CPT Coding and Why You Care
advertisement

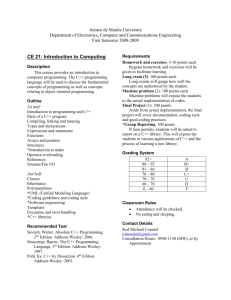
CPT Coding and Why You Care Ted A. Bonebrake, M.D. CPT Coding Current Procedural Terminology System of coding medical encounters for billing purposes in the US First published by AMA in 1966 Updated annually on January 1 CPT Coding E & M Codes (Evaluation and Management) Procedural Codes Pathology, Laboratory, Radiology CPT Coding Why do we care? 1. Correct coding results in correct reimbursement 2. Coding errors can result in claim rejection, rebilling and delayed reimbursement 3. Providers are responsible for errors 4. Incorrect coding may result in charges and fines Reimbursement Most family physicians today are employees of a clinic or hospital system Part or all of physician compensation is based on production. Reimbursement Salaries and/or bonuses are typically based on production which is determined one of two ways: Gross receipts minus overhead RVU’s (Relative value units) Either method is ultimately determined by the CPT codes that a provider bills for. Incorrect Coding False Claims Act 1986 HIPAA 1996 The Office of Inspector General (OIG) and the Department of Justice enforce federal, state, and local laws to control healthcare fraud and abuse They conduct investigations and audits pertaining to the delivery of and payment for healthcare services. Incorrect Coding In egregious cases, a doctor can be fined, excluded from Medicare and Medicaid, lose their medical license, and even do jail time. More commonly, the government imposes financial penalties. Incorrect Coding The civil monetary penalty for healthcare fraud has been increased from $2000 to $10,000 for each item or service for which fraudulent payment has been received. The monetary assessment has been increased from not more than twice the amount to not more than three times the amount of the overpayment. Incorrect Coding Two practices have been added to the list of fraudulent activities for which civil monetary penalties may be assessed: 1. Engaging in a pattern of presenting claims based on a code that the person knows or should know will result in greater payments than appropriate. 2. Submitting a claim or claims that the person knows or should know is for a medical item or service that is not medically necessary. Audits and Investigations What will trigger an audit or investigation? A pattern of “upcoding” Whistle blowers E & M codes that are consistently different than average distributions for your specialty Within a group setting, inconsistent coding among partners. Audits and Investigations What will trigger an audit or investigation? Excessive use of a code. Coding level 5 services and not preventive medicine codes for annual physicals. Use of symbols or shorthand Lack of specificity about what you are reviewing. (Review of systems as unremarkable is insufficient) Frequent coding based on “time” CPT codes national average 60.00% 50.00% 40.00% 30.00% CPT codes national average 20.00% 10.00% 0.00% 9921199212992139921499215 Procedural Coding There is a code for every procedure that physicians perform Each code dictates the price for that service that will be charged by the physician Procedural Coding Each code is a five-digit number, which identifies the procedure or service Health care entities (hospitals, clinics, individual providers) attach a price to each code Actual reimbursement will vary depending on what insurance companies or government payers will allow Procedural Coding Organization of codes Anesthesia 00100-01999; 99100-99140 Surgery 10021-69990 Radiology 70010-79999 Pathology & Lab 80048-89356 Medicine 90281-99199; 99500-99602 Procedural Coding Add-on codes Additional procedures that are commonly done in addition to the primary procedure Identified by terms like “each additional” Performed by same physician Cannot be reported separately Procedural Coding Modifiers Additional two-digit code that is added to the primary CPT code Format: 11300-59 Some modifiers are attached to E & M codes; others to procedural codes Procedural Coding Modifiers Both a professional and technical component More than one physician and/or location Only part of a service was performed An adjunctive service was performed A bilateral procedure was performed Service or procedure performed more than once Procedural Coding Global Procedure Codes Most procedure codes are “global”, i.e. they include ALL care related to that particular procedure May or may not include initial encounter For example, fracture care includes initial evaluation, treatment (splint or cast), follow up, and treatment of complications, if done by same provider E & M Coding Evaluation and Management Billing for an E/M service requires the selection of a Current Procedural Terminology (CPT) code that best represents: ❖ Patient type; ❖ Setting of service; and ❖ Level of E/M service performed. E & M Coding The “level” of the code is then determined by three components: Patient History Physical Exam Medical Decision Making For a new patient, all 3 components are used. The lowest “level” determines the code. For established patients, only 2 out of 3 are needed. E & M Coding Patient Type For purposes of billing for E/M services, patients are identified as either new or established: New patient -- has not received any professional services from the physician/non-physician practitioner (NPP) or another physician (of the same specialty) who belongs to the same group practice in the past three years. Established patient -- has received professional services as noted above in the past three years. E & M Coding Patient Type “Any professional services” includes: Emergency department visit Treatment as an inpatient (including newborns) Nursing home visit Outpatient visit at any location E & M Coding Patient Type Example Is #1 Joe comes in c/o cough. He has never been seen at FPC. When reviewing his chart, you see that he had a knee replacement in 2012 at Allen. Dr. Johnston was the attending physician. Family Practice was consulted for medical management of his hypertension. Joe a new or established patient for E & M Coding purposes? E & M Coding Patient Type Example Is #2 Holly comes to the clinic for follow up of hypertension, diabetes and CHF. She moved away in July 2011, but just moved back to Waterloo. Her FPC chart contains a complete history, and her last office visit was 12/01/10. You note that her medications were refilled by phone on 7/01/11. Holly a new or established patient for E & M coding purposes? E & M Coding Patient Type Example Is #3 While you are on team, you admit Alfred for CHF. Dr. Kettman is his PCP. The following year, Alfred changes insurance carriers, and can no longer see Dr. Kettman. He remembers the excellent care you gave him in the hospital, and comes to FPC to see you for his CHF. Alfred a new or established patient for E & M coding purposes? E & M Coding Setting of Service E/M services are categorized into different settings depending on where the service is furnished. Examples of settings include: ❖ Office or other outpatient setting ❖ Hospital inpatient ❖ Emergency department ❖ Nursing facility ❖ Home E & M Coding Setting of Service In each setting, there different types of services which may be billed. OFFICE Office visit Office consultation (new or est.) Preventive medicine services Nursing Facility Initial nursing facility care (new or est.) Subsequent nursing facility care Nursing facility discharge E & M Coding Setting of Service Hospital Initial hospital care (new or est.) Subsequent hospital care Observation (admit/discharge same day) Hospital discharge Inpatient consultation Emergency Department Emergency department visit (new or est.) Physician direction of EMS care E & M Coding Setting of Service Critical Care May be billed in hospital or ED setting Critical care E/M (first 30-74 minutes) Critical care (each additional 30 minutes) Domiciliary or Rest Home Services Home Services E & M Coding Setting of Service Prolonged Services With direct patient contact Without direct patient contact Anticoagulant Management Medical Team Conferences Care Plan Oversight Serices Home health agency Hospice Nursing facility E & M Coding Level of Service Provided In general, the more complex the visit, the higher the level of code the physician or NPP may bill within the appropriate category. In order to bill any code, the services furnished must meet the definition of the code. It is the provider’s responsibility to ensure that the codes selected reflect the services furnished. E & M Coding Level of Service Provided There are three key components when selecting the appropriate level of E/M service provided: Patient History Physical Examination Medical Decision Making The criteria for each component varies depending on the setting and type of service. E & M Coding Level of Service Provided Visits that consist predominately of counseling and/or coordination of care are an exception to this rule. For these visits, time is the key or controlling factor to qualify for a particular level of E/M services. E & M Coding Level of Service Provided E&M CODE HISTORY EXAM MDM 99201 Problem Focused Problem Focused Straightforward 99202 Expanded PF Expanded PF Straightforward 99203 Detailed Detailed Low Complexity 99204 Comprehensive Comprehensive Moderate Complexity 99205 Comprehensive Comprehensive High Complexity E & M Coding Level of Service Provided E&M CODE HISTORY EXAM MDM 99211 Nurse Visit ---- ---- 99202 Problem Focused Problem Focused Straightforward 99203 Expanded PF Expanded PF Low Complexity 99204 Detailed Detailed Moderate Complexity 99205 Comprehensive Comprehensive High Complexity E & M Coding Level of Service Provided Patient History Definitions Problem Focused: CC, brief HPI Expanded PF: CC, brief HPI, pertinent ROS Detailed: CC, extended HPI, extended ROS, pertinent PMH, FH and/or SH Comprehensive: CC, extended HPI, complete ROS, complete PMH, FH and SH E & M Coding Level of Service Provided Patient History Definitions HPI Elements: (Brief 1-3; Extended 4+) Location Duration Severity Modifying factors Context Timing Quality Associated symptoms E & M Coding Level of Service Provided Patient History Definitions ROS Definitions Pertinent=1 Extended 2-9 Comprehensive 10+ E & M Coding Level of Service Provided Organ Systems: Constitutional Eyes ENT Cardiovascular Respiratory GI GU Musculoskeletal Hematologic/Ly mphatic Neurologic Endocrine Psychiatric Skin Allergic E & M Coding Level of Service Provided Physical Exam Definitions Problem focused: limited exam of affected area Expanded PF: limited exam of affected area and related systems Detailed: extended exam of affected area and related systems Comprehensive: general multisystem OR complete exam of affected system E & M Coding Level of Service Provided Physical Exam Definitions Problem-focused: 1-5 elements in 1 or more organ systems/body areas Expanded problem-focused: 6 or more elements in 1 or more organ systems Detailed: at least 2 elements in at least 6 organ systems or body areas OR at least 12 elements in a single organ system Comprehensive: All elements of at least 9 organ systems or body areas OR all elements of one single organ system E & M Coding Level of Service Provided Medical Decision Making Number of possible diagnoses and/or management options Amount or complexity of information Risk of complications, morbidity, and/or mortality E & M Coding Level of Service Provided Medical Decision Making Number of possible diagnoses and/or management options STRAIGHTFORWARD: One self-limited or minor problem LOW COMPLEXITY: * * * * One or two self-limited problem(s) or symptom(s) One stable chronic illness Acute self-limited uncomplicated illness or injury Risk of complications, morbidity or mortality is low E & M Coding Level of Service Provided Medical Decision Making MODERATE COMPLEXITY: * Three or more or self-limited problems * One or more chronic problems with mild to moderate exacerbation, progression or side effects * 2 OR 3 stable chronic illnesses * Undiagnosed new illness, injury or problem with uncertain prognosis * Acute illness with systemic symptoms * Risk of complications, morbidity or mortality is moderate. E & M Coding Level of Service Provided Medical Decision Making HIGH COMPLEXITY: * One or more chronic illnesses with severe exacerbation, progression, side effects * Four or more stable chronic illnesses * Acute complicated injury with significant risk of morbidity or mortality * Acute or chronic illnesses that pose a threat to life or bodily function * Abrupt change in bodily function (e.g., seizure, CVA, acute mental status change) * Risk of complications, morbidity/mortality is high.