IABP- instrumentation, indications and complications
advertisement

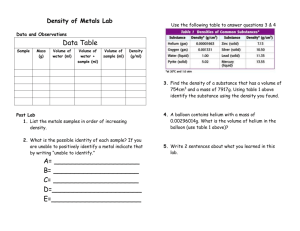
1 Dr Sajeer KT Senior Resident Dept.of Cardiology, MCH Calicut 2 Intra aortic balloon counter pulsation( IABP): Temporary support for the left ventricle by mechanically displacing blood within the aorta Most common and widely available methods of mechanical circulatory support Concepts: - Systolic unloading - Diastolic augmentation Traditionally used in surgical and non surgical patients with cardiogenic shock 3 4 Indications for IABP 1. Cardiogenic shock: - Associated with acute MI - Mechanical complications of MI - MR , VSD 2. In association with CABG : Preoperative insertion - Patients with severe LV dysfunction - Patients with intractable ischemic arrhythmias Postoperative insertion - Postcardiotomy cardiogenic shock 3. In association with nonsurgical revascularization: -Hemodynamically unstable infarct patients -High risk coronary interventions - severe LV dysfunction, LMCA, complex coronary artery disease 4. Stabilization of cardiac transplant recipient before insertion of VAD Post infarction angina Ventricular arrhythmias relathed to ischemia 5 6 Contraindications to IABP Severe aortic insufficiency Aortic aneurysm Aortic dissection Limb ischemia Thrombo embolism 7 8 Cardiac cycle LV contraction: - Isovol. Contraction (b) - maximal ejection (c) LV relaxation: - start of relaxation and reduced ejection (d) - isovol.relaxation (e) LV filling: - LV filling , rapid phase (f) - slow LV filling (g) - atrial systole( a) 9 10 11 12 13 14 Interpreting IABP waveforms 15 IABP –instrumentation and techniques 16 The IAB Counter pulsation system - two principal parts A flexible catheter -2 lumen • first - for distal aspiration/flushing or pressure monitoring • second - for the periodic delivery and removal of helium gas to a closed balloon. A mobile console • system for helium transfer • computer for control of the inflation and deflation cycle 17 18 HEMODYNAMIC EFFECTS — Inflation and deflation of the balloon Blood is displaced to the proximal aorta by inflation during diastole. Aortic volume ( afterload) is reduced during systole through a vacuum effect created by rapid balloon deflation 19 Expected changes with IABP support in hemodynamic profile in patients with Cardiogenic shock - Decrease in SBP by 20 % - Increase in aortic Diastolic Press. by 30 % ( raise coronary blood flow) - Increase in MAP - Reduction of the HR by 20% -Decrease in the mean PCWP by 20 % - Elevation in the COP by 20% 20 21 IABP catheter: 10-20 cm long polyurethane bladder 25cc to 50cc capacity Optimal 85% of aorta occluded (not 100%) The shaft of the balloon catheter contains 2 lumens: - one allows for gas exchange from console to balloon - second lumen - for catheter delivery over a guide wire - for monitoring of central aortic pressure after installation. 22 Intra Aortic Balloon 23 IABP sizing chart 24 Benefits of larger volume IABs More blood volume displacement More diastolic augmentation More systolic unloading 25 IABP Kit Contents Introducer needle • Guide wire • Vessel dilators • Sheath • IABP (34 or 40cc) • Gas tubing • 60-mL syringe • Three-way stopcock 26 Intraaortic balloon 27 STEP BY STEP- IABP insertion Connect ECG Set up pressure lines Femoral access – followed by insertion of the supplied sheath(7.5 F) 0.030 inch supplied J-shaped guide wire to the level of the aortic arch (LAO view) 28 Before taking the Catheter out of Tray 29 Take the entire catheter and T handle as one unit (DO NOT disconnect one-way valve when removing the extracorporeal tubing from the tray.) Pull out the T- handle only as shown 30 Inserting the Balloon catheter • Remove stylet/aspirate/Flush • Insert the balloon only over the guide wire • Hold the catheter close to skin insertion point • Advance in small steps of 1 to 2 cm at a time and stop if any resistance. • The IABP should advance freely - Many vascular complications occur during insertion itself - Resistance during insertion either indicates PVOD, or dissection - Kinking of IABP » improper inflation/deflation 31 Positioning - The end of the balloon should be just distal (1-2 cm) to the takeoff of the left subclavian artery - Position should be confirmed by fluoroscopy or chest x-ray 32 Connecting to console: - Connect helium gas tube to the console via a long extender - Open helium tank. - The central lumen of the catheter is flushed and connected to pressure tubing with 3 way and then to a pressure transducer to allow for monitoring of central aortic pressure. - Zero the transducer Initial set-up: - Once connected properly the console would show ECG and pressure waveforms. - Check Basal mean pressure - Make sure the setting is at “auto” - Usually IABP started at 1:1 or 1:2 augmentation - Usually Augmentation is kept at maxim 33 34 Trigger modes Trigger : - Event the pump uses to identify the onset of cardiac cycle (systole) - Pump must have consistent trigger in order to provide patient assist - If selected trigger not detected, counter pulsation will interrupted 1.ECG - uses the slope of QR segment to detect triggering point 2. AP(Arterial pressure wave) - Systolic upstroke of the arterial pressure wave form is the trigger 3. IN(Internal trigger) 35 ECG signal – most common • Inflation - middle of T wave • Deflation – peak of R wave • Pacer (v/a) • Arterial waveform • An intrinsic pump rate (VF, CPB) 36 Initial settings Auto Operation Mode Automatic lead and trigger selection Automatic and continuous inflation and deflation timing management - User has ability to fine-tune deflation timing Automatic management of irregular rhythms Semi-Auto Operation Mode Operator selects most appropriate lead and trigger source 37 38 39 40 41 The “normal” augmented waveform Increased coronary perfusion 42 Not all Sub optimal augmentation is due to Timing errors/kinks 43 Factors affecting diastolic augmentation Patient - Heart rate - Mean arterial pressure - Stroke volume - Systemic vascular resistance Intra aortic balloon catheter - IAB in sheath - IAB not unfolded - IAB position - Kink in the IAB catheter - IAB leak - Low helium concentration Intra aortic balloon pump - Timing - Position of IAB augmentation control 44 How to check waveform is acceptable ? First change from 1:1 to 1:2 augmentation 45 46 How to check waveform is acceptable ? First change from 1:1 to 1:2 augmentation Check the dicrotic notch See if augmentation starts at that point This should produce a sharp “V” at inflation. 47 How to check waveform is acceptable ? First change from 1:1 to 1:2 augmentation Check the dicrotic notch See if augmentation starts at that point This should produce a sharp “V” at inflation. Check if diastolic augmented wave is › systolic wave 48 How to check waveform is acceptable ? First change from 1:1 to 1:2 augmentation Check the dicrotic notch See if augmentation starts at that point This should produce a sharp “V” at inflation. Check if diastolic augmented wave is › systolic wave Confirm if end diastolic wave following the augmented wave is less than an non augmented wave. Is Deflation slope ok 49 50 Late Inflation Inflation of the IAB markedly after closure of the aortic valve. Waveform Characteristics: • Inflation of IAB after the dicrotic notch. • Absence of sharp V. • Sub optimal diastolic augmentation 51 Early Deflation Premature deflation of the IAB during the diastolic phase. 52 Late Deflation Late deflation of the IAB during the diastolic phase. Waveform Characteristics: • Assisted aortic end diastolic pressure may be equal to the unassisted aortic end diastolic pressure. • Rate of rise of assisted systole is prolonged. • Diastolic augmentation may appear widened 53 Once Arterial waveform is ok, check balloon waveform Normal Balloon Pressure Waveform 54 55 Variation in balloon pressure wave forms Increased duration of plateau due to longer diastolic phase Decreased duration of plateau due to shortened diastolic phase 56 Variation in balloon pressure wave forms Varying R-R intervals result in irregular plateau durations 57 Variation in balloon pressure wave forms Increased height or amplitude of the waveform Decreased height or amplitude of the waveform 58 Variation in balloon pressure wave forms Gas leak Leak in the closed system causing the balloon pressure waveform to fall below zero baseline.. - due to a loose connection - a leak in the IAB catheter - H2O condensation in the external tubing - a patient who is tachycardiac and febrile which causes increased gas diffusion through the IAB membrane 59 Catheter Kink Rounded balloon pressure waveform - Loss of plateau resulting from a kink or obstruction of shuttle gas - Kink in the catheter tubing - Improper IAB catheter position - Sheath not being pulled back to allow inflation of the IAB - IAB is too large for the aorta - IAB is not fully unwrapped - H2O condensation in the external tubing 60 “Balloon too large” syndrome 61 Patient Management During IABP support Anticoagulation-- maintain apTT at 50 to 70 seconds CXR daily – to R/O IAB migration Check lower limb pulses - 2 hourly. - If not palpable » ? - vascular obstruction - thrombus, embolus, or dissection (urgent surgical consultation) Prophylactic antibiotics --?? Hip flexion is restricted, and the head of the bed should not be elevated beyond 30°. 62 Patient Management During IABP support Never leave in standby by mode for more than 20 minutes > thrombus formation Daily – Haemoglobin (risk of bleeding or haemolysis) – Platelet count (risk of thrombocytopenia) – Renal function (risk of acute kidney injury secondary to distal migration of IABP catheter) Wean off the IABP as early as possible as longer duration is associated with higher incidence of limb complications 63 64 Weaning of IABP Timing of weaning: - Patient should be stable for 12 – 24 hours - Decrease inotropic support - Decrease pump ratio – From 1:1 to 1:2 or 1:3 - Decrease augmentation - Monitor patient closely – If patient becomes unstable, weaning should be immediately discontinued 65 IABP Removal -Discontinue heparin 1 hour prior to removal -Disconnect the IAB catheter from the IAB pump - Patient blood pressure will collapse the balloon membrane for withdrawal - Withdraw the IAB catheter through the introducer sheath until resistance is met. - NEVER attempt to withdraw the balloon membrane through the introducer sheath. -Remove the IAB catheter and the introducer sheath as a unit - Check for adequacy of limb perfusion after hemostasis is achieved. 66 67 • 1. Major physiological effects of counter pulsation include? ▫ A) increased coronary artery perfusion, increased preload, decreased after load, decreased myocardial oxygen consumption ▫ B) increased coronary artery perfusion, increased preload, increased after load, decreased myocardial oxygen consumption ▫ C) increased coronary artery perfusion, decreased preload, decreased after load, increased myocardial oxygen consumption ▫ D) increased coronary artery perfusion, decreased preload, decreased after load, decreased myocardial oxygen consumption 68 2. the dicrotic notch on the arterial wave form reflects A) aortic valve opening B) aortic valve closure C) isovolumetric contraction D)rapid ejection 69 3. Expected changes with IABP support in hemodynamic profile in patients with Cardiogenic shock include all except? A) Decrease in SBP by 20 % B) Increase in aortic DP by 30 % C) Decrease in MAP by 10% D) Reduction of the HR by 20% E)Decrease in the mean PCWP by 20 % 70 4. late inflation of the balloon can result in? A) B) C) D) premature augmentation increased augmentation decreased augmentation increased coronary perfusion 71 5. A rounded balloon pressure wave form indicate? A) helium leak B) power failure C) hypovolemia D) balloon occluding the aorta 72 6. width of balloon pressure wave form corresponds to A) length of systole B) length of diastole C) arterial pressure D) helium level 73 7. true statement a) Dicrotic notch- land mark used to set deflation b) Deflation is timed to occur during period of iso volumetric contraction c) Most common trigger used is arterial pressure wave method d) Internal trigger mode is acceptable to use in a patient with normal sinus rhythm 74 8. true statement A) pacing spikes are automatically rejected in ECG triggered modes B) pacing trigger modes can be used in a patient of 50% paced rhythm C) Varying R-R interval result in regular plateau durations in Balloon pressureWave form 75 9. Identify the tracing abnormality 76 10. Identify the tracing abnormality 77 • 1. Major physiological effects of counter pulsation include? ▫ A) increased coronary artery perfusion, increased preload, decreased after load, decreased myocardial oxygen consumption ▫ B) increased coronary artery perfusion, increased preload, increased after load, decreased myocardial oxygen consumption ▫ C) increased coronary artery perfusion, decreased preload, decreased after load, increased myocardial oxygen consumption ▫ D) increased coronary artery perfusion, decreased preload, decreased after load, decreased myocardial oxygen consumption 78 2. the dicrotic notch on the arterial wave form reflects A) aortic valve opening B) aortic valve closure C) isovolumetric contraction D)rapid ejection 79 3. Expected changes with IABP support in hemodynamic profile in patients with Cardiogenic shock include all except? •A) Decrease in SBP by 20 % •B) Increase in aortic DP by 30 % •C) Decrease in MAP by 10% •D) Reduction of the HR by 20% •E)Decrease in the mean PCWP by 20 % 80 4. late inflation of the balloon can result in? • • • • A) premature augmentation B) increased augmentation C) decreased augmentation D) increased coronary perfusion 81 5. A rounded balloon pressure wave form indicate? • A) helium leak • B) power failure • C) hypovolemia • D) balloon occluding the aorta 82 6. width of balloon pressure wave form corresponds to • A) length of systole • B) length of diastole • C) arterial pressure • D) helium level 83 7. true statement a) Dicrotic notch- land mark used to set deflation b) Deflation is timed to occur during period of iso volumetric contraction c) Most common trigger used is arterial pressure wave method d) Internal trigger mode is acceptable to use in a patient with normal sinus rhythm 84 8. true statement A) pacing spikes are automatically rejected in ECG triggered modes B) pacing trigger modes can be used in a patient of 50% paced rhyth C) Varying R-R interval result in regular plateau durations in Balloon press. Wave form 85 9. 86 10.