, androgens and many NSAIDs Levels are elevated in selective proteinlosing syndrome such Nephrotic syndrome Significantly elevated in biliary obstruction in the absence of severe hepatocellular disease Measured by immunoturbidimetry and immunonephelometry A major plasma proteinase inhibitor A very large molecule that does not diffuse from the plasma space into extracellular fluids in significant amounts Homologous to complement components C3 and C4 in inhibiting classes of proteinases, including those with serine, cysteine and metal ions in their catalytic sites Synthesized by the liver Levels are higher in women of childbearing age and in infants and children Increased in nephrotic syndrome Decreased in severe acute pancreatitis or with advance carcinoma of the prostate Ccan be measured by zone electrophoresis in the alpha2-globulin region Quantified by immunoturbidimetry or immunonephelometry 26 Chem PPT Flashcards Unit 2 What is Ceruloplasmin (Cp)? Following are clinical significant of what type of plasma protein? decreased levels are due to dietary copper insufficiency (including malabsorption), associated with neutropenia, thrombocytopenia, low serum iron and hypochromic, normocytic, or microcytic anemia that does not to respond to iron therapy What disease is characterized by increased total body copper and deposited in tissues including the hepatic parenchymal cells, the brain, and the periphery of the iris (resulting in the characteristic Kayser-Fleisher ring)? How measure Ceruloplasmin (Cp)? What is separation and transportation or holding condition for Ceruloplasmin (Cp)? What is concentration of Ceruloplasmin (Cp) at birth? When is peak concentration of Ceruloplasmin (Cp)? What is concentration of Ceruloplasmin (Cp) for adult? What is other name for Transferrin? An α2-globulin that contains approximately 95% of the total serum copper, giving it a blue color - May give plasma a greenish tint when concentrations are significantly elevated during pregnancy - Synthesized primarily by the liver, and is responsible for catalysis of reduction and oxidation reactions - Important in regulating the ionic state of iron, oxidizing from the ferrous (Fe2+) to the ferric (FE3+) state, thus permitting incorporation of the iron into transferrin - It is a weak, late-reacting positive APP - Increased significantly by estrogens, as in pregnancy or with the use of oral contraceptives Ceruloplasmin (Cp) - Wilson disease, or hepatolenticular degeneration by immunoturbidimetry and immunonephelometry serum or plasma should be separated from blood as soon as possible specimen should be refrigerated for up to three days or frozen at below -70°C for prolonged storage Low at birth increased to peak concentrations at 2 or 3 years of age decline slowly until adolescence, when adult concentrations are reached also known as siderophilin 27 Chem PPT Flashcards Unit 2 What is the major plasma transport protein for iron? What is the main factor in plasma which Transferrin accounts for it? Where is Transferrin in the body synthesized and how it migrates in electrophoresis? What is relationship between Transferrin and iron concentration? What is concentration of Transferrin and iron saturation in hereditary hemochromatosis (iron-overload state)? What is diurnal cycle for Transferrin? What is level of Transferrin in pregnancy and inflammation? What is the level of synthesis of Transferrin in following diseases? chronic liver disease, protein malnutrition, protein loss as seen in nephrotic syndrome or in protein-losing enteropathy What are laboratory considerations for Transferrin determination? What is the formula for TIBC (Total Iron Binding Capacity)? Transferrin (TRF) migrates in…………on routine serum electrophoresis. What is equation which TIBC is used to estimate TRF? What Low-Density Lipoprotein is termed on the basis of its electrophoretic mobility? What percentage of LDL is lipid? What percentage of LDL is protein? What is the main lipid component of LDL? What is the main protein component of LDL? Transferrin total iron binding capacity synthesized primarily in the liver and usually migrates in the β1-region on routine clinical electrophoresis of serum plasma concentrations are inversely related to iron concentration concentration is normal in hereditary hemochromatosis (iron-overload state), but iron saturation often exceeds 55% serum iron concentration usually is highest in the morning and decreases markedly in the evening high concentrations are present in pregnancy and during estrogen administration is a negative APP, and low concentrations occur in inflammation and malignancy Decreases Serum electrophoresis Immunoturbidimetry and Immunonephelometry methods Photometric assays for TIBC (Total Iron Binding Capacity) TIBC = UIBC + Iron Where: TIBC = total iron binding capacity UIBC = unsaturated binding capacity β1 –region TRF (mg/dL) = 0.70 x TIBC (µg/dL) or Iron % Transferrin saturation = --------------- x 100 TIBC β-lipoprotein 80% 20% cholesterol ester apolipoprotein B 28 Chem PPT Flashcards Unit 2 Increase in LDL concentration confer increased risk of ……………..? How concentration of LDL are assessed? Following is characteristic of what plasma protein? a low-molecular-mass protein found on the cell surfaces of all nucleated cells Which protein plasma is the light or beta chain of the human leukocyte antigens (HLAs)? Which protein is high in individuals with renal failure, inflammation, and neoplasm especially those associated with B lymphocytes Name a protein marker for renal tubular function? BMG levels has been used as a staging criterion for what type of disease? Name a protein plasma which can deposit as amyloid, leading to systemic amyloidosis in many patients of long-term dialysis? What protein is the terminal component of the coagulation system, aggregates to form a fibrous network when it is cleaved by the protease thrombin? What protein is a highly elongated protein that consist of six polypeptide chains joined by disulfide bonds? Fibrinogen is positive or negative APP? What protein is the major contributors to plasma viscosity because of its large size? What does occur when Fibrinogen is low? cardiovascular disease assessed by calculation of LDL cholesterol that are based on other lipid measurements, direct quantification of LDL cholesterol, or quantification of apolipoprotein B β2-Microglobulin (BMG) β2-Microglobulin (BMG) β2-Microglobulin (BMG) urinary BMG (β2-Microglobulin) multiple myeloma β2-Microglobulin (BMG) Fibrinogen Fibrinogen Positive Fibrinogen the result of consumption from extensive bleeding or dysregulation of the coagulation system What is the level of Fibrinogen in disseminated Low intravascular coagulation (DIC)? In what disease Dysfibrinogenemia (functional Liver disease disorders of fibrinogen) may be seen? What high levels of Fibrinogen on a chronic increased risk of cardiovascular disease, basis are associated with? which may relate to increase plasma viscosity or the increased tendency for thrombosis One of the assay to measure Fibrinogen is? functional clotting assays What method can be used to measure measured by immunoturbidimetry methods or Fibrinogen level? by turbidimetric methods based on the addition of precipitating reagents 29 Chem PPT Flashcards Unit 2 What protein may be mistaken for a paraprotein if not completely removed from serum on serum protein electrophoresis? Where C-reactive Protein (CRP) is found? Name the bacteria that CRP is able to bind the cell wall C polysaccharide of it? CRP is positive or negative APR? CRP used extensively as a marker of……….? Where CRP synthesized in the body? What is function of CRP? CRP binds to a variety of compounds is dependent on the presence of …………? What is diagnostic window for CRP? In what disorders CRP increases? CRP is a stronger stimulus in bacteria or viral infection? Name the protein marker for bacterial infection in newborns? What protein marker is used to assess the activity of disorders such as rheumatoid arthritis and Crohn disease? What are referred of High-sensitivity CRP (hsCRP) assay? What types of assays are used for high sensitivity CRP? What type of gel is used for electrophoresis of CRP? What are complement proteins and where are they found? What complement proteins are in the Classical Pathway? How is the Classical Pathway activated? What complement proteins are in the Alternative Pathway? Fibrinogen in the sera of acutely ill individuals Streptococcus pneumoniae an early positive APR inflammation Liver to protect the body against foreign organisms and to assist in clearing tissue debris Calcium Levels begin to rise within 6 to 12 hours of the onset and peaks within 48 hours myocardial infarction, stress, inflammation, trauma, neoplastic proliferation, infection, surgery Bacterial infection is usually a stronger stimulus than viral infection CRP CRP Detection limit of about 1 mg/L levels greater than 2 mg/L is suggestive of increased cardiovascular risk Particle-enhanced immunoturbidimetry, nephelometry, or sandwich immunoassays with fluorescence or chemiluminescent detection. Cellulose acetate or agarose gel Complement proteins help to complement the ability of antibodies and phagocytic cells to clear pathogens from an organism. They are found in normal blood plasma and also as cellular receptors on cell surfaces. It includes C1, C4, C2, and C3 (in order of activation) It is activated primarily by complexes of immunoglobulins with antigen or bacteria or other ligands with CRP Includes C3, factor B and D, and properdin 30 Chem PPT Flashcards Unit 2 How is the Alternative Pathway activated? What complement proteins are in the Lectin Pathway? How is the Lectin Pathway activated? What complement proteins are in the Membrane Attack complex? What protein is activated through all of the pathways? What is chemotaxis? What is opsonization? What is phagocytosis? Where are complement components mainly synthesized? Of all the complement proteins, which is the most abundant? What does a genetic deficiency of C2 and C4 cause? What causes hereditary angioedema? What are coagulation proteins? What organ primarily produces all of the coagulation factors? Of all the coagulation factors, which is the most important? What causes low concentrations of clotting factors? What are some hereditary disorders that cause excessive bleeding? What may cause a risk of thrombosis? It is activated by bacterial lipopolysaccharides, cellular proteases and cobra venom It includes mannan-binding protein (MBP), ficolins, and proteases It is activated by binding of ficolins and MBP to mannose-rich oligosaccharides that are present in the cell walls of many microorganisms Includes C5 through C9 and inserts into cell membranes and lyses cells The common step involved is the activation of C3 to C3b. The movement or orientation of an organism or cell along a chemical concentration gradient or in response to a chemical stimulus It refers to an immune process where particles such as bacteria are targeted for destruction by an immune cell known as a phagocyte The engulfing and ingestion of bacteria or other foreign bodies by phagocytes to form an internal vesicle known as a phagosome The liver C3 A genetic deficiency of C2 and C4 is associated with autoimmune immune complex diseases such as systemic lupus erythematosus (SLE), polymyositis and glomerulonephritis. Heterozygous deficiency of C1 inhibitor results in hereditary angioedema (HAE) A complex system designed to prevent bleeding from injuries by forming blood clots The liver Fibrinogen The result of hereditary deficiencies, consumption by active clotting, liver disease or anticoagulant therapy Hemophilia A, factor VIII deficiency, hemophilia B, and factor IX deficiency Risk of thrombosis may be result of factor V Leiden deficiency, antithrombin III deficiency and protein C deficiency 31 Chem PPT Flashcards Unit 2 What are immunoglobulins (antibodies)? What stimulates the production of immunoglobulins, and what do they attack? What is the structure composition of immunoglobulins? On what chromosomes are the light and heavy chains encoded? What forms the antigen-binding site on the immunoglobulins? What are heavy chains made up of? What are light chains made up of? Where are immunoglobulins synthesized? What are the five classes of immunoglobulins? Which of the five immunoglobulins are the most abundant? What does IgG do? What is the circulating half-life of IgG? Which, if any, of the immunoglobulins can cross the placenta blood barrier? What are the four subclasses of Immunoglobulin G (IgG)? They’re a family of proteins the contain highly specific antigen-binding sites. Synthesis of immunoglobulins is stimulated by foreign immunogens, leading to immunoglobulins that selectively bind foreign molecules or organisms. All immunoglobulins include one or more basic units consisting of two identical heavy (H) chains encoded on chromosome 14 and two identical light (L) chains encoded on chromosome 2 that are joined by disulfide bonds. Heavy chain is encoded on chromosome 14 and the light chains on chromosome 2 Two variable domains, one from the light chain and one from the heavy chain, together form an antigen-binding site. They consist of gamma, alpha, mu, delta, and epsilon Kappa and Lambda Immunoglobulins are synthesized by cells of the B-lymphocyte lineage. IgG, IgA, IgM, IgE, and IgD The most abundant class of Ig, making up 70 to 75% of total Ig. Of this amount, 65% is extravascular and 35% is found in plasma. It is responsible for long-term physiologic protection and the majority of neutralization of bacteria and virus antigens Approximately 22 days IgG IgG includes four subclasses - IgG1, IgG2, IgG3, and IgG4 - IgG1 and IgG3 strongly activate complement via the classical pathway - IgG2 weekly activates complement - IgG4 does not activate complement - IgG1 and IgG3 bind Fc receptors on phagocytic cells can cross the placenta via receptor-mediated active transport IgG1 is the major neonatal Ig. 32 Chem PPT Flashcards Unit 2 What are some characteristics of Immunoglobulin A (IgA)? - What are two types of Immunoglobulin A (IgA)? - Where is Immunoglobulin A (IgA) synthesized and secreted? - - - What is Immunoglobulin M (IgM)? - - What is Immunoglobulin E (IgE)? - Makes up 10% to 15% of serum immunoglobulin On electrophoresis, IgA migrates near the junction of the beta and gamma regions IgA also activates the complement by the alternative pathway Plasma dimeric IgA1: sedimentation coefficient of 7S Secretory dimeric IgA2: sedimentation coefficient of 11S and present in saliva, tears, sweat, milk, colostrum and secretion of nasal, gastrointestinal and tracheobronchial origin It is synthesized mainly by plasma cells in the mucous membranes of the gut and bronchi and in the ductules of the lactating breast This secretory component helps transport secretory IgA across mucosal epithelium and into secretions Secretory IgA is more abundant than IgG in colostrum and milk and may help protect neonates from intestinal infection Produced at early stages of β-cell development. Comprises about 5%-10% of the total circulating immunoglobulins Largest immunoglobulin, a pentamer (molecular weight > 900 kilodaltons) Most primitive immunoglobulin and is found on the surface of early B lymphocytes First or primary response immunoglobulin to be produced following antigen assault. Monomeric immunoglobulin in plasma Lowest concentration (about 0.05 mg/dL) Attaches rapidly to the membranes of mast cells by its Fc region Cross-linking of two IgE molecules by antigen causes release of histamine, heparin and vasoactive amines by mast cells 33 Chem PPT Flashcards Unit 2 What role does Immunoglobulin E (IgE) play in allergic or hypersensitivity reaactions? What is Immunoglobulin D (IgD)? What is the significance of immunoglobulin deficiency? What is Polyclonal Hyperimmunoglobulinemia? What are some characteristics of Monoclonal Immunoglobulins (Paraproteins)? What malignant neoplasm is usually a single clone of plasma cells? What is the tumor called when the plasma cells proliferate diffusely throughout the bone marrow? What is produced due to multiple myeloma? What are decreased due to multiple myeloma? - Urticaria Hay fever Asthma Eczema A monomeric immunoglobulin in plasma - Active on the cell surface of B lymphocytes - Labile upon storage - Not routinely measured - Immunodeficiency may be the result of a deficiency of a single factor or of a combinations affecting multiple systems and factors - It results in increased susceptibility to infections that usually do not cause disease in people with normal immune systems - Polyclonal increases in plasma immunoglobulins constitute the normal response to infection - IgG response predominates in most autoimmune responses; IgA in skin, gut, respiratory and renal infections; and IgM in primary viral infections and with bloodstream parasites like malaria. - Produces a discrete band on electrophoresis often referred to as an M-spike or M-protein - up to 25% of paraproteins are benign and have been termed monoclonal gammopathy of undetermined significance (MGUS) - Bence-Jones proteins: the primary clinical interest in identifying paraproteins involves the detection or monitoring of proliferative disorders of B lymphocytes Multiple myeloma plasmacytoma Osteolytic bone lesions Bone marrow cells like platelets, red cells, neutrophils 34 Chem PPT Flashcards Unit 2 What is inhibited due to multiple myeloma? What consequently happens? Lymphomas or chronic lymphocytic leukemias are examples of ___. Where do lymphoid tumors arise? What is a malignant proliferation of plasmacytoid cells producing IgM? What causes hyperviscosity that may require treatment by plasma exchange? What is the rare disorder in which a free Ig heavy chain is produced? What is the most common form of Heavy Chain disease? What is alpha chain disease associated with? What can cause malabsorption in alpha chain disease? What are serum proteins or protein complexes that precipitate at a temperature lower than normal core body temperature? What is the result of precipitation in tissues? How do you lower a patient's cryoglobulin concentrations? What do type I cryoglobulins consist of? How many days are serum usually refrigerated for cryoglobulin analysis? What is the next step after 7 days? What happens when cryoglobulins that precipitated in the cold are warmed back to 37C? What is a pathological process in which proteins are deposited in tissues as aggregates (amyloid), and form b-sheet structures? What can result from amyloidosis? What are stable structures resistant to proteolysis and normal clearance mechanisms? Aggregates accumulate over time. What happens when there is increased production of specific proteins, genetic variants of proteins, or fragments of proteins? Where are the tissues obtained in order to diagnose amyloidosis? Normal plasma cells Synthesis of other immunoglobulins is reduced, recurrent infections may occur Lymphoid tumors From less mature stages in B-lymphocyte development Waldenstroms Macroglobulinemia IgM and IgM paraproteins Heavy Chain disease Alpha chain disease The heavy chain of IgA Intestinal infiltration with clonal lymphocytes Cryoglobulins Vasculitis and ischemic injury to peripheral tissues of the lower temperature Patient must be kept in a warm environment Monoclonal immunoglobulins, often IgM 7 days Centrifugation They should redissolve Amyloidosis Kidney failure, heart failure, and peripheral neuropathies Aggregates TRUE Formation of amyloid From fat aspirates, rectal biopsy specimens, or biopsy specimens of affected tissues 35 Chem PPT Flashcards Unit 2 What can the b-sheet structure of the amyloid be stained with? What occurs as the result of increased concentrations of proteins including... ...Ig light chain paraproteins? ...BMG in renal failure? ...Serum amyloid A Urine usually contains much lower protein concentration than plasma. How does urine maintain its concentration? Why is analysis of urinary proteins mainly performed? What is the increase of urinary protein excretion called? When can cause proteinuria? Why is glomerular proteinuria sometimes referred to as albuminuria? Glomerular proteinuria is seen in conditions including diabetes, systemic lupus erythemotosis, IgA nephropathy, glomerularnephritis, hepatitis and HIV infections. What is characterized by hypoalbuminemia, hypercholesterolemia, and edema Excretion of ____ g/d protein is a criterion for nephrotic syndrome. What signifies early stage of glomerular injury and a risk factor for progressionof kidney disease in diabetes? How is urine albumin detected? When can functional or benign proteinuria occur? Postural or orthostatic proteinuria is associated with the upright position. First voided urine is analyzed to detect orthostatic proteinuria. What is the appearance of low molecular weight proteins in the urine as a result of decreased reabsorption by the proximal tubules? Congo red dye AL amyloidosis AB2 amyloidosis AA amyloidosis TRUE Through the combined action of glomerular filtration and tubular uptake of protein To diagnose kidney disease or disorders with paraprotein production Proteinuria Glomerular injury, postrenal proteinuria, tubular injury, overflow proteinuria of low molecular weight proteins Because albumin is the major protein TRUE Nephrotic syndrome >3.5 Microalbuminuria (30-300mg/d) By dipsticks, followed by quantitative assays like pyrogallol red dye binding assays and benzethonium chloride turbidity assays With exercise fever and exposure to cold TRUE TRUE Tubular proteinuria 36 Chem PPT Flashcards Unit 2 What is Fanconi syndrome? What are some of the causes of tubular proteinuria? What occurs when an increased load of small proteins (hemoglobin, myoglobin, free Ig light chain paraproteins) filtered through the glomerulus exceed the tubular uptake capacity? What does detection of light chains depend on in overload proteinuria? What color does hemoglobin or myoglobin confers to urine, yielding positive reactions in the dipstick test for blood? What arises from injury, inflammation or malignancy of the lower urinary tract? What does Postrenal proteinuria reveal under microscopic examination of urine? What helps to distinguish whether a process is occurring in the kidneys or in the lower urinary tract? What is an excellent screening tests for major glomerular injury (sensitive to albumin)? What is the extracellular fluid around the brain and spinal column? Analysis of CSF is mainly performed to determine? Which disease aids increased intrathecal synthesis of immunoglobulins? Methods for measuring CSF protein includes? What is analyzed in proteins in amniotic fluid? What represents the fluid secreted by several salivary glands containing amylase and small peptides? Which immunoglobulin is tested in saliva for evaluation of possible immunological deficiency? What is used in the diagnosis of gastrointestinal protein loss? What has been used as a measure of disease activity in inflammatory bowel disease? A hereditary disorder of tubular functio Fanconi syndrome, toxicity from compounds, poisoning from heavy metals, ischemia due to obstruction of blood flow, decreased blood flow in shock or heart failure, toxicity from overload with proteins Overload Proteinuria Electrophoresis and immunochemical testing Brown Postrenal Proteinuria Inflammatory and malignant cells and bacteria Cast that arise in kidney tubules Dipstick test Cerebrospinal fluid Increased permeability of blood-brain barrier (BBB) or increased intrathecal synthesis of immunoglobulin. Multiple sclerosis Pyrogallol red dye-binding assays Benzethonium chloride turbidity assays Biuret assays α-fetoprotein (AFP) Proteins in saliva and oral fluid IgA assay of feces for (α1-antitrypsin) AAT Lactoferrin and calprotectin 37 Chem PPT Flashcards Unit 2 Refers to proteins abnormally accumulated in the peritoneal (abdominal) and pleural (lung) cavities What are enzymes? How specific are they and where are the majority found? What do the increases of serum enzymes usually indicate and why are they useful? What are Enzymes? What is necrosis? How many classes of Enzymes are there? What are the Classification of enzymes Oxidoreductase? Proteins in Peritoneal and Pleural Fluid Enzymes are organic catalysts than hasten a chemical reaction without themselves being consumed or undergoing a chemical change. They have a high degree of specificity for a certain substrate or class of substrates and the majority are intracellularly found. increased serum levels are due to tissue damage and necrosis, therefore they are used diagnostically to asses tissue damage. are organic catalysts than hasten a chemical reaction without themselves being consumed or undergoing a chemical change protein in nature with high degree of specificity for a certain substrate or class of substrates. majority are intracellularly found amounts found in serum are result of normal cellular turnover; specialized tissue or widely distributed with tissue-specific isoenzymes or isoforms increased serum levels are due to tissue damage and necrosis (markers of tissue damage) thus, used diagnostically to assess tissue damage Necrosis is tissue damage due to elevating serum levels. There are 6 classes of Enzymes: I. Oxidoreductases II. Aminotransferases/Aminotransaminase s III. Hydrolases IV. Lyases V. Isomerases VI. Ligases Oxidase Cytochrome oxidase Dehydrogenase Lactate dehydrogenase (LDH) Malate dehydrogenase (MDH) Isocitrate dehydrogenase (ICD) Glucose-6-phosphate dehydrogenase (G-6-PD) 38 Chem PPT Flashcards Unit 2 What are the Classification of enzymes Aminotransferase/Aminotransaminase? What are the Classification of enzymes Hydrolase? What are the Classification of enzymes Lyases? Two types of Isomerases: Another name for Ligases enzyme: The roles of Oxidoreductases: The activities of Aminotransferases /Aminotransaminases: The factors of Hydrolases: Aspartate aminotransferase (AST / SGOT) Alanine aminotransferase (ALT / SGPT) Creatine kinase (CK /CPK) Gamma glutamyl transferase (GGT) Ornithine carbamyl transferase (OCT) Esterase Acid phosphatase (ACP) Alkaline phosphatase (ALP) Cholinesterase (CHS) Lipase (LPS) Peptidases Typsin (PTS) Pepsin (PPS) Leucine aminopeptidase (LAP) Glucosidase Amylase (AMS) Amylo-1,6 glycosidase Galactosidase Aldolase (ALD) Carbonic anhydrase Glutamate decarboxylase Pyruvate decarboxylase Tryptophan decarboxylase 1) Glucose phosphate isomerase 2) Ribose phosphate isomerase Glutamine synthetase a) Catalyze an oxidation-reduction reaction b) Catalyze the addition or removal of hydrogen from compounds c) Require a coenzyme (NAD or NADP) as a hydrogen acceptor or donor in order to function a) Catalyze the transfer of amino or phosphate groups between compounds b) Require coenzyme (pyridoxal-5’phosphate [P-5’-P]) for the amino transfer reactions a) Catalyze the hydrolysis of ether and ester b) They split molecules with the addition of water c) Do not usually require coenzymes but often need activators 39 Chem PPT Flashcards Unit 2 How do Lasses operate inside a cell? a) Catalyze the removal of groups without hydrolysis (loss of hyroxide ion) b) Split molecules between carbon-tocarbon bonds without the addition of water c) Resulting products usually contain carbon double bonds How do Isomerases function? a) Catalyze the interconvertion of geometric or optical isomers b) Catalyze the intramolecular conversions such as the oxidation of a functional group by an adjacent group within the same molecule What are the tasks of Ligases? a) Catalyze the joining of two substrate molecules b) Catalyze the union of two molecules accompanied by the breakdown of a phosphate bond in adenosine triphosphate (ATP) The following are additional questions on slides 4-20 How many classes of Enzymes are there? I. Oxidoreductases II. Aminotransferases/Aminotransaminase s III. Hydrolases IV. Lyases V. Isomerases VI. Ligases What are the classification of enzymes Oxidase Oxidoreductase? Cytochrome oxidase Dehydrogenase Lactate dehydrogenase (LDH) Malate dehydrogenase (MDH) Isocitrate dehydrogenase (ICD) Glucose-6-phosphate dehydrogenase (G-6-PD) What are the classification of enzymes Aspartate aminotransferase (AST / Aminotransferase/Aminotransaminases? SGOT) Alanine aminotransferase (ALT / SGPT) Creatine kinase (CK /CPK) Gamma glutamyl transferase (GGT) Ornithine carbamyl transferase (OCT) What are the enzymes Hydrolases actions? Catalyze the hydrolysis of ether and ester they split molecules with the addition of water. Do not usually require coenzymes but often need activators. 40 Chem PPT Flashcards Unit 2 What are the enzymes Lyases actions? Catalyze the removal of groups without hydrolysis (loss of hyroxide ion). Split molecules between carbon-to-carbon bonds without the addition of water. Resulting products usually contain carbon double bonds. What are the enzymes Isomerases actions? Catalyze the interconvertion of geometric or optical isomers. Catalyze the intramolecular conversions such as the oxidation of a functional group by an adjacent group within the same molecule. What are the enzymes Ligases Actions? Catalyze the joining of two substrate molecules. Catalyze the union of two molecules accompanied by the breakdown of a phosphate bond in adenosine triphosphate (ATP). What is Phosphatase? is an enzyme that removes a phosphate group from its substrate by hydrolyzing phosphoric acid monoesters into a phosphate ion and a molecule with a free hydroxyl group. What is Acid Phosphatase? Promotes the hydrolysis of orthophosphate esters. Found in almost all body tissues, but significantly in RBC’s and platelets. In adult men, 50% is found in the prostate gland. High levels are found in semen. What are the requirement substrates to measure p-nitrophenylphosphate (PNPP) (preferred Total ACP Activity? substrate for continuous monitoring) thymolphthalein monophosphate (TMP) (substrate of choice) What is p-nitrophenylphosphate (PNPP)? Is a non-proteinaceous, non-specific substrate used to assay protein, alkaline and acid phosphatases. The PNPP phosphatase activity is measured using a continuous or single-point spectrophotometric assay based on the ability of phosphatases to catalyze the hydrolysis of PNPP to p-nitrophenol, a chromogenic product with absorbance at 405 nm (1). What is thymolphthalein monophosphate Obtained from 10 commercial suppliers were (TMP)? compared spectrophotometrically at 445 and 595 nm, liquid-chromatographically with monitoring at 254 nm, and enzymically by measurements of activity of prostatic acid phosphatase in human serum. 41 Chem PPT Flashcards Unit 2 What is the measurement of Total ACP Activity? What is isoenzymes of Acid Phosphatase (ACP)? What is Isoenzyme Test Include: What is the Clinical Significance of ACP? What is Metastatic Carcinoma? What enzyme(s) have liver as the primary source and can be used to detect hepatic parenchymal disease? What enzyme is a indicator in muscle disease ? What enzyme(s) associated with detecting pancreatic disease? Where would you find enzyme lipase ? What does ACP - Acid Phosphatase do? Where would you find ACP? In adult men, where is 50% of ACP found? What condition the ACP activities were taken placed at? What is tartrate used in isoenzyme testing? D- What are the clinical significance of ACP? What is ALP alkaline phosphatase? What’s the optimal pH for ALP All reactions are carried out at a pH lower than 6.0 Falsely low values are produced by improper anticoagulant use (heparin, fluoride, oxalate) Hemolysis produces false elevation Specific Prostatic Phosphatase Non-Specific Prostatic Phosphatase or Red Cell Phosphatase inhibition of prostatic ACP by Dtartrate, followed by the determination of the serum level of other ACP fractions immunoassay with antibodies specific to certain isoenzymes - electrophoresis aids in detecting metastatic carcinoma other types of cancer and bone diseases evidence of rape Metastatic Carcinoma is the spreading of cancer, but with the Clinical Significant of ACP they can detect and prevent the cancer spreading. Alanine aminotransferase Aspartate aminotransferase Creatine kinase Amylase Lipase Pancreas Promotes the hydrolysis of orthophosphate ester In all body tissues, significantly in RBC’s and platelets found in the prostate gland, high levels are found in semen pH lower than 6.0 inhibition of prostatic ACP , followed by the determination of the serum level of other ACP fractions aids in detecting metastatic carcinoma Other types of cancer and bone disease Evidence of rape Hydrolyzed phosphate esters At 8.6 ÷ 10 42 Chem PPT Flashcards Unit 2 What is ALP used for? Where will you find ALP? What is the ALP isoenzyme that is most susceptible to heat inactivation (heat labile),? What are bone disease patients will have elevated level of ALP? diagnosis of hepatobiliary disease and bone disease associated with increased osteoblastic in liver, bone, kidney, intestines and placenta Bone isoenzyme Osteomalacia Rickets Paget’s disease Why ALP level is high in children? It’s from the osteoblasts during bone growth What are semiautomatic and automatic pipettes These devices are programmed and and dispensers used for? used to simultaneously dispense aliquots into multiple wells. Why are they piston driven? To allow the user to pipette with a few or as many tips as necessary. What is centrifugation? The process of using centrifugal force to separate lighter from heavier parts of a solution, the correct term to describe the force required to separate two phases in a centrifuge is relative centrifugal force (RCF), also called relative centrifugal field. Examples are horizontal head or swinging bucket, fix angle or angle head, ultracentrifuge and axial. What is gravimetry? The process used to measure the mass of a substance using a balance to compare the mass of an unknown to that of a known mass. The comparison is called weighing and the absolute standards with which masses are compared are called weights. What are the types of balances used? Double pan, single pan and the electronic balance. The following are additional questions for slides 19:21-37 What does Alkaline phosphatase (ALP) do and Hydrolyzes phosphate esters; optimum pH = what is its optimum pH? 8.6-10 What are the activators for Alkaline Activators include Mg2+, Co2+ and Mn2+ phosphatase? What are the inhibitors for Alkaline Inhibitors include phosphate, borate, oxalate phosphatase? and cyanide ions How is the Alkaline phosphatase used in Used in the diagnosis of hepatobiliary disease clinical diagnosis? and bone disease associated with increased osteoblastic activity Where Alkaline phosphatase is located? Found significantly in liver, bone, kidney, intestines and placenta 43 Chem PPT Flashcards Unit 2 Does the bone isoenzymes of Alkaline phosphatase (ALP) tolerate to heat? How does the bone isoenzymes Alkaline phosphatase (ALP) influence in the person with bone disease? What is the outbreak of Alkaline Phosphatase (ALP) in children? What is the B. Liver isoenzyme? How does the B.Liver isoenzyme migrate on electrophoresis? What is the outcome of B.Liver isoenzyme in person with hepatobiliary? What is the next type of isoenzymes Alkaline phosphatase (ALP)? How does the C.Intestinal isoenzyme migrate on electrophoresis? What is the D. Placental isoenzyme? What period does the D.Placental isoenzyme have a higher concentration? What is the optimum temperature for D.Placental isoenzyme? What is the last type of Alkaline phosphatase (ALP)? What is the carcinoplacental Alkaline phosphatase? What is the optimum temperature for carcinoplacental Alkaline phosphatase? What is the method used to Measure of Alkaline phosphatase (ALP) activity? What is the substrate used in Bessey-LowryBrock-methods? What are the requirement cofactors in BesseyLowry-Brock-methods? What is the time window for Serum to be analyzed Measuring of Alkaline phosphatase (ALP) activity? What are the substances should be voided in Measurement of Alkaline phosphatase (ALP) activity? Bone isoenzyme; The most susceptible to heat inactivation (heat labile) Elevated in persons with bone disease a) Osteomalacia b) Rickets c) Paget’s disease (osteitis deformans) High in children; Alkaline phosphatase (ALP) from osteoblasts during bone growth It is one of the Five type isoenzymes of Alkaline phosphatase (ALP). The most rapidly moving isoenzyme in electrophoresis Greatly elevated in persons with hepatobiliary obstruction C. Intestinal isoenzyme The slowest moving isoenzyme in electrophoresis D.Placental isoenzymes is belonging to Alkaline phosphatase (ALP) group. Becomes elevated between the 16th and 20th weeks of pregnancy. The most heat stable (65°C) E. Regan isoenzyme An abnormal Alkaline Phosphatase (ALP); A carcinoplacental Alkaline phosphatase (ALP) that has similar properties to the placental isoenzyme heat stable (65°C) Bessey-Lowry-Brock - methods p-nitrophenylphosphate (PNPP) Required cofactors: Mg+2 Zn+2 Serum (analyzed within 4 hours after collection) is preferred or heparinized plasma EDTA, citrate and oxalate plasma must be avoided 44 Chem PPT Flashcards Unit 2 Does the concentration of Alkaline phosphatase (ALP) in serum increase at refrigerated temperature? What should the frozen Alkaline phosphatase (ALP) be treated? Does hemolysis increase results in Alkaline phosphatase activity? What is the most common method to differentiate Alkaline Phosphatase (ALP) isoenzymes? How does Alkaline phosphatase (ALP) be placed on Electrophoresis? What substance will improve the separation of bone ALP and liver isoenzymes on Electrophoresis? What residues must be dropped off bone ALP and liver ALP on Electrophoresis? Why should the terminal sialic acid residues be removed off Electrophoresis? How does intestinal Alkaline phosphatase (ALP) be confirmed in serum? Is intestinal Alkaline phosphatase (ALP) resistant to neuraminidase? What is the second method to differentiate Alkaline phosphatase (ALP) isoenzymes? Does Alkaline phosphatase (ALP) increase during the pregnancy? What is the concentration of Alkaline phosphatase (ALP) in hepatitis and cirrhosis condition? Does Alkaline phosphatase (ALP) increase in person with bone disease? What will be happened to Alkaline phosphatase (ALP) in hyperthyroidism case? How concentration of Alkaline phosphatase (ALP) in diabetes mellitus case? What are the defintion for amiotransferases/(aminotransaminases)? Alkaline phosphatase (ALP) in serum stored at refrigerated temperature increases slowly (2%/day) Frozen samples should be thawed 18-24 hours at room temperature Hemolysis falsely increases results Electrophoresis Order of anodal migration: 1) Liver ALP 2) Bone ALP 3) Placenta / Regan ALP 4) Intestinal ALP Pre-treatment with neuramidase for 15 minutes at 37°C improves separation of bone and liver isoenzymes Removes the terminal sialic acid residues Sialic acid residues of bone ALP are more attached than liver ALP, thus reducing mobility Overnight incubation of serum with neuraminidase is used to confirm presence of intestinal Alkaline phosphatase (ALP) Intestinal Alkaline phosphatase (ALP) is neuraminidase-resistant Stability to denaturation by heat or chemical Elevation during the 3rd trimester of pregnancy Elevation in hepatitis and cirrhosis Elevation in bone diseases with osteoblastic activity Elevation in hyperthyroidism Elevation in diabetes mellitus a) Aspartate Transferase (Transaminase) – AST b) Serum Glutamate Oxaloacetate Transaminase –SGOT 45 Chem PPT Flashcards Unit 2 How does the chemical reaction happened on Aspartate Transferase (AST)? What is the first measurement of Aspartate Transferase (AST) activity? Transfers an amino group between as aspartate and keto acids The reaction with dinitrophenylhydrazine (DNPH) couples color reagent with keto acid product (Rietmann Frankel method) What is the second measurement of Aspartate The reaction with diazonium salts couples the Transferase (AST) activity? salt with the keto acid product and forms a color (Babson) What is the third measurement of Aspartate The coupled enzyme assay (Karmen method) Transferase (AST) activity? involves NADH, malate dehydrogenase and keto acid to form NAD. Malate dehydrogenase catalyzes the oxidation of oxaloacetate to malate in the indicator reaction. What is the optimum temperature for Aspartate AST is stable in refrigerated temperature or Transferase (AST)? frozen samples What are the acceptable reagents in collection Serum or plasma collected with heparin, Serum or plasma Aspartate Transferase (AST)? EDTA, citrate or oxalate is acceptable. What substance is added to the Aspartate Stability can be further enhanced by adding Ptransferase (AST) specimen for stability? 5’-P (pyridoxal-5’-phosphate) to the specimen Where are Aspartate Transferase (AST) AST is present in cardiac tissue, liver, skeletal located? muscles and RBC’s Should Aspartate Transferase (AST) hemolysis Hemolyzed specimens must be avoided specimens be avoided? Does the alcohol affect Aspartate transferase Alcohol lowers AST values. (AST)? How many hours after onset of Myocardial Elevated in: infarction will increase the Aspartate a) Myocardial infarction transferase (AST)? b) Increases 6-8 hours after onset of pain How fast Aspartate transferase (AST) will be Elevated in: elevated in Viral hepatitis? a) Viral hepatitis b) 100-fold increase Does Aspartate transferase (AST) increase its Elevated in Skeletal muscle diseases like concentration in Skeletal muscle diseases? Polymyositis Rhabdomyolysis Duchenne muscular dystrophy Does Aspartate transferase (AST) affect Liver Elevated in: disease? Liver hypoxia What will be happened to the concentration of Elevated in: Aspartate transferase (AST) in strenuous Strenuous physical activity physical activity? What is the Aspartate transferase (AST) AST tends to be higher in infants and children concentration in children? than adults How does Aspartate transferase (AST) be Adult males exhibit higher AST activities than classified in adult males and adult females? adult females 46 Chem PPT Flashcards Unit 2 What are 5 clinical significance of ALP? What does AST stand for? What does SGOT stand for? what do AST and SGOT do? what are 3 major approaches involved in the measurement of AST activity? AST is stable at what temperature? What specimen collection is needed for the measurement of AST? What can you add to the specimen for AST so it can be more stable? Where is AST present in the body? What must be avoided in a specimen collected for AST measurement? What lowers the AST values? What are the clinical significance of AST? 1) elevation during the 3rd trimester of pregnancy 2) elevation in hepatitis and cirrhosis 3) elevation in bone diseases with osteoblastic activity 4) elevation in hyperthyroidism 5) elevation in diabetes mellitus Aspartate Transferase Serum Glutamate Oxaloacetate transminase It transfers an amino group between an aspartate and keto acids. L-aspartate + α-ketoglutarate AST oxaloacetate + L-glutamate 1. The reaction with dinitrophenylhydrazine (DNPH) couples color reagent with keto acid product (Rietmann Frankel method) 2. The reaction with diazonium salts couples the salt with the keto acid product and forms a color (Babson) 3. The coupled enzyme assay (Karmen method) involves NADH, malate dehydrogenase and keto acid to form NAD. Malate dehydrogenase catalyzes the oxidation of oxaloacetate to malate in the indicator reaction. At refrigeration or frozen temperature. Serum or plasma collected with heparin, EDTA, citrate or oxalate is acceptable. Stability can be further enhanced by adding P5’-P (pyridoxal-5’-phosphate) to the specimen. AST is present in cardiac tissue, liver, skeletal muscles and RBC’s. Hemolyzed specimens must be avoided. Alcohol AST is elevated in: 1) Myocardial infarction * Increases 6-8 hours after onset of pain 2) Viral hepatitis * 100-fold increase 3) Skeletal muscle disease * Polymyositis * Rhabdomyolysis * Duchenne muscular dystrophy 47 Chem PPT Flashcards Unit 2 What is a micropipettes ? Pipettes come in different sizes? What is the purpose of a pipette ? What is the mouthpiece of the pipette? What is the calibration lines of a pipette? What is Volume of the pipette ? What is the T.D of the pipette? What is the T. C of the pipette Why must a distinction between T.D and T.C pipettes be made ? What is T.D calibrated with ? What is T.C glassware calibrated with ? What is the meniscus ? What is centrifugation ? What is gravimetric ? What is a Double-pan, single-pan and electronic balances A hallow glass tube used for measuring small volumes of liquid in microliters and transfer of liquid from one source to anothere Yes from single piece glass pipettes to more complex adjustable or electronic pipettes for various purposes with differing levels of accuracy and precision To draw up liquid for the purpose of measuring and transferring a specific volume of liquid The end of the pipette to which suction is applied to draw up liquid into the pipette Marks on the stem of the pipette to show the point where liquid must be drawn to give a specific volume Stated in millimeters example inscription may read 10ml in 1/10 ml and the pipette is graduated in 1/10 ml increments allowing it to be used to measure volumes up to 10 ml “To deliver “pipettes designed to deliver a specific volume of fluid “To contain “ pipettes designed to contain a certain volume of fluid Because there may be a difference between the volume a pipette will contain and a volume it will deliver Distilled or deionized water Mercury A crescent shaped structure appearing at the surface of a liquid column it has the appearance of a contact lens The process of using centrifugal force to separate the lighter portion of a solution mixture or suspension from heavier portions. The process used to measure the mass of a substance Types of balances What are the Isoenzymes of CK? CK1 or CKBB CK2 or CKMB CK3 or CKMM CK- Mt Macro- CK Where is found CK1? brain and nerve tissues Where is found Ck2 in body? At which level Ck2 is elevated and return to normal in MI? In cardiac muscles. levels rise within 4-6 hours, peak at 12-24 hours and return to normal within 48-72 hours 48 Chem PPT Flashcards Unit 2 Located between the inner and outer membranes of mitochondria, and it constitutes up to 15% of total CK activity Located on chromosome 15 How to measure CK by ion-exchange involves an anion exchange resin at a pH 8.0 chromatography? isoenzymes have different charges and can be selectively eluted How to measure CK by immunoassay? involves antisera employed against certain subunits of each isoenzyme How to measure CK by Tanzer-Gilvarg assay? involves coupling with pyruvate kinase and lactate dehydrogenase to produce a change in absorbance measured spectrophotometrically. How to measure CK by Oliver-Rosalki assay? involves coupling with hexokinase and G6PD, in which creatine is produced from creatine phosphate Which are the Clinical Significance of CK? Increased in: -Myocardial infarction -Progressive Muscular Dystrophy (Duchenne type) -hypothyroidism -vigorous muscular activity (cerebrovascular accidents, stroke) -repeated intramuscular injections -drugs such as statins, fibrates, anti-retrovirals and angiotensin II receptor antagonists Why should Avoid hemolysis in Measurement Adenylate kinase, ATP and G6P/glucose-6of CK activity? phosphate liberated from RBCs may affect the lag phase and may cause side reactions The following are some additional questions on slides 38-54 Where is found CK-Mt? In what health condition/disease, the AST level found to be decreased ? What does alanine aminotransferases? What is te required coenzyme for full catalytic activity of ALT? How long can the sample being reserved What is ALT:AST ratio (De Ritis ratio)used for? What is ALT:AST ratio increased in? What is ALT:AST ratio decreased in? - Autoimmune hepatitis - Cholestasis - Cirrhosis - Alcohol liver disease catalyzes the transfer of an amino group from alanine to α-ketoglutarate with the formation of glutamate and pyruvate Pyridoxal-5’-phosphate (P-5’-P) samples stored at room temperature are stable for 3 days, 1 week if refrigerated determine the etiology of hepatocellular disease infectious (viral) hepatitis severe liver disease with necrosis (alcoholic hepatitis, cirrhosis, hepatocellular carcinoma) 49 Chem PPT Flashcards Unit 2 What enzyme Catalyzes the reversible phosphorylation of creatine by ATP What is CREATINE PHOSPHOKINASE (CPK) or CREATINE KINASE (CK) What are the isoenzymes of CK? What appears in in brain damage or nerve tissues? Where is CK2 located? What would be the optimal testing period for CKMB? Creatine kinase a dimer that is composed of two subunits: Bproduct and M-product - CK1 or CKBB - CK2 or CKMB - CK3 or CKMM CK1 or CKBB Heart muscle followingh MI, levels rise within 4-6 hours, peak at 12-24 hours and return to normal within 48-72 hours What type of CK will be use as an indicative of - CK2 or CKMB iIschemic heart disease ? What is the indicative of myocardial damage? levels is >6% What enzyme is majorly found in striated and CK3 or CKMM cardiac muscle and in normal serum? What will CKMM find to be elevated in? hypothyroiidism and intramuscular injections Where will CK-Mt find in? inner and outer membranes of mitochondria, and it constitutes up to 15% of total CK activity What can be used in Measurement of CK - Electrophoresis (agarose, cellulose activity acetate) - Ion-exchange chromatography - Immunoassay - Tanzer-Gilvarg assay (coulormetric method) - Oliver-Rosalki assay How to reserve CK for accurate result? - Refrigerated or frozen protected from light - Addition of cysteine 2+ What substance is required as an activator for Mg full enzyme activity? In what condition would CK level increased? - Myocardial infarction - Progressive Muscular Dystrophy - Hypothyroidism - vigorous muscular activity (cerebrovascular accidents, stroke) - repeated intramuscular injections - drugs such as statins, fibrates, antiretrovirals and angiotensin II receptor antagonists 50 Chem PPT Flashcards Unit 2 What Catalyzes the conversion of lactate to pyruvate at pH 8.8-9.8 and pyruvate to lactate at 7.4-7.8, mediated by NAD? Lactate dehydrogenase (LD/LDH) What does LD stand for? What is the end product of LACTATE DEHYDROGENASE (LD/ LDH)? Lactate Dehydrogenase pyruvate + NADH + H+ Which are the Isoenzymes of LDH? LD1 (HHHH; H4) LD2 (HHHM; H3M) LD3 (HHMM; H2M2) LD4 (HMMM; HM3) LD5 (MMMM; M4) predominantly in heart muscle and RBC’s localization is similar to LD1, but also found in the kidneys. Where is found LD1 HHHH;H4 in body? Where is found LD2 HHHM;H3M? The Isoenzyme LD3 (HHMM;h2M2) is found where ? The Isoenzyme LD3 (HHMM;h2M2) accounts for what percentage of total LD? The Isoenzyme LD4 (HMMM; HM3) is found where ? The Isoenzyme LD4 (HMMM; HM3) accounts for what percentage of total LD? LD5 (MMMM; M4) is similar to? Based on the detection of NADH the Wacker method uses? Based on the detection of NADH the Wrobleuski-Ladue method employs what? For measurement of Total LDH activity, why is serum the preferred specimen ? Measurement of Total LDH activity avoids what? For measurement of Total LDH activity, LD4 and LD5 can be stored at room temperature for how many days? What is the normal LD1:LD2 ratio ? After MI, LD1 is > than LD2 (“flipped pattern”). Also observed in what? Immuno-inhibition for the measurement of LD1 activity involves what? Clinical Significance of LD is used for diagnosis of what? lymphocytes, spleen and pancreas 22% Liver and Skeletal muscles 10% LD4 in both localization and portion of total the lactate-to-pyruvate reaction with the formation of NADH the reverse reaction of the Wacker method and measures the decrease in absorbance as NADH is consumed. -heparinized plasma also acceptable -oxalate has inhibitory effect on the enzyme Hemolysis 2-3 days 0.45-0.74 Hemolyzed specimens an antibody that binds all other isoforms, leaving LD1 to be assayed by chemical reaction Cardiac, hepatic, skeletal muscles and renal disease 51 Chem PPT Flashcards Unit 2 LD is elevated in association with what diseases ? What are two clinical significances of LD1 and LD2 when elevated? What are three clinical significances of LD3 when elevated? What are two clinical significances of LD4 and LD5 when elevated? The LD isoenzyme pattern in renal disease is very similar to a normal pattern except for the higher _____________? Define Diagnostic Window. When does CK activity increase? When does CK activity peak? When does CK activity return to normal? When does AST activity increase? When does AST activity peak? When does AST activity return to normal? When does LD activity increase? When does LD activity peak? How long does LD activity remain elevated? What does AMI stand for? What is a myoglobin? How long does myoglobin take to increase after infarction? How long does myoglobin take to double its initial volume after infarction? When does myoglobin peak? When does myoglobin return to normal? What is myoglobin used in conjunction with to assess AMI? What is Troponin? What are the 3 types of Troponin? -Pernicious anemia -Viral hepatitis -Cirrhosis -Crush injuries -Renal disease Hemolytic anemia Myocardial infarction (MI) Pulmonary edema Pulmonary infarction Pancreatitis Liver disease Skeletal muscle disease Absolute values The interval of time after an episode of injury during which plasma concentrations of the marker are increased, thereby demonstrating the occurrence of injury 4-6 hours after the symptoms 12-24 hours 48-72 hours 6-8 hours after the symptoms 24-46 hours 4th of 5th day 8-12 hours after the symptoms 48-60 hours 10-14 days Acute Myocardial Infarction A heme protein that can bind oxygen reversibly found in cardiac and striated muscles 1-3 hours 1-2 hours 5-12 hours 18-30 hours Troponin and CK-MB A group of three proteins that function in muscle contraction by binding to the thin filaments of cardiac and skeletal muscles Troponin T (TnT) Troponin I (Tn I) Troponin C (TnC) 52 Chem PPT Flashcards Unit 2 When does Cardiac troponin I (cTn I) increase after an AMI? How long does Cardiac troponin I (cTn I) remain elevated after an AMI? When is a serial quantification of Cardiac troponin I (cTn I) necessary after an AMI? Where is Cardiac troponin T (cTnT) found in the body? What is GAMMA GLUTAMYL TRANSFERASE (GGT)? What is an example of tissues containing significant amounts of GGT (descending order of activity per gram of tissue) ? a. Kidney b. Liver c. Pancreas d. Intestines All of the above How is GGT activity measured? a. Szasz Method b. Nonhemolyzed serum Both A and B How is GGT activity stored? List the Clinical Significance of GGT: a. primarily used as a marker for the diagnosis of liver related disorders (intrahepatic or post hepatic obstruction b. detection of alcoholism and monitoring of alcohol intake c. urine contains significant amount of GGT d. elevated also in serum of patients receiving anticonvulsant drugs such as phenytoin and phenobarbital. e. All of the above Between male and female organism, who shows the higher GGT activities? GGT values are lowest in adolescents and rise steadily throughout life: a. True b. False 4-8 hours 3-5 days 3-6 hours 6-9 hours 12-24 hours interval cTnT is found in regenerating and diseased skeletal muscle expressed in small quantities GGT is an amino transferase that transfers a terminal gamma-glutamyl from one compound to an acceptor compound (transpeptidation) E C Stable for at least one month at 4°C and for one year at -20°C. E Male A 53 Chem PPT Flashcards Unit 2 What does it usually mean when GGT and ALP enzymes are elevated and when GGT is normal but ALP is high? What is Gamma Glutamyl Transferase (GGT)? What does GGT do? What contains a significant amount of GGT? Name some tissues that contain GGT in descending order of activity per gram of tissue. What is used for the measurement of GGT? What is the preferred specimen for GGT? What can decrease GGT”s activity by 10%15%? In what temperature can GGT be stable in and for how long? What diagnosis is GGT markers used for? What contains significant amounts of GGT? What can the GGT assays detect? In what other patients can GGT be elevated? What are some clinical significance of GGT? Is GGT higher in males or females? GGT values are lowest in 1) _____? and 2) _____? steadily throughout life. What are GGT levels often examined with? What is suspected if both enzymes (GGT and ALP) are elevated? If GGT is normal, and ALP is high then what is suspected? What is Amylase (AMS)? What is the optimum PH of AMS? What is and what does AMS do? If both enzymes are elevated, liver disorder is suspected; If GGT is normal, and ALP is high, suggestive of bone disease Is an amino transferase Transfers a terminal gamma-glutamyl from one compound to an acceptor compound (transpeptidation). Tissues 1) Kidney (proximal renal tubule) 2) Liver 3) Pancreas 4) Intestines Szasz Method *substrate *gamma-Glutamyle-p-nitroanilide Nonhemolyzed serum is the preferred specimen, but EDTA plasma has also been used. Heparin may produce turbidity; citrate, oxalate and fluoride. Stable for at least one month at 4°C and for one year at -20°C. Liver related disorders (intrahepatic or post hepatic obstruction). Urine Alcoholism and monitoring of alcohol intake. In serum of patients receving acticonvulsant drugs such as phenytoin and Phenobarbital. 1) Acute pancreatitis 2) Diabetes mellitus (in relation to triglycerides increased) In males (do to the contribution of GGT from the prostate gland) 1) adolescents 2) rise ALP Liver disorder Suggestive of bone disease It is a digestive enzyme 6.9-7.0 a hydrolase that catalyzes the breakdown of starch and glycogen producing products consists of glucose, maltose and dextrins. 54 Chem PPT Flashcards Unit 2 AMS is a metalloenzyme that requires what as a cofactor? AMS is the _____? In size. What are the mist affective activators of AMS? Ca2+ Smallest Chloride and bromide The only plasma enzyme physiologically found Amylase AMS in urine is? What are the 2 forms of AMS 1) P-type (pancreas) = ptyalin 2) S-type (salivary glands) = amylopsin What are 5 measurements of AMS activity? Amyloclastic method *measures amylase activity by following the decrease is substrate concentration *substrate = starch 2. Saccharogenic method *measures the amount of reducing sugars produced by the hydrolysis of starch by the usual glucose methods 3. Chronometric method *measures the time required for AMS to hydrolyzed completely all the starch present in a reaction mixture. 4. Amylometric method *measures the amount of starch hydrolyzed in a fixed period of time using the intensity of the blue starch iodine color. 5. Coupled-enzyme methods *measure change in absorbance of NAD. *AMS acts on maltopentose to produce maltose that is then reduced to form ATP. This reaction is the coupled with NAD. When is the end point, in the chronometric When there is absence of any substrate capable method, reached? of forming the blue starch iodine color. What are some clinical significance of AMS? 1) Acute pancreatitis 2) Salivary gland lesion 3) Opiates medication In acute pancreatitis, when do AMS levels 5-8 hours after the onset of attack, peak at 12rise? 72 hours, and then declines to normal in 3-5 days. What are some salivary gland lesions? 1) Mumps 2) Parotidis Opiates medication causes pancreatic Constrict sphincters to do what? What is Macroamylasemia? An asymptomatic condition which results when the amylase molecule and immunoglobulins (IgG) combine to form a complex. 55 Chem PPT Flashcards Unit 2 The complex is too large to be filtered across the? The lack of 1) ___ ___? leads to an 2) ____? serum amylase and 3) _____? Urine amylase. What is evaluated using the ACCR (amylase: creatinine clearance ratio?)? What is ACCR? Macroamylasemia will show decreased urine amylase wit? In what is ACCR increased? What is Lipase (LPS) LPS is filtered by what? LPS is totally reabsorbed by the? What does LPS do? What is used for the measurements of LPs activity? What is the preferred specimen for LPS assays? What is the stability of LPS and at what temperatures? What causes a reduction in lipase activity? What increases lipase activity? What are some clinical significance in LPS? Glomerulus 1) Renal clearance 2) Increased 3) Decreased Macroamylasemia ACCR is the ratio of urinary clearance of amylase to urinary clearance of creatinine, expressed in %. Low ACCR In acute pancreatitis A digestive enzyme secreted by the pancreas. The glomerulus The renal tubules, thus is not physiologically detected in urine. It catalyzes the hydrolysis of ester bonds in triglycerides to produce fatty acids and 2acylglycerol. *Generally, Titrimetric and Turbidimetric methods ~ Cherry Crandall ~ Tietz Templaton Substrate = olive oil Cofactor = colipase Serum 1 week at room temperature 3weeks refrigerated 5 months frozen repeated freezing and thawing should be avoided 3. Lipemic specimens 4. Opiates and morphine 1. Acute pancreatitis Lipase rises within 4-8 hours, peaks at about 24 hours, and decreases within 7-14 days. 2. Pancreatic duct obstruction 3. Tumors of the pancreas 4. Renal insufficiency 56 Chem PPT Flashcards Unit 2 From the graph below, the red line rises within 4-8 hours and peaks at about 24 hours, and decreases within 7-14 days, what is this digestive enzyme? Lipase The graph below indicates that the black line Amylase rise 5-8 hours after the onset of attack, peak at 12-72 hours, and then declines to normal in 3-5 days, what is this digestive enzyme? What do you call the enzyme synthesized by the liver that hydrolyzes the esters of choline? What do you call an enzyme that is also known as “pseudo-cholinesterase”? What does Acetylcholinesterase use as a substrate? Where is Acetylcholinesterase found in the body? a. RBC, Spleen b. Gray matter, nerve endings c. A and B d. Stomach and Heart Acetylcholinesterase is the false cholinesterase or WBC cholinesterase. Evaluate this statement. True or False Psuedocholinesterase uses what kind of substrate? Where is Psudeocholinesterase found in the body? a. serum, liver b. pancreas, heart c. gray matter d. A and B CHOLINESTERASE (CHS) CHOLINESTERASE (CHS) Acetlycholine C. False Butyryl esters (butyrylcholine) D. A and B 57 Chem PPT Flashcards Unit 2 Pusedocholinesterase has other reference names. Which of these is false. a. serum cholinesterase (SChE) b. or acylcholine acylhydrolase c. butyrylcholinesterase, choline esterase II d. acetylcholinesterase Manometric techniques measure liberated ____________ from the formation of acetic acid. a. Carbon Dioxide b. Carbon Monoxide c. Phosphate Dioxin d. Methane Gas Electrometric techniques determine enzyme activity by measuring the ____ decrease resulting in the liberation of acetic acid. a. Salt b. Base c. pH d. Aerosol In the Ellman technique the substrate is a _______ ester that produces a ________, which reacts with a disulfide to form a colored compound. a. Butryl, Butryl b. Thiol, thiol c. Glycol, glycol d. Menthol, menthol __________ is a commonly used substrate for measuring serum cholinesterase activity. a. Psuedocholine b. Butrylcholine c. Acetylcholine d. Propionylthiocholine The Succinyldithiocholine method uses Serum or heparinized plasma only. The method is inhibited by__________. a. Oxalate b. Fluoride c. Citrate d. All the above D. A C B D D 58 Chem PPT Flashcards Unit 2 PChe is stable for several weeks in refrigerated samples; __ years in frozen serum but only up to __ month(s) in frozen plasma a. 3, 1 b. 2, 2 c. 4, 2 c. 2, 6 When PChe is decreased it is clinically significant among other factors for a. organic phosphorus insecticide poisoning b. prolonged apnea after succinylcholine administration during surgery c. hepatocellular disease, starvation d. All the above _______ is an oxidoreductase that catalyzes the oxidation of glucose-6-phosphate to 6phosphogluconate, which is an important step in the pentose-phosphate shunt in glucose metabolism. Name key organs where G6PD is found: a. Adrenal Glands, Thymus b. RBC’s, Lymph Nodes c. Stomach, Pancreas d. A and B G6PD functions to maintain NADPH in a reduced form to protect hemoglobin from oxidation and prevent RBC hemolysis. True or False? a. True b. False The activity of G6PD is by the formation of NADPH which then is measured mass spectometrically. True or False a. True b. False G6PD is increased in Myocardial Infarction and Megaloblastic Anemia. True or False a. True b. False In Latinos G6PD is a common inherited sexlinked trait. True or False. a. True b.False A D G6PD D A B A A 59 Chem PPT Flashcards Unit 2 5’-NTP becomes elevated as a result of liver disease. True or False a. True b. False 5’-NTP in _______ levels are more sensitive to liver cancer. a. Serum b. Plasma c. A and B d. blood The lab wants to keep a sample stable for 5’NTP. What is the longest temperature and time that it can be kept. a. 4 days at 4 degrees centigrade b. 2 hours at room temperature c. 4 months at minus 20 degrees centigrade d. None of the above Lipoprotein-Associated Phospholipase A2 is a _______ risk marker. a. Cardiovascular b. Endocrine c. Skeletal Muscular System d. None of the above Which cells produce Lipoprotein-Associated Phospholipase A2 a. Monocytes b. Macrophages c. Mast Cells d. All of the Above Lipoprotein-Associated Phospholipase A2 is used in detecting atherosclerotic lesions, especially in complex plaque prone to rupture. True or False a. True b. False Can increased levels of Lipoprotein-Associated Phospholipase A2 be associated with future coronary and cerebrovascular events? a. Yes b. No Lp-PLA2 can measured by the ELISA method and the Immunoturbidimetric method. True or False A. True B. False A A C A D A A A 60 Chem PPT Flashcards Unit 2 Should EDTA plasma be used as a recommended sample? a. Yes b. No Myeloperoxidase is released in circulation typically with inflammation. True or False a. True b. False A Define Cancer. it is a term used for diseases in which abnormal cells divide without control and are able to invade other tissues. It can spread to other parts of the body through the blood and lymph systems. Is a substance produced by a tumor or by the host in response to a tumor, which is used to differentiate the tumor from normal tissue, or to detect the presence of a tumor based on measurements in the blood or secretions It can be used for:-For diagnosis, prognosis and prediction For monitoring the effects of therapy -as targets for localization and therapy It is a useful approach to evaluating multiple tests for the same analyte or multiple markers of the same type of cancer Alkaline Phosphatase Lactate Dehydrogenase Neuron-Specific Enolase Prostatic Acid Phosphatase Prostate-Specific Antigen Urokinase-Plasminogen Activator System Cathepsins Adrenocorticotropic hormone (ACTH) Calcitonin Human Chorionic Gonadotropin (CG) α-Fetoprotein (AFP) Carcinoembryonic Antigen (CEA) Tissue Polypeptide Antigen (TPA) Tissue Polypeptide Specific Antigen (TPS) CYFRA 21-1 Squamous Cell Carcinoma Antigen (SCCA) -Mucins -CA 125 -CA 15-3 -HE4 -CA 27.29 -OVA1 -Urinary Bladder Tumor Markers -Nuclear Matrix Protein (NMP22) -Bladder Tumor-Associated (BTA) Analytes DefineTumor Marker. What is the use of Tumor Marker? What is Receiver operating characteristic curve (ROC) ? Enzymes as Tumor Markers. Hormones as Tumor Markers. Oncofetal Antigens as tumor markers. Cytokeratins as tumor markers. Carbohydrate Markers as tumor markers. Which are Bladder Cancer Markers? A 61 Chem PPT Flashcards Unit 2 Proteins as tumor markers. Receptors as tumor markers. Genetic and Molecular Markers. Which are the primary sources of Alkaline Phosphatase What can be seen in primary and secondary liver cancer? When does Lactate dehydrogenase release take place? Neuron-Specific Enolase (NSE) associated with which tumors? What is Prostatic Acid Phosphatase (PAP)? How is Prostate-Specific Antigen (PSA) produce? Where is found Prostate-Specific Antigen (PSA)? Which of the greatest clinical use of PSA? Which methods are used to measure PSA? Which are the components mainly used in Urokinase-Plasminogen Activator System? -Soluble Mesothelin-Related Peptides (SMRPs) -Des-y-carboxy prothrombin (PIVKA-II) S-100 Proteins -Thyroglobulin and Antibodies Chromogranins -Estrogen and Progesterone Receptors -Epidermal Growth Factor Receptor Oncogenes:-RAS genes -HER2 -BCR-ABL Tumor-Suppressor Genes:-Retinoblastoma gene -adenomatous polyposis Coli (APC) Gene -BRCA1 and BRCA2 liver, bone and placenta -Elevation of ALP with elevations in 5'nucleotidase or γ-glutamyltransferase -as a result of cell damage tumors of neuroendocrine origin like small cell lung cancer (SCLC), neuroblastoma, pheochromocytoma, carcinoid, medullary carcinoma of the thyroid, melanoma and pancreatic endocrine tumor It is considered to be less sensitive for the detection of early cancer but may prove useful when combined with other markers for improving prostate cancer detection or predicting recurrence after radical prostatectomy. produce exclusively by epithelial cells of the acini and ducts of the prostate gland and widely use to screen, detect and monitory treatment of prostate cancer. concentrations of PSA has been found to correlate with clinical stages of prostate cancer. PSA involves monitoring of definitive treatment for prostate cancer which includes radical prostatectomy, radiation therapy and antiandrogen therapy. Sandwich immunoassays using labels such as enzymes, fluorescence or chemiluminescence 1. Urokinase plasminogen activator (uPA) 2. uPA membrane-bound receptor (uPAR) 3. uPA inhibitors, PAI-1 and PAI-2 62 Chem PPT Flashcards Unit 2 Which is the main activity of UrokinasePlasminogen Activator ? What is the used of Urokinase-Plasminogen Activator System? Which method is used to measure UrokinasePlasminogen Activator System? What is Cathepsin? What happened if Cathepsin level increased? What methods are used to measure Cathepsin concentration? Which gland produced Adrenocorticotropic hormone? elevated What happened if Adrenocorticotropic hormone concentrations of plasma is elevated? Which are cells are responsible to produced Calcitonin? What happened if Calcitonin concentration is elevated? Which cells are produced Human chorionic gonadotropin (CG)? the main activity is the conversion of plasminogen to active plasmin It has been used as a prognostic marker in breast cancer, colorectal cancer, ovarian, renal, hepatocellular, pancreatic, urinary, bladder, lung (adenocarcinoma) and cervical cancers as well as gliomas. measured in the laboratory by the EnzymeLinked Immunosorbent Assay (ELISA) Cathepsin are lysosome on protease enzymes: Cathepsins B, D and L Cathepsin increased levels are demonstrated in breast, colorectal, gastric, lung, prostate carcinoma, gliomas, melanomas and osteoclastomas. Cathepsin concentrations are generally measured in tissue extracts by ELISA or directly in the tissues by immunohistochemistry Adrenocorticotropic hormone produced by corticotropic cells of the anterior pituitary gland Elevated plasma concentration pancreatic, breast, gastric and colon cancer, and benign conditions such as chronic obstructive pulmonary disease, mental depression, obesity, hypertension, diabetes mellitus and stress. It is produced by the C cells of the thyroid in response to increased serum calcium. It inhibits the release of calcium from bone and thus lowers the serum calcium concentration -Elevated concentration is usually associated with medullary carcinoma of the thyroid (MTC) -It is also elevated in patients with carcinoid tumors and cancers of the lung, breast, kidney and liver -It is also elevated in other nonmalignant conditions such as pulmonary disease, pancreatitis, hyperparathyroidism, pernicious anemia, Pagets' disease of bone and pregnancy Human chorionic gonadotropin (CG) is a glycoprotein secreted by the syncytiotrophoblastic cells of the healthy placenta 63 Chem PPT Flashcards Unit 2 What happened if Human chorionic gonadotropin (CG) elevated? What is the use of GC and AFP together? What method is used to measure chorionic gonadotropin? What is Oncofetal antigens? How to work Oncofetal antigens in fetal life? Which are the Oncofetal antigens tumor markers? What happened if α-fetoprotein (AFP) is elevated? α-fetoprotein (AFP) is determined by Which method? What is the other name of Carcinoembryonic Antigen (CEA)? Which is the origin of Cytokeratins? What happened if Tissue polypeptide antigen (TPA) is elevated? What is the use of Tissue polypeptide antigen (TPA)? What is tissue Polypeptide-Specific Antigen ? -Elevated concentrations are seen in pregnancy, trophoblast disease and germ cell tumors -Also elevated in biliary cancer, pancreatic cancer and other cancers including bladder, renal, prostate, liver, colorectal, non-small cell lung, breast and head and neck cancers GC together with α-fetoprotein (AFP) is useful in detecting nonseminomatous testicular tumor measured in the laboratory by a immunometric (sandwich) technique Oncofetal antigens are proteins produced during fetal life -present in high concentration in the sera of fetuses and decrease to low concentrations or disappear after birth -This proteins often reappear in cancer patients, indicating the reactivation of certain genes as a result of the malignant transformation of cells α-fetoprotein (AFP) Carcinoembryonic Antigen (CEA) Elevated AFP and serum bilirubin concentrations (>2 mg/dL) are associated with a decreased survival time Levels are determined by immunometric assay "Gold" antigen Cytokeratins group of proteins that make up the cytoskeletal intermediate filaments of epithelial cells and cells of epithelial origin. Tissue polypeptide antigen (TPA) Elevated serum concentrations are related to the proliferative activity and turnover of cells, allowing it to be used as a proliferation marker. In monitoring of metastatic disease, TPA is useful when comb (ined with CEA and CA 153 in breast cancer, with CEA and CA 19-9 in colon cancer, and with CA 125 in ovarian cancer. TPA may be helpful in the differentiation of cholangiocarcinoma (increased TPA) from hepatocellular carcinoma (in which TPA is not elevated) an antigenic site on cytokeratin 18 that is specifically recognized by the M3 monoclonal antibody 64 Chem PPT Flashcards Unit 2 CYTOKERATINS AS TUMOR MARKERS have been proposed as a specific marker for cell proliferation and is detectable in serum with the use of a _____ _____? CYFRA 21-1 is elevated in all types of _____ _____, although it is most sensitive for nonsmall cell ____ _____. Squamous Cell Carcinoma Antigen (SCCA) is a _______ referred to as tumor associated antigen 4. Squamous Cell Carcinoma Antigen (SCCA) is useful in detecting recurrence of ______ and in monitoring treatment and disease progression CA 15-3 is detected by a _____ ______ _____ against a membrane-enriched extract of the human breast cancer metastatic to liver CA 15-3 elevated concentrations are found in ______ including pancreatic, lung, breast, ovarian, colorectal and liver cancers. CA 27.29 is used for detecting recurrent _____ _____ in patients with stage II or stage III disease and for monitoring response to therapy in patients with stage IV (metastatic) disease CA 125 is a marker for monitoring what? CA 125 is also used to detect ______ or _____ disease in patients who have undergone firstline therapy and would be considered for second-look procedures CA 125 is also elevated in non-_____ carcinoma including pancreatic, lung, breast, colorectal, gastrointestinal tumors and useful in determining the prognosis of patients with endometrial carinoma CA 125 is determined by what? CA 19-9 (sialylated Lexa) a marker for gastrointestinal cancer and is used primarily in patients with _____ _____? CA 19-9 has been approved by the FDA for quantitative measurement in serum and as an aid in monitoring _____ _____ patient Monoclonal immunoglobulin has been used as a marker for multiple ______? Monoclonal paraproteins appear as sharp bands in the _____ region of serum electrophoretic patterns. specific immunoassay lung cancer, lung cancer glycoprotein cancer murine monoclonal antibody malignancies breast cancer epithelial ovarian cancer residual or recurrent ovarian determined by immunoradiometric essay pancreatic carcinoma pancreatic cancer myeloma Globulin 65 Chem PPT Flashcards Unit 2 Bence Jones proteins is what? What type of cancer is detected through cytoscopy or cytology of shed cells using tumor markers like NMP22, complement factor-H (CFH), fibronectin, telomerase, cytokeratins and survivin. Bladder cancer is measured what type of technique? What type of proteins have functions that have been associated with regulating key reactions in the nucleus, such as DNA replication and RNA synthesis What detects the antigen human complement factor-H related protein, which is a variant of human complement factor-H Bladder Tumor Associated analytes functions in the alternative complement pathway by interacting with complement factor C3b to prevent what? _______ is a cell surface glycoprotein express on mesothelial cells, and mesothelin fragments, found in the circulation of patients with mesothelial tumor. Mesothelioma is a rare cancer of the mesothelial surfaces of the pleural and peritoneal cavities or the pericardium that is linked to what? What type of tumor markers are used as Calcium binding proteins for diagnostic histological marker of melanoma and melanoma metastases What type of protein is a family of proteins that are major components of the secretory granules of most neuroendocrine cells Chromogranins is useful in detecting _____ ______ like carcinoid tumor, pheochromocytoma and neuroblastoma Thyroglobulin and antibodies produced by the _____ gland as the precursor to ____ hormone Thyroglobulin and antibodies are used for monitoring patients with a diagnosis of differentiated ____ cancer after thyroid gland ablation. a free monoclonal immunoglobulin light chain in the urine Bladder Cancer fluorescence in situ hybridization (FISH) Nuclear Matrix Protein (NMP22) Bladder Tumor Associated analytes cell lysis Mesothelin asbestos exposure S-100 Proteins Chromogranins neuroendocrine tumors thyroid Thyroid 66 Chem PPT Flashcards Unit 2 What antibodies are used to monitor residual disease and or recurrence? Thyroglobulin and antibodies are measured by what? Estrogen and progesterone receptors are members of the nuclear ____ hormone receptor family and are involved in hormone directed transcriptional activation Estrogen and progesterone receptors are used in tumor markers as indicators of what type of cancer for hormonal therapy? Immunohistochemistry assay is used to measure steroid hormone receptors in what type of tumor tissue specimens? Epidermal Growth Factor Receptor (EGFR) is a prototype of what type of family receptors? What is used as a companion diagnostic to aid in identifying colorectal cancer patients? Prostate Cancer Gene or Antigen3 (PCA3) a molecular test for what? Single-Nucleotide Polymorphisms genes are associated with what? Cell-Free Nucleic Acids are markers for what 2 types of cancer? Creatinine is a diagnostic indicator of what function? What three organs is Creatinine synthesized in? True or False: Creatinine is present in all body fluids and secretions. What is Creatinine a marker of? What reaction is used in Creatinine? The Jaffe reaction of Creatinine has a reaction with what? Creatinine analytical methods tend to lack what? Name two enzymes of Creatinine Antithyroglobulin Immunometric assays and RIA steroid Breast cancer breast tyrosine kinase Epidermal Growth Factor Receptor prostate cancer human disease lung cancer and colorectal cancer Kidney Kidneys Liver Pancreas True Glomerular Filtration Rate (GFR) Jaffe reaction Picrate ion Specificity What are four analytical methodology factors that are used in Creatinine? Enzymatic methods (Fig. 21-1) What type of state is Urea? • Urea is an underestimation of what? • Urea is an outdated indicator of what function? • Creatininase creatinase Hydroxide Wavelength Temperature “Concentration” Azotemic state Glomerular filtration rate Kidney 67 Chem PPT Flashcards Unit 2 What is a chemical method of Urea? What is an enzymatic method of Urea based on? What three types of Urea enzymatic methods approached is used? What does a spectrophotometric approach consist of? What does the biochemistry and physiology of Uric Acid focus on? A clinical significance of Uric Acid that involves, 20-plus inherited disorders of what metabolism? Uric Acid is used as a measurement in management of what? What does Uric Acid help determine on during Hypouricemia? Name two analytical methodology of Uric Acid? Which is more specific, PTA or Uricase? What does HPLC-based methods focus on during Uric Acid? What does reference values of Uric Acid indicate? What are Carbohydrates ? What is a Monosaccharides ? What is an example of a Monosaccharide? What are Oligosaccharides ? Give an example • • Fearon reaction Preliminary hydrolysis of urea with urease Spectrophotometric Dry Chemistry Systems • Specificity Berthelot method and enzymatic assay Urate pool Renal handling of uric acid Purine metabolism Gout Link to underlying conditions Other causes Phosphotungstic acid (PTA) Uricase Uricase Ion-exchange or reversed-phase Gout Purine-containing and purine-free diets •Aldehyde or ketone derivatives of polyhydroxy (more than one -OH group) alcohols composed of carbon, hydrogen, and oxygen in the ratio of 1:2:1 •they serve as structural components in RNA and DNA sugars •considered to be the main source of energy Simple sugars that contain 4-8 carbons and only 1 aldehyde or ketone group. They are reducing sugars with the general formula of Cn(H2O) n that cannot be broken down to simpler substances by acid hydrolysis. Glucose Sometimes referred to as disaccharides which are formed by the interaction of two monosaccharides with the loss of water molecule. Examples are: Maltose → two molecules of glucose ;Lactose → glucose and galactose; Sucrose → glucose and fructose 68 Chem PPT Flashcards Unit 2 Describe Polysaccharides? What is considered the primary energy source for the human body? What are the results of Glucose metabolism? What is Glycogenesis and Glycolysis? What is Hypoglycemia and its symptoms? Describe neuroglycopenia and its characteristics How is a 72-hour test for Hypoglycemia conducted? How to determine a true Hypoglycemia? How does Ethanol produces hypoglycemia? One way to determine an insulin producing pancreatic islet cell tumor is? Carbohydrates formed by the interaction between many units of simple sugars. Examples include starch and glycogen Glucose •energy production by conversion to carbon dioxide and water •storage as glycogen in the liver or as triglycerides in adipose tissue •conversion to keto acids, amino acids or protein Glycogenesis is the conversion of glucose to glycogen and Glycolysis is the conversion of glucose or other hexoses into lactate or pyruvate. Hypoglycemia is a blood glucose concentration below the fasting value (<50 mg/dL or 2.75 mmol/L). Symptoms include trembling, sweating, nausea, rapid pulse, lightheadedness, hunger and upper abdominal discomfort Neuroglycopenia is caused by the lack of glucose supply in the brain. It is characterized by headache, confusion, blurred vision, dizziness, seizures, loss of consciousness and even death. •Fasting hypoglycemia in adults can be monitored by the 72 hour fasting test •symptoms usually begin at plasma glucose concentrations below 55 mg/dL, and impairment of cerebral function begins when glucose is less than 50 mg/dL •the 72 hour fast should be conducted in the hospital •the patient should be allowed a liberal intake of calorie free and caffeine free fluids True hypoglycemia will show an abnormally low value within 12 hours of beginning a fast Ethanol produces hypoglycemia by inhibiting gluconeogenesis, and this inhibition is aggravated by malnutrition (low glycogen stores) in individuals with chronic alcoholism. The demonstration of a low plasma glucose concentration in the presence of a high plasma insulin value 69 Chem PPT Flashcards Unit 2 Name possible causes of Postprandial Hypoglycemia What are some criteria of Whipple's triad overflow blood glucose concentration? What are the Pathophysiological mechanisms that contribute to hypoglycemia in patients with diabetes? Where does the Lactic acid predominantly derived from? What is the Cori cycle ? How can the measurement of pyruvate be useful? What can a lactate-to-pyruvate ratio indicate? Describe Lactic acidosis When testing for carbohydrate metabolism, a deficiency or absence of an enzyme that participates in carbohydrate metabolism may result in what inborn error? Name the 2 sugars of clinical interest that are found in the urine? •drugs •antibodies to insulin or insulin receptor •inborn errors (fructose-1,6- diphosphatase deficiency) •reactive hypoglycemia (functional hypoglycemia) •symptoms known or likely to be caused by hypoglycemia •low glucose when symptoms occur •relief of symptoms when glucose is increased the normal Defective glucose counter regulation (ability to increase glucose, counter to the effect of insulin) unaware of hypoglycemia white skeletal muscle, brain, skin, renal medulla and erythrocytes, and are metabolized in the liver and kidneys The Cori cycle is the conversion of glucose to lactate in the periphery and reconversion of lactate to glucose in the liver Measurement of pyruvate is useful in the evaluation of patients with inborn error of metabolism who have increase serum lactate concentration. Pyruvate is also measured in clinical studies evaluating reperfusion after myocardial ischemia A lactate-to-pyruvate ratio of less than 25 suggests a defect in gluconeogenesis, whereas an increase ratio (<35) indicates reduced intercellular conditions found in hypoxia Lactic acidosis is a lactate concentrations exceeding 5mmol/L with pH less than 7.25. Occurs in 2 clinical settings: •Type A (hypoxic) associated with decreased tissue oxygenation •Type B (metabolic) associated with diabetes mellitus, neoplasia, liver disease, drugs and inborn error of metabolism Accumulation of monosaccharides, which are measured in the urine Glucose and Galactose 70 Chem PPT Flashcards Unit 2 Glucose can be checked by what? Why should urine from infants and children be tested by both the glucose oxidase and copper reduction test? Name the 5 techniques used to separate and identify sugars? Where in the body is glycogen predominantly stored? What is the cause of Glycogen Storage Disease? Lipids are a class of compounds that are soluble in but insoluble in ? Which organic compound can serve as hormones, energy source, assist with ingestion and act as structural components in cell membranes? Name the 6 forms of lipids: What form of lipid is an unsaturated steroid alcohol whose structure is based on the CPPP nucleus? CPPP stands for? Where does absorption of cholesterol mostly occur? Absorption of cholesterol is mediated by what enterocyte protein? In the intestinal mucosal cells, cholesterol is packaged with triglycerides, phospholipids and a large protein, called apolipoprotein (apo) B48, into large lipoprotein particles called? What is the function of the chylomicrons? Cholesterol is synthesized by all cells in the body, but particularly by what organs? Glucose oxidase strips To identify individuals with inborn error of metabolism fermentation optical rotation osazone formation with phenylhydrazine specific chemical test paper or thin layer chromatography Liver and Skeletal muscles Deficiency of a specific enzyme in glycogen metabolism Organic solvents; water Lipids Cholesterol Fatty acids Acylglycerols (Glycerol esters) Sphingolipids Prostaglandins Terpenes Cholesterol Cyclopentanoperhydrophenanthrene In the middle jejunum and the terminal ileum of the small intestines NPC1L1 (Niemann-Pick C1-like1). Chylomicrons Chylomicrons are secreted into the lymph and enter the circulation, where they deliver the absorbed dietary lipid to the liver and peripheral tissues Liver and intestines 71 Chem PPT Flashcards Unit 2 What are the three stages to cholesterol biosynthesis? Cholesterol is esterified to a fatty acid to form a cholesteryl ester by what two enzymes? What happens to cholesterol when it is esterfied? Specialized endocrine cells can use cholesterol for the synthesis of what? How is most cholesterol catabolized? What is referred by the term, essential fatty acids? Name the only 2 fatty acids known to be essential to humans: What is the term that is used for other fatty acids that are sometimes essential under some developmental or disease conditions? What 2 fatty acids are conditionally essential? Where does the fatty acid get metabolized and produced energy by a series of reactions known as β-oxidation? When fatty acid is metabolized it produces energy by a series of reactions, this reaction is called what? What is Krebs cycle? What is the main energy storage molecule in the body? True or False Ketone formation develops from excessive production of acetyl-CoA (ketosis) involvement of acetyl-coenzyme A (CoA) involvement of the microsomal enzyme HMG-CoA ( hydroxy-methyl-glutaryl CoA) reductase a series of oxidation-decarboxylation reactions in the endoplasmic reticulum acylcholesterol acyltransferase (ACAT) lecithin cholestrol acyltransferase (LCAT) It loses its free hydroxyl group and becomes more hydrophobic Steroid hormones Most cholesterol is converted in the liver into bile acids The term "essential fatty acid" refers to fatty acids required for biological processes but does not include the fats that only act as fuel. alpha-linolenic acid (an omega-3 fatty acid) linoleic acid (an omega-6 fatty acid) Conditionally essential docosahexaenoic acid gamma-linolenic acid Mitochondria β-oxidation A common pathway for the final oxidation of nearly all metabolic fuels (carbohydrate, fat or protein) and ultimately results in the production of ATP (adenosine triphosphate) ATP (adenosine triphosphate), True 72 Chem PPT Flashcards Unit 2 True or False In ketone formation, as the body attempts to obtain necessary energy from stored fat, in the absence of an adequate supply of carbohydrate metabolites as in cases of prolonged starvation or when carbohydrate metabolism is impaired (as in diabetes mellitus) What are the forms of ketone bodies? What do you call a three-carbon alcohol that contains a hydroxyl group on each of its carbon and is classified by the number fatty acyl groups present? What is acylglycerol? How many carbons does ACYLGLYCEROLS contain? What do you call an ACYLGLYCEROL that has one fatty acid? What do you call an ACYLGLYCEROL that has two fatty acids? What do you call an ACYLGLYCEROL that has three fatty acids? What type of lipid that constitutes 95% of tissue storage fat and are the predominant form of glyceryl esters found in plasma? Triglycerides from plant sources (corn, sunflower, safflower) are liquid oils at room temperature tend to be enriched with what kind of fatty acid? Triglycerides from animals (ruminants) that are solid at room temperature and tend to have this kind of fatty acid, what is this fatty acid called? Where does dietary triglyceride get digested? After being digested in the duodenum, dietary triglycerides get absorbed where? True acetoacetic acid Β-hydroxybutyric acid acetone ACYLGLYCEROLS (GLYCEROL ESTERS) A three-carbon alcohol that contains a hydroxyl group on each of its carbon and is classified by the number fatty acyl groups present: one fatty acid - monoacylglycerols (monoglycerides); two fatty acids diacylglycerols (diglycerides); and three fatty acids - triacylglycerols (triglycerides)? 3 monoacylglycerols diacylglycerols (diglycerides); triacylglycerols (triglycerides) Triglycerides Unsaturated fatty acids saturated fatty acids Dietary triglycerides are digested in the duodenum Absorbed in the proximal ileum. 73 Chem PPT Flashcards Unit 2 Dietary triglycerides through the action of pancreatic and intestinal lipases and in the presence of bile acids, they are first hydrolyzed to what? Through the action of and intestinal lipases and in the presence of bile acids, they are first hydrolyzed to ____(1)___, ___(2)___,and ___(3)_. After absorption, they are reassembled as triglycerides in the intestinal epithelial cells and then are package with cholesterol and apoB-48 to form ___(4)_____ What do you call the lipoprotein that carries triglycerides to the liver and peripheral cells? ______________are the main metabolic fuel carried by chylomicrons to the liver and peripheral cells. A ________ is a dihydric 18-carbon alcohol, derived from the amino alcohol sphingosine. What form of lipids that have a more general role in cellular interactions and serves as a source of blood group and tumor antigens? What are prostaglandins? What group of physiologically active lipid compounds, which have diverse hormone-like effects in animals and found in almost every tissue in humans and other animals? Prostaglandins are derived enzymatically from? True or False The structural differences between prostaglandins account for their different biological activities. True or False A given prostaglandin may have different and even opposite effects in different tissues. The ability of the same prostaglandin to stimulate a reaction in one tissue and inhibit the same reaction in another tissue is determined by? With their target cells present in the immediate vicinity of the site of their secretion, Prostaglandin acts as what? To glycerol, monoglycerides, and fatty acids. 1) glycerol 2) monoglycerides 3) Fatty acids 4)chylomicrons chylomicrons Triglycerides Sphingolipids Sphingolipids Any of the group of compounds derived from unsaturated 20-carbon fatty acids (primarily arachidonic acid) via the cyclo-oxygenase pathway prostaglandins fatty acids True True The type of receptor which the prostaglandins bind. autocrine or paracrine factors 74 Chem PPT Flashcards Unit 2 How does Prostaglandins differ from endocrine Prostaglandins differ from endocrine hormones hormones? in that they are not produced at a specific site but in many places throughout the human body. What are the two derivatives of prostaglandin? prostacyclins and thromboxanes What derivative of prostaglandin that is Prostacyclins powerful locally acting vasodilators and inhibits the aggregation of blood platelets? Through their role of this prostaglandin Prostacyclins derivative in vasodilation, they are also involved in inflammation. What is this derivative called? Where does Prostacyclins get synthesized? They are synthesized in the walls of blood vessels and serve the physiological function of preventing needless clot formation, as well as regulating the contraction of smooth muscle tissue What derivative of prostaglandins produced by Thromboxanes platelet cells? What Prostaglandin derivatives are vasoconstrictors and facilitate platelet aggregation? What is this polymer consisting of the fivecarbon isoprene unit and include vitamins A, E, and K and the dolichols, which play important roles in protein glycation? _____(1)____ and _____(2)______ are the primary constituents of the essential oils of many types of plants and flowers. Essential oils are used widely as fragrances in perfumery, and in medicine and alternative medicines such as aromatherapy. What are these macromolecular complexes that serve as transport vehicle of insoluble lipids in the plasma? What is the role of the lipoprotein in insoluble lipids in the plasma? What is the appearance of a lipoprotein? What do you call this major protein component that is found on the surface of a lipoprotein? Thromboxanes Terpenes 1)Terpenes 2)terpenoids Lipoprotein Serves as transport vehicle of insoluble lipids in the plasma. They are typically spherical particles with nonpolar neutral lipids (triglycerides and cholesterol esters) in their core and more amphipathic lipids (phospholipids and free cholesterol) at their surface. Apolipoproteins 75 Chem PPT Flashcards Unit 2 What are the categories of lipoprotein? True of False. The larger lipoproteins contain more core lipids, triglycerides and cholesterol esters and are lighter in density and contain a small percentage of protein. True or False In the fasting state, most plasma triglycerides are present in VLDL, but 10 to 12 hours after a meal, most triglycerides are transported on chylomicrons. How much total of plasma cholesterol is carried by LDL? What Lipoprotein contains about 20% to 30% of plasma cholesterol? True or False Lower density corresponds to larger particle and lower protein-to-lipid ratio, while higher density are smaller and have higher proportions of protein In lipoprotein, density is inversely proportional to the protein content and directly proportional to the lipid content and size of the molecule Complete the chart: _(1)_ density = _(2)_ protein content ↑ density = _(3)_ lipid content _(4)_ density = ↓ size of the molecule (smaller) Are the Apolipoproteins; major components of lipoproteins? True or False A. True B. False 1)Chylomicrons 2)Very Low Density Lipoprotein (VLDL) or pre-β-Lipoprotein 3)Intermediate Density Lipoprotein (IDL) 4)Low Density Lipoprotein (LDL) or βLipoprotein 5)High Density Lipoprotein (HDL) or αLipoprotein 6)Lipoprotein (a) [Lp(a)] True False (2 – 6 hours after a meal) carries about 70% of total plasma cholesterol HDL True False (directly proportional to the protein content and inversely proportional to the lipid content and size of the molecule) 1) ↑ 2) ↑ 3) ↓ 4) ↑ A 76 Chem PPT Flashcards Unit 2 Apolilipoproteins function to: A. modulate the activity of enzymes that act on lipoproteins B. maintain the structural integrity of the lipoprotein complex C. facilitate the uptake of lipoprotein by acting as ligands for a specific cellsurface receptors D. All of the above Apo A-1 is not the major protein in HDL. True or False A. True B. False Chylomicrons have what type of Apolipoprotein? A. Apo A-1 B. Apo B-100 C. Apo B-48 D. none of the above Lipoproteins have several pathways. Identify them. A. Exogenous Pathway and the Endogenous Pathway B. Intercellular-Cholesterol Transport Pathway and the Reverse-Cholesterol Transport Pathway C. A and B D. None of the Above The transport of dietary lipids from the intestines to the liver and peripheral cells mediated by: A. Chylomicrons B. RBC’s C. WBC’s D. Adipose Tissues The endogenous pathway’s is transfer _______ derived________ . A. Hepatically, Lipids B. Splenically, Triglycerides C. Kidney, Monoglycerides D. Stomach, Diglycerides D B C C A A 77 Chem PPT Flashcards Unit 2 The endogenous pathway has which mediator lipoprotein? A. Apo A-1 B. Apo B-100 C. Apo B-48 D. all of the above Cells use the cholesterol for several roles. Identify the appropriate role. A. Membrane Biogenesis B. Vesicular Transport C. Osmosis D. Exocytosis Do cells have a surface receptor for cholesterol? A. Yes B. No The Reverse Cholesterol Transport Pathway’s function is to remove excess cellular cholesterol from peripheral cells and return it to the liver for excretion. What is the mediator? A. HDL B. VLDL C. LDL D. chylomicrons Are Coronary Heart Disease, Type V Hyperlipoproteinemia, and Familial hypercholesterolemia clinically significant? A. Yes B. No The Lab has been asked to conduct a total lipid panel. What tests must be run? A. Total Cholesterol B. Triglyceride C. HDL-C D. LDL-C E. All of the above B A A A A E 78