Here a gap, there a gap, everywhere a gap, gap

Peggy Brown DNP, RN, APRN-CNS-BC, NE-BC
Clinical Quality Coordinator
The Nebraska Medical Center
OBJECTIVES
1. Identify gaps between evidence and practice
2. Recognize the role of Translational Science in improving quality of care
3. Describe one strategy/technique that you could use to facilitate a practice change
MEET YOUR
NEIGHBOR
Share your experience with a GAP
3 minutes
http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx
TRANSLATIONAL SCIENCE
“Diffusion & implementation”
“Knowledge translation & integration”
DISSEMINATION OF EVIDENCE
R E S E A R C H E R U S E R
Practice guidelines
Publications
Tool kits
Presentations
IMPLEMENTATION OF EVIDENCE
U S E R
P A T I E N T
COMPILATION OF
IMPLEMENTATION STRATEGIES
• 6 process
• 68 implementation strategies and definitions
Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT,
Bunger AC, . . . York, J. L. (2012). A compilation of strategies for implementing clinical innovations in health and mental health.
Medical Care Research and Review: MCRR, 69 (2),
123-157.
EXAMPLES OF STRATEGIES
Planning Education
Strategies
Finance
Conduct needs assessment
Involve executive board
Visit other sites
Train-thetrainer
Learning collaborative
Local opinion leaders
Alter incentives
Access new funding
Restructure
Strategies
Quality
Management
Strategies
Revise roles Small tests of change
Change physical structure
Create new service teams
Auditfeedback
Improvement advisor
Powell et al. (2012)
TRANSLATIONAL RESEARCH MODEL
TITLER & EVERETT (2001)
Titler (2008)
•
Advantages
•
Compatibility with values and needs
•
Complexity
•
Feasible
•
Cost
• Mass media
• Opinion leaders –local, respected, influential, competent, trusted to evaluate knowledge
• Change championslocal, expert clinicians, passionate, committed to improve quality, positive working relationships
• Consultation by experts
• Hallway chats, one-to-one
• Stakeholders
• Adoption of practice varies
• Audit and feedback changes behavior
• Opinion leaders
• Change agents
• Organizational resources
• Organizational size
• Organizational culture
• Readiness for change
• Structure supporting
EBP
• Leadership support
IMPLEMENTATION EXAMPLE
Map:
Integrated quality improvement and translational research model
EBP:
Uninterrupted skin-toskin contact at birth
Users
Define
Measure
Analyze
Improve
Innovation
Communication
Social System
Control
Feedback Feedback
Adoption
PROBLEM STATEMENT
In January of 2014, The Joint Commission began mandating that hospitals with > 1,100 births per year, report the percent of newborns that were fed breast milk only from the time of birth to the time of discharge.
From July 2012 to December 2012, 53% of eligible newborns at TNMC were fed breast milk exclusively.
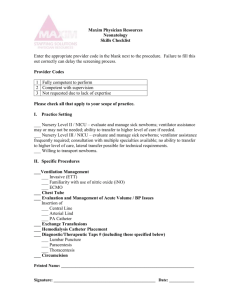
DEFINE
Data recorded manually by Lactation Consultants for every newborn until automated in August 2013 with OneChart report
Goal: top 10 th percentile of UHC
Top 10 th percentile value unknown as new core measure and comparison data not yet available
MEASURES
Exclusive breastfeeding
# Newborns fed breast milk only since birth
# Single, term newborns discharged alive
Skin-to-skin contact at birth
# Newborns with immediate, uninterrupted SSC until after 1st feed
# Term, singleton, healthy newborns
ANALYZE
Supplementation
50% of breastfed newborns were supplemented with nonbreastmilk (Jan’13)
Skin-to-skin contact (SSC) at birth
Literature review for evidence-based best practices revealed
SSC to be the hospital practice most highly correlated with exclusive breastfeeding during hospitalization
20% of healthy term newborns received skin-to-skin contact at birth (mother interviews, Jan’13)
ANALYZE
Benefits of skin-to-skin contact at birth
• Physiologic stability o Respirations, temperature, glucose levels, decreased crying & stress
• Promotes attachment behaviors o Short-term and long-term
• Increased exclusive breastfeeding in hospital
• Longer duration of breastfeeding
Critical X’s
Supplementation with non-human milk
Limited skin-to-skin contact at birth
Solution
Follow provider orders not to supplement breastfed newborns without first notifying provider.
Documentation of informed decision or medical indication for supplementation with non-human milk. Education to providers, nurses and parents on indications for supplementation.
Implement evidence-based practice of Skin-to-skin contact at birth
IMPROVE – CHARACTERISTICS OF INNOVATION
Skin-to-skin contact at birth has been recommended by leading health organizations since 1998 (WHO, AAP, ABM, NRP)
Relatively simple
Requires change in work flow
Numerous benefits
IMPROVE - COMMUNICATION
Increase understanding of advantages of innovation
You-tube videos of SSC
Emails
Links to websites
Research abstracts
Unit meetings
Class for professionals
One-to-one discussions with change champions/opinion leaders
Bulletin boards
IMPROVE - USERS
Nurses & Providers
Opinion leaders
Change champions
IMPROVE – SOCIAL SYSTEM
Provided structure for innovation:
Shared governance structure
Quality triad
Policy/procedure
CONTROL – JULY 2013
Audit-feedback
Skin-to-skin contact weekly, individual
Monthly exclusive breastfeeding %
EBF & SSC Trends
100
90
80
70
60
50
40
30
20
10
0
Project Kickoff
Clarification of orders
SSC
SSC
Q1'13 Q2
EBF all healthy newborns
SSC audit
Q3 Q4
EBF mother planned to EBF
CONTROL – JANUARY 2014
Monthly/Quarterly skin-to-skin percentages
Feedback for individual trends
10 th percentile – Are we there?
SHARE WITH YOUR NEIGHBOR
Strategy you may use to enhance implementation of the next evidence-based practice
3 minutes
OBJECTIVES
1. Identify gaps between evidence and practice
2. Recognize the role of Translational Science in improving quality of care
3. Describe one strategy/technique that you could use to facilitate a practice change
Powell BJ, McMillen, JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, . . . York, J.
L. (2012). A compilation of strategies for implementing clinical innovations in health and mental health.
Medical Care Research and Review: MCRR, 69 (2),
123-157.
Rogers, E.M. (2003). Diffusion of Innovations. New York : Free Press.
Titler MG, & Everett, L. Q. (2001). Translating research into practice. considerations for critical care investigators.
Critical Care Nursing Clinics of North America,
13 (4), 587-604.
Titler, M. G. (2010). Translation science and context.
Research & Theory for Nursing
Practice, 24 (1), 35-55. doi:10.1891/1541-6577.24.1.35
Titler, M. (2008). Evidence for EBP implementation. AHRQ nursing handbook (1st ed., pp. Ch 7)
Titler, M. G. (2011). Nursing science and evidence-based practice.
Western Journal of Nursing Research, 33 (3), 291-295. doi:10.1177/0193945910388984