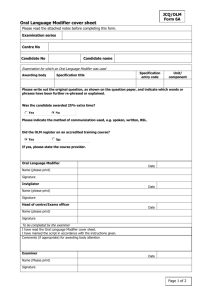
ICD-10
advertisement

MODIFIERS
Kandy Morris CPC,CPMA,CPB,
CEMC, CCS-P, CPO-C
What Are Modifiers?
Modifiers are two digit codes appended to a CPT code
that indicates that a service or procedure has
been altered by a specific circumstance, but
has not changed in its basic definition
“Strictly alters the code definition”
Why do we use Modifiers?
Modifiers are used for a variety of reasons, including:
Claims can be incomplete or inaccurate without a modifier
Coding to the highest level of specificity requires modifier use
Appropriate use of modifiers get services reimbursed that
might otherwise be denied
Allows for proper reimbursement (increased or decreased)
based on the procedure/service circumstances
………….and to avoid hearing your physician saying……….
Why aren’t my claims
getting paid……?
Where to find Modifiers
CPT Book - Appendix A
HCPCS Level II - Appendix 2
Modifiers denote that:
A service or procedure has both a professional and technical components
A service or procedure was performed by more than one physician
A service or procedure has been reduced or increased
Only part of a procedure was performed
A service or procedure was provided more than once
A bilateral procedure was performed
Unusual events occurred
Modifier Categories
Global
CCI
Package Modifiers
or Bundling Modifiers
Evaluation
and Management Only Modifiers
Number
of Surgeon Modifiers
“Other”
Modifiers
Global Modifiers
What is the “Global” Period?
Also known as the global surgical package. CMS and AMA have the same
definition. Per CPT Guidelines, the following services are always included
in addition to the operation:
Local or topical anesthesia
Subsequent to the decision for surgery, one related E/M encounter on the
date immediately prior to or on the date of the procedure (including
history and physical)
Immediate postoperative care
Writing orders
Evaluating the patient in the post-anesthesia recovery area
Typical postoperative follow-up care
Examples of Services Included in the
Global Period
A
visit with a patient prior to surgery
to answer last minute questions
Removal of staples 10 days after a
surgical procedure
A post-operative visit in the office to
check on wound healing
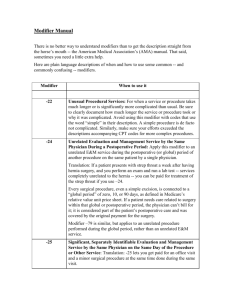
Modifier – 24 Unrelated E/M Service by Same Physician
During a Postoperative Period:
(Appended to the E&M code only)
Used when a physician provides a surgical service related to one
problem, and then during the postoperative period provides an E&M
service that is unrelated to the surgery.
Diagnosis code selection is critical to indicate the reason for the
additional E&M service
Modifier Category: E/M Only & Global Package
Modifier - 24
Example: Patient came in for a post-operative visit. He is
12 weeks s/p discectomy. During the exam the pt c/o
severe headaches with visual changes, proceeded by an
aura. The physician performs an expanded problem focused
exam. His impression is migraine with medical decision
making of low complexity.
Report: CPT Code 99213(24) Level 3, established patient
office visit
Modifier – 25 Significant, Separately Identifiable E/M by
the Same Physician on the Same Day of the Procedure or
other service
(Append to E&M Code Only)
Indicates that on the day of a procedure or other service, the patients
condition required an additional E&M service above and beyond the usual
pre and post-op care associated with the procedure performed.
E&M service elements must be clearly documented to justify that a visit
took place beyond the elements necessary to perform the procedure.
Modifier Category: E/M Only & Global Package
Modifier – 25
Example: An established patient is seen by
the physician to evaluate his general
osteoarthritis, benign HTN and NIDDM. While
examining the patient, the physician
determines that an arthrocentesis of the
patient’s knee joint needs to be performed.
Report: 9921X(25) & 20610
Modifier – 26 Professional Component
(Appended to procedure code)
Certain procedures are a combination of a physician component
and a technical component.
When the physician component is reported separately, add -26
to the CPT code to identify that the physician’s component
ONLY is being billed.
Modifier – 26 Professional Component
(Appended to procedure code)
For use by physicians when utilizing equipment owned by a hospital/facility
Interpretations must be separate, distinct, written and signed
Not all procedures have a professional/technical split
Refer to Medicare Fee Schedule to determine what procedures are eligible for this
modifier
Common Services billed with – 26: Radiology, Stress Tests, Heart Catheterizations
Modifier - 26
Certain procedures are a combination of a physician component and a
technical component. When physician component is reported separately,
add -26 to the CPT code to identify that the physician’s component only
is being billed.
Example: A 72 year old woman comes to the Emergency Room
complaining of chest discomfort. The physician orders a complete 2D
echocardiography using the hospital equipment. The physician provides
the written interpretation.
Report: CPT Codes 93307(26)
Modifier – 54 Surgical Care Only
(Appended to the surgical procedure codes only)
Physician service to the patient was only the intra-operative procedure. (The physician is paid
a portion of the global package and another physician will perform the pre & post-operative
care)
There should be agreement for the transfer of care between physicians
Do not use with procedure codes having a zero day global period
Do not use -54 if physician is a covering physician (locum tenens) or part of the same group as
the physician who performed the procedure
Example: A neurosurgeon travels to a rural location to perform a craniotomy for drainage of an
intracranial abscess. He assessed the patient the day before, and performed the procedure. Follow-up
care was provided by a local surgeon. The Neurosurgeon would report 61321-54
Modifier – 55 Post Operative Management Only
(Appended to the surgical procedure codes only)
Modifier 55 is reported when one physician performed
the postoperative management only; another physician
performed the surgical procedure
Example: While on vacation in Vail, the patient had a skiing accident. A local
Orthopedist in Vail did the pre-operative & intra-operative procedure. The patient’s
physician at home provides all the post-op care and would bill by adding a -55 to the
surgical procedure code.
Modifier – 56 Pre Operative Management Only
(Appended to the surgical procedure codes only)
Modifier 56 is reported when one physician performed
the preoperative care and evaluation and another
physician performed the surgical procedure
Example: Internist does pre-op work-up on a patient having a laparoscopic
cholecystectomy by a general surgeon who travels to the area monthly.
Internist would bill 47562-56
Modifier-57 Decision for Surgery
(Appended to E&M code only)
The purpose of this modifier is to report an E&M service on the day before or on the
day of a major surgery (90 day global period) which results in the initial decision to
perform the surgery
Without using this modifier on the E&M code the E&M will be denied as
“included in the Global period of the surgical procedure”.
Example: Patient comes to the emergency department with sudden onset of acute abdominal
pain. GYN physician evaluates patient & determines that patient has a twisted ovarian cyst.
Physician admits patient to OR for a right salpingo-oophorectomy. CPT codes report are
99223(57) & 58720.
Modifier Category: E/M Only & Global Package
Modifier-58 Staged or Related Procedure by the
Same Physician during the Postoperative Period
(Appended to surgical code)
The purpose of this modifier is to report the performance of a procedure or service
during the postoperative period for one of the following circumstance's:
planned or staged
more extensive than the original procedure
therapy following a surgical procedure
This modifier is used to report a staged or related procedure by the same physician
during the postoperative period of the first procedure
Modifier -58 is used ONLY during the global surgical period for the original procedure
Modifier-58 Staged or Related Procedure by the
Same Physician during the Postoperative Period
(Appended to surgical code)
The purpose of this modifier is to report the performance of a procedure or service
during the postoperative period for one of the following circumstance's:
planned or staged
more extensive than the original procedure
therapy following a surgical procedure
This modifier is used to report a staged or related procedure by the same physician
during the postoperative period of the first procedure
Modifier -58 is used ONLY during the global surgical period for the original procedure
Modifier – 58 Clinical Examples
Example # 1: 32 year old woman with breast cancer undergoes a
mastectomy one week ago. Today, she is scheduled to have breast
implants placed
Report: 19342(58)
Example # 2: Sternal debridement performed for mediastinitis and it is
noted that a muscle flap repair will be needed in a few days to close the
defect
Report: 15734(58) since the muscle flap was planned at the time of
the initial surgery
Modifier Category: Global Package
Modifier-62 Co-Surgeon
When two or more surgeons with different specialties submit claims for the same
operative session for the same beneficiary and same date of service, all providers
must use the co-surgeon modifier.
When two different providers bill the same CPT code, same patient and same date of
service and one of the providers bills with modifier 62, the other provider must also
bill with modifier 62. Note, however, that modifier 62 may only be used when the cosurgeons are of different specialties and are working simultaneously.
Modifier-62 Clinical Examples
Example # 1: A provider bills for CPT code 61548,
Hypophysectomy or excision of pituitary tumor, and bills
with modifier 62, for a patient on date of service March
8, 2014. A different provider bills for the same service
for the same patient on the same date of service
because he/she was the co-surgeon, yet did not bill with
modifier 62. The second surgeon was overpaid for failing
to properly apply modifier 62.
Example # 2: A provider bills for CPT code 49652,
Laparoscopy, Surgical repair, ventral, umbilical, spigelian
or epigastric hernia, and bills with modifier 62, for a
patient on July 2, 2014. A different provider bills for the
same service for the same patient on the same date of
service because he/she was the co-surgeon, yet did not
bill with modifier 62. The second surgeon was overpaid
for failing to properly apply modifier 62.
Modifier-76 Repeat Procedure by the Same
Physician
(Appended to procedure code)
Modifier -76 is used when it is necessary to report a repeat of the same procedure on the same day
Medicare considers two physicians, in the same group with the same specialty performing services on
the same day as the same person
Appropriate Usage: On procedure codes that cannot be quantity billed
Report each service on a separate line, using a quantity of one and append 76 to the subsequent
procedures
The SAME physician performs the services
Inappropriate Usage: Appending to a surgical code
Appending to each line of service
Repeat services due to equipment or other technical failure
For services repeated for quality control purposes
Modifier - 76
Medicare considers two physicians, in the same group with the
same specialty performing services on the same day as the
same physician
For all procedure codes that cannot be quantity billed always
use quantity of “1”
To avoid denials, bill all services performed on one day on the
same claim
For repeat clinical diagnostic laboratory tests, use modifier 91
if the service can not be quantity billed
Modifier Category: Global Package
Modifier-77 Repeat Procedure by Another Physician
(Appended to procedure code)
Repeat procedure by a different physician; use when it is necessary to report repeat
procedure performed on the same day
Appropriate Usage: A different physician performs the repeat services
Inappropriate Usage: Appending to a surgical procedure code
Appending when the repeat procedure is performed by the same physician
Appending to E&M codes
Modifier Category: Global Package
Modifier – 77
Example: A PCP performs a chest x-ray in his
office and observes a suspicious mass. He
sends the patient to a Pulmonologist who, on
the same day, repeats the CXR.
The Pulmonologist should submit their claim
with the 77 modifier and provide
documentation to support the need for a
repeat CXR.
Modifier-78 Unplanned Return to the
Operating/Procedure Room by the Same Physician
Following Initial Procedure for a Related Procedure
During the Postop Period
(Appended to procedure code)
The purpose of this modifier is to report a related procedure performed during the postoperative
period of the initial procedure (unplanned procedure following initial procedure) and requires use of
the operating/procedure room
Modifier -78 should NOT be used if a complication does not require use of the operating/procedure
room
Modifier -78 may be used to report procedure performed on the same day (usually in emergency
situations)
Modifier Category: Global Package
Modifier – 78
Example: Pt brought to recovery room S/P abdominal
surgery. Dressings became saturated, vital signs were
unstable. Pt brought back to OR for exploration postop hemorrhage
Report: CPT Codes 35840(78)
“Complication” modifier
Modifier Category: Global Package
Modifier-79 Unrelated Procedure/Service by Same
MD during the Post-op Period
(Appended to procedure code)
The purpose of this modifier is to report services during the postoperative
period that are unrelated to the original procedure
The procedure must be performed by the same physician, and modifier 79 is appended to the procedure code
Claim should be submitted with a different diagnosis and documentation
should support the different diagnosis and medical necessity
Modifier Category: Global Package
Modifier - 79
Example: A cataract removal of the
right eye(90 day global) is performed on
Jan. 5th. On Feb. 12th, the same
physician performs a cataract removal
on the left eye.
Report:
CPT Code 66984(79)
“Other” Modifiers
Modifier-22 Unusual Procedural Services
(Appended to procedure code)
Indicates that procedure was more complicated or complex
Alerts payers to unusual circumstances or complications during a
procedure
Increased work effort of 30-50%
Must be accompanied by an operative report with a letter explaining
additional time required to support modifier -22 use
Modifier-22 Unusual Procedural Services
(Appended to procedure code)
Operative/Procedure Note Key Terms:
Increased risk; difficult; extended; complication; prolonged; unusual findings; unusual
contamination controls; hemorrhage, blood loss over 600cc; etc
Additional physician work due to complications or medical emergencies may warrant use of 22
Documentation MUST support the substantial additional work and the reason for the
additional work (i.e., increased intensity, time, technical difficulty of procedure, severity of
patient’s condition, physical and mental effort required)
Overuse can trigger an audit, if you find yourself consistently using modifier -22, chances are
you are using the wrong CPT
Use of Modifier - 22
Appropriate Use:
Inappropriate Use:
Partial colectomy in a
patient with a tumor
adherent to vascular
structures requiring
additional 60 minutes of
dissection (due to
increased risk and time)
Partial colectomy with
accidental laceration of
vessel resulting in
additional time for
repair
Modifier-50 Bilateral Procedure
(Appended to procedure code)
Used to report bilateral procedures that are performed at the same operative session
(bi = two, lateral = side; both sides)
Modifier -50 is used to report diagnostic, radiology and surgical procedures
Modifier -50 should only be applied to services and/or procedure performed on identical
anatomic sites, aspects, or organs (arms, legs, eyes, breasts)
Modifier -50 is NOT applicable to:
Procedures that are bilateral by definition
Procedures with descriptions including the terminology as “bilateral” or “unilateral”
When removing a lesion on the right arm and one on the left arm (RT/LT should be used)
Modifier-50 Bilateral Procedure
(Appended to procedure code)
Modifier -50 CAN be appended to codes with a bilateral indicator of “1”
or “3” on the Medicare Physician Fee Schedule
https://www.cms.gov/apps/physician-fee-schedule/search/search-criteria.aspx
Some payers require the bilateral procedure to be report on a single line
with -50; however some may require the procedure to be reported on two
separate lines using RT/LT modifiers (check with the individual payer for
their bilateral billing policy)
Modifier – 51 Multiple Procedures
(Append to Procedure Code)
Used when multiple procedures, other than E/M services, performed at the
same session by the same provider
Reimbursement is subject to 100% of the allowable charge for the primary
code and 50% of the allowable charge for each additional procedure code
Example: Patient presents for removal of a malignant lesion on the face with a
complex repair of the defect
Report: Line 1: 11641
Line 2: 13152(51)
Paid at 100% of Allowed
Paid at 50% of Allowed
Modifier - 51
The surgical procedure with the highest allowable amount is
considered the primary (first) procedure. Medicare uses the RVU for
this determination, which can be found on the Physician Fee Schedule
Do NOT use -51 on the primary procedure, only on the secondary
procedures (order procedures by RVU; highest to lowest)
Do NOT use -51 on procedures with a “+” or "∅“symbol indicated in
the CPT Manual (See Appendix D and E)
These codes can also be identified on the Medicare Physician Fee
Schedule with a Multiple Procedure Indicator of “3”
Modifier-52 Reduced Service
(Appended to procedure code)
This modifier is used to report a service or procedure that is partially reduced or
eliminated at the physician’s election
Modifier -52 is NOT used to report an elective cancellation of a procedure before
surgical preparation in the operating suite
Modifier -52 should NOT be used if the procedure is discontinued after administration
of anesthesia
The presence of modifier -52 will reduce the payment of the service. Depending
upon the payer
Modifier-53 Discontinued Procedure
(Appended to procedure code)
Used to indicate that a surgical or diagnostic procedure was started but discontinued due to
extenuating circumstances that threaten the patient’s well-being
This modifier is used to report services or procedures when discontinued after anesthesia is
administered to the patient
This modifier is NOT used to report an elective cancellation of a procedure or prior to the patient’s
anesthesia induction and/or surgical preparation in the operating suite; including situations where
cancellation is due to patient instability
Modifier -53 should NOT be used when a laparoscopic or endoscopic procedure is converted to an open
procedure
Modifier -53 should NOT be appended to E/M codes
CCI or Bundling Modifiers
What is CCI or NCCI?
CMS developed the National Correct Coding Initiative (NCCI) to promote national
correct coding methodologies and to control improper coding leading to inappropriate
payment in Part B claims. The CMS developed its coding policies based on coding
conventions defined by the American Medical Association’s CPT manual, national and
local policies and edits, coding guidelines developed by national societies, analysis of
standard medical and surgical practices, and a review of current coding practices
NCCI (National Correct Coding Initiative ) edits, which are released by CMS quarterly,
define when two procedures HCPCS/CPT codes may not be reported together except
under special circumstances. If an edit allows use of NCCI associated modifiers, the
two procedure codes may be reported together if the two procedures are performed
at different anatomic sites or different patient encounters
Edits can be viewed @:
https://www.cms.gov/NationalCorrectCodInitEd/01_overview.asp
•
Modifier-59 Distinct Procedural Service
(Appended to procedure code)
The purpose of this modifier is to identify procedures or services that are not usually reported
together but appropriate under the circumstance. This may represent the following:
A different session or patient encounter
A different procedure or surgery
A different site or organ system
A separate incision or excision
A separate lesion
A separate injury (or area of injury in extensive injuries)
Modifier -59 should only be used if no other modifier more appropriately describes the relationships
of the two or more procedure codes (i.e. RT/LT, T1-T10, etc.)
Modifier 59 should NOT be appended to an E/M code
CMS is establishing the following four new HCPCS modifiers (referred to collectively as -X{EPSU} modifiers) to define
specific subsets of the -59 modifier:
-XE Separate Encounter: A Service That Is Distinct Because It Occurred During A Separate Encounter.
Separate surgical operative session on the same date of service (e.g. 8 AM surgery with one procedure, 4 PM surgery with second
procedure code).
If a patient came in for an outpatient EKG, then comes back later in the day for blood work, the blood work would require an XE
modifier.
Patient comes to the facility for an x-ray of their hip as a result of an injury. The results are sent to the physician’s office who calls the
patient and has them return to the radiology department for a CT of their hip due to possibility of a hairline fracture all on the same
day.
-XS Separate Structure: A Service That Is Distinct Because It Was Performed On A Separate Organ/Structure.
From an NCCI perspective, the definition of different anatomic sites includes different organs or different lesions in the same organ.
However, it does not include treatment of contiguous structures of the same organ.
Injection into tendon sheath, right ankle (20550) and injection into tendon sheath, left ankle (20550-XS).
Right pectoralis major muscle flap (15734) and right rectus abdominis muscle flap (15734-XS)
-XP Separate Practitioner: A Service That Is Distinct Because It Was Performed By A Different Practitioner.
The patient is seen in the office by a family practice physician, who in the course of the visit encounters a problem outside
their scope of ability so calls in (or arranges an immediate transfer to) a specialist physician at the same claim to perform the
needed service.
-XP modifier still unclear, but probable scenario: The patient is seen by one provider who in the course of treating a patient
encounters a problem outside his scope of ability so calls in another doctor to perform the service.
Patient goes to their family physician due to a cold, after being seen by their physician the are sent to their respiratory
physician for breathing treatments, all on the same day.
-XU Unusual Non-Overlapping Service: The Use Of A Service That Is Distinct Because It Does Not Overlap Usual
Components Of The Main Service.
A diagnostic procedure is performed. Due to the findings, a decision is then made to perform a therapeutic/surgical
procedure. (This may or may not occur in the same procedure room during the same session/encounter.) For example,
diagnostic cardiac angiography leads to therapeutic angioplasty.
Patient is seen in the OR for an EGD procedure in the recovery room the patient is noted to be short of breath and a fever,
patient receives a chest x-ray to rule out pneumonia.
Excision of two non-contiguous lesions on the same structure or body area that might typically be bundled together can be
separated by this modifier.
CMS will continue to recognize the -59 modifier, but notes that Current Procedural
Terminology (CPT) instructions state that the -59 modifier should not be used when a more
descriptive modifier is available. While CMS will continue to recognize the -59 modifier in
many instances, it may selectively require a more specific - X{EPSU} modifier for billing
certain codes at high risk for incorrect billing. For example, a particular NCCI PTP code pair
may be identified as payable only with the -XE separate encounter modifier but not the -59
or other -X{EPSU} modifiers. The -X{EPSU} modifiers are more selective versions of the -59
modifier so it would be incorrect to include both modifiers on the same line.
The combination of alternative specific modifiers with a general less specific modifier
creates additional discrimination in both reporting and editing. As a default, at this time CMS
will initially accept either a -59 modifier or a more selective - X{EPSU} modifier as correct
coding, although the rapid migration of providers to the more selective modifiers is
encouraged.
However, please note that these modifiers are valid even before national edits are in place.
MACs are not prohibited from requiring the use of selective modifiers in lieu of the general 59 modifier, when necessitated by local program integrity and compliance needs.
Number of Surgeons Modifiers
How to Determine if Multiple Surgeons
Are Allowed
To determine whether the services of more than one surgeon may be submitted to
Medicare with CPT Modifiers 62, 66, 80, 81, 82 or AS, refer to the Medicare Physician
Fee Schedule database (MPFSDB):
Access the database directly from the CMS Web Site at
www.cms.gov/apps/physician-fee-schedule/overview.aspx/
Select Physician Fee Schedule Search from the left area of the Web page
Refer to the column headings applicable:
‘Co Surg’, ‘Team Surg’, or Asst Surg’
0 = Co-surgeons not permitted for this procedure
1 = Co-surgeons may be paid if supporting documentation is supplied to
establish medical necessity
2 = Co-surgeons permitted. No documentation is required if twospeciality requirement in met
Modifier – 62 Two Surgeons
(Append to Surgical Procedure)
Two surgeons (each in a different specialty) work together to perform a specific
procedure
If two surgeons (each in a different specialty) are required to perform a specific
procedure, each surgeon bills for the procedure, and both surgeons need to report the
same surgery code with the modifier 62.
Example: Thansphenoidal Hypophesectomy, Neurosurgeon and ENT both
report 61548(62)
Warning: If one surgeon bills with a modifier “-62” and one surgeon bills with no
modifier, the payer may deny or suspend the claim with the modifier for review.
Coordination of billing is key to proper reimbursement for each surgeon!
Modifier
– 80 Assistant Surgeon (for MD’s,
DO’s)
Modifier – 81 Minimal Assistant Surgeon
Modifier – 82 Assistant surgeon (when
qualified resident surgeon not
available)
Modifier – AS Physician assistant, nurse
practitioner, or clinical nurse
specialist services for assistant
at surgery
HCPCS Level II Modifiers
Alpha
or alphanumeric
Provide additional information just like
CPT modifiers
Found in HCPCS Manual
Can be used on Level I CPT codes
and/or Level II HCPCS codes
Examples of HCPCS Modifiers
LT: Left side
RT: Right side
GA: Waiver of liability statement on file
RR: Rental (for DME)
F1: Left hand, 2nd digit
F6: Right hand, 2nd digit
GP: Services delivered under an outpatient physical
therapy plan of care
Modifiers – Work Comp/Colorado
Modifier – 00 All providers should indicate whether they are
billing for the total component for a radiology
service
Questions?????
Feel free to email me directly at mzkandyd@gmail.com
Kandy Morris CPC, CPMA, CPB, CEMC, CCS-P, CPO-C
2015 Las Vegas Chapter Vice President
Physicians Choice, LLC
2657 Windmill Pkwy, Suite# 590
Henderson, NV 89074
Phone: 702.550.8769/Fax: 702.543.7095