Eustachian tube dysfunction - Derby GP Specialty Training
advertisement

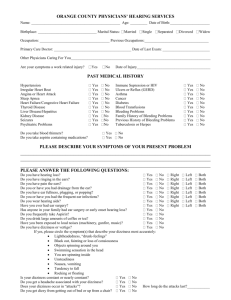
Derby GP Specialty Training Programme E A R S Practical exercise • Get into pairs • Look in each others ears • Draw and label what you see! Normal eardrum Right or left? The normal tympanic membrane should appear •Pearly grey •With a light reflex •Concave •Should be able to make out malleus – looks like an arm 7 6 1 = pars flaccida (=attic) 2 = lat process of malleus 3 = handle of malleus 4 = end of malleus 5 = light reflex 6 = eardrum margin 7 = pars tensa Anterior, posterior, inferior regions Attic – this area is located above the elbow. Anterior – this is the area the elbow is point towards (Face end of patient) Posterior – this is the area opposite the elbow. Inferior – this is the area below the hand. Malleus What are you looking for? • Shape of the eardrum – bulging or retracted • Colour of the eardrum – red (infection), yellow (glue ear), brown (blood), presence of blood vessels (injected?) • Light reflex present or not? (usually absent in bulging ear drums) • Things that should not be there… Case Study 1 2 ½ year old ♂ History Presents with a 2 day history of irritability, runny nose and fever. He’s not been playing as much as usual and today his Mum noticed that he’s been pulling his left ear. He had an ear infection last year and was given some antibiotics, Mum would like the same again please. Examination Irritable. HR 100, RR 22, Temp 37.4ºC HS I+II+0, cap refil <2sec. Chest clear, no signs of respiratory distress Abdo SNT ENT – throat red, right ear nad, left ear – see picture... • What further information would you like to know? • What are your differential diagnoses? • How would you manage him? Who would you see again? • When would you consider referral? • Any advice to prevent further episodes? What else would you like to know? Symptoms More common: In winter Have older siblings At nursery Uses a dummy Parents smoke • • • • • • • Earache or pulling/tugging ear URTI Pain Malaise Fever Irritability Vomiting Signs • Pyrexia • Red, bulging tympanic membrane • May be air-fluid level behind TM • Perforated TM +/or discharge in canal • Possibly hearing loss What are your differential diagnoses? • Otitis Externa • URTI – TM a little red • Acute mastoiditis – swelling, erythema & tenderness over mastoid bone; displacement (downwards & outwards) of pinna • Post auricular adenitis • Referred pain from teeth How would you manage him? • Pain relief & antipyretic – regular paracetamol, ibuprofen • Antibiotics – For most people no or delayed Abx with appropriate explanation or risk vs benefit – Consider if • • • • <2yrs Systemic Sx inc temp >38ºC or vomiting Bilateral AOM Perforated TM with discharge – Amoxicillin (Erythromycin) – Co-amoxiclav (Azithromycin) if Rx failure • Consider admission – systemically unwell • Safety netting – “Needs review if...” • Review at 2-3 weeks if perforated TM When would you consider referral? • 3+ episodes in 6 months or 4+ episodes in 1 year with the absence of disease between episodes • Adults with >2 episodes in a year with suspicion of nasopharyngeal cancer – persistent Sx & signs, cervical lymphadenopathy, unilateral epistaxis Any advice to prevent further episodes? • • • • Eliminate passive smoking Avoid dummies Avoid supine feeding ?pneumococcal vaccinations Case study 2 • Red itchy ear • 40 year old female • 1 week history of an “Itchy Ear”, getting worse • Keen Swimmer • Type 2 Diabetic – on Metformin • No other medical history of note Red, Itchy Ear On Examination • BMI 35 • Swollen Ear Canal with erythema • No discharge, some debris • Pain on moving pinna • Nil else of note Red, Itchy Ear Otitis Externa • Often occurs after trauma – e.g. Scratching, ear cleaning, swimming • Symptoms – Pain (Severe, also on pinna movement), – Discharge (May be offensive) • Signs – Swollen ear Canal +/- Discharge / Debris – May have swollen pre/post auricular lymph glands Otitis Externa • Management – Aural Toilet (unless mild case) – ABX Ear Drops (Gentamicin 0.3%) – +/- steroid if eczematous (Gentisone HC) – May need strong analgesia, and wick – If refractory , need to swab - may be candida or aspergillus (Clotrimazole) Otitis Externa • Prevention – No cotton buds! – Keep ears dry • If mild itchiness / eczema • Short course steroid drops (Prednisolone 0.5% TDS) Case Study 3 • History: 28 year old woman with known anxiety problems presented with ear popping and occasional pain for the past 3 weeks following a cold. She has no history of ear problems and recently had a relaxing holiday in Turkey. She is very concerned and thinks she is becoming deaf. She is otherwise well and apyrexial. • What further information would you like to know as the GP? • What do you think is going on? Can you formulate a differential list? • Can you think of a simple test to aid diagnosis? • How are you going to manage this patient? • When will you think about referring for ENT opinion? Eustachian tube dysfunction Symptoms: Muffled hearing, dull hearing, ear popping, ear pain, ringing, dizziness. Causes: Blocked Eustachian tube – ENT infections, glue ear, allergies, blockages, air travel. Test: Look at the ear drum whilst asking the patient to perform valsalva manoeuvre, if Eustachian tube dysfunction, the ear drum moves very little. Treatment: Often no treatement is needed. Antihistamine tablets, decongestant nasal sprays or drops may help. Referral: When symptoms persist despite treatment. Case Study 4 • History: 57 year old man who works as a football manager came to see you because he thinks he needs a hearing aid. He has noticed whistling and ringing noise in his right ear for the past 8 months, he put this down to occupational related hearing changes. More recently, he has noticed some headache on the right hand side of the head with occasional tingling sensations. He has been to see the football club doctor, who thought he had tinnitus and advised him to come and see you to arrange assessment for a hearing aid. On examination, you cannot appreciate any obvious abnormality. • What are you going to do next? • Can you think of the possible differentials? • What are you worried about? • How will you manage this patient? • When will you think about referring him for ENT opinion? Acoustic neuroma (Schwannoma) Symptoms: Unilateral hearing loss over months, unilateral ringing/buzzing. Occipital pain. Possible facial numbness. Pathology: Slow growing neurofibroma arising from the acoustic nerve, associated with type II neurofibromatosis (especially bilateral cases). Investigations: Audiometry to demonstrate unilateral sensorineural hearing loss. Contrast CT scan. MRI sometimes needed to identify small lesions. Treatment: Conservative – elderly patients or high risk patients due to tumour location. Sterostatic radiosurgery – small/medium tumours Microsurgery – large tumours Referral: Unilateral sensorineural deafness – 2WW referral criteria Case Study 5 • 65 year old man, presented to you with hearing loss on one side. Gradual onset, wife has been telling him that the wax coming out from his ear has been very smelly. He wants some olive oil on prescription because he does not pay for his medications anymore. How will you manage this patient if you see this during the examination? • Cholesteatoma • 9/100,000 • Offensive discharge • Retracted eardrum • Crusty lesion, typically attic • Enzymatic destruction of ossicles or temporal • Urgent referral for surgery Conductive hearing loss Sensorineural hearing loss • Presbyacusis • Greek: old, hearing • Whisper (letters, numbers) • Weber, Rinnes • Pure tone audiometry • 250, 500, 1000, 2000, 4000kHz • http://www.phys.unsw.edu.au/jw/hearing.ht ml • “Mosquito” 17.4kHz • Mild 20-40dB • Moderate 41- 70dB • Severe 71-95dB • Profound >95dB Case study 6 • 52 year old lady presents with 1 week history of dizziness and feels like the room keeps spinning. She feels sick with it and has vomited several times. She also complains of reduced hearing in her left ear. This is what you see on examining her left ear… • What else do you want to know? • What are your differentials? • What investigations do you want to do? • What would your management be? Vertigo BPPV Menieres Viral labyrinthitis/ vestibular neuronitis Duration seconds/mins Minutes to hours >24hrs Assc. Hearing loss N Y N Assc tinnitus N Y N Related to position Y N N Diagnosis History & + Hallpikes History and assc Sx History and duration Refer If not settling for Epleys All cases to confirm Dx If persists>6wk Examination • • • • • • • Ears Cerebellar signs Cranial nerve exam Romberg’s sign Hearing – Webers + Rinnes Nystagmus Hallpike manoeuvre and Epleys Management • BPPV – – – – Self limiting Reassure Physio, reduce alcohol Prochlorperazine/ betahistine • Viral labyrinthitis / vestibular neuronitis – Follows viral URTI – Prochlorperazine/ cyclizine • Menieres – Clusters of attacks of vertigo, nausea, tinnitus, SNHL and fullness in ear. – Give info and support groups – Treat acutely with labyrinthine sedativesprochlorperazine /cyclizine – Mobilize – Consider: Betahistine, low salt diet, vestibular rehab, tinnitus masker, HA – Look out for and treat depression/anxiety Hallpike and Epley manoeuvre Picture Quiz Answers… Bubbles Glomus tumour Acute Otitis Media Otitis Media with retraction Eustachian Tube dysfunction Cholesteatoma Tympanic sclerosis Normal tympanic membrane Safe Anterior Perforation Inferior Perforation Unsafe Posterior Perforation Unsafe Attic Perforation Grommet Otitis Externa This is a Monkey… This is a Bat… This is a Tiger… This plant is called Elephant Ears… Thank you for listening, and now it’s time to go home!