Lab 2 Blood - Winona State University
advertisement

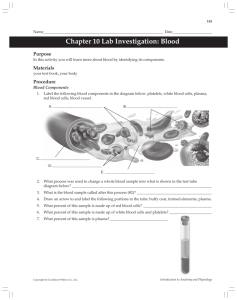
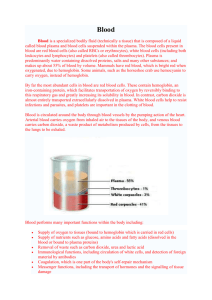
Biology 212: Anatomy and Physiology II Lab #2: BLOOD/HEMATOLOGY Blood is one of the most important components of the human body. It transports materials (i.e., oxygen, carbon dioxide, hormones, waste products, nutrients, etc.) from one area of the body to another and allows tissues in distant areas to communicate with one another. In addition, blood protects us from harmful things like bacteria and viruses via the coordinated actions of a variety of different types of leukocytes (a.k.a. white blood cells). The average human body contains roughly 5 liters of blood that is constantly being forced through our arteries and veins by the heart. Many pathologies of the human body involve blood.. For example, anemia can result from excess blood loss or the inability to form red blood cells and deliver oxygen to the body or parts of the body. Heart disease risk is associated with the large amounts of LDL (bad) cholesterol, low HDL (good) cholesterol, and high levels of triglycerides in the blood. Blood clotting (i.e., hemostasis) of blood are associated with inappropriate blood clot formation (i.e. stroke) and an inability to form blood clots (hemophilia). Blood is technically a type of connective tissue that essentially consists of two fractions: 1. Formed elements – the cells and cell fragments found in blood a. Erythrocytes (red blood cells) b. Leukocytes (white blood cells) c. Platelets 2. Plasma – the “liquid/matrix” portion of blood. Blood plasma contains a great deal of water, ions, proteins, antibodies, and clotting factors. The analysis of blood and its components are very important clinically since the body often changes the composition of blood in response to various conditions (changes in physiology or disease). The clinical study of blood and its components is known as HEMATOLOGY and CLINICAL CHEMISTRY. A Clinical Laboratory Scientist completes these types of blood analyses. Part of the job of an RN is to explain what the clinical values mean to their patients and what it means in terms of their disease diagnosis In this lab exercise, we will draw a small blood sample from a finger (not the arm). We will examine the different components of blood as well as look at some of the basic diagnostic tests commonly used in hematology. Working safely with blood In this lab exercise, we will be working with human blood (your own). If you are not comfortable with blood donation, if you know you are sick, if you have history of fainting, if you consider yourself at risk for transmitting a blood born disease, etc., then please do not draw your own blood. Work to safely support your peers in your laboratory group. While it is somewhat unlikely that someone in this class carries an infectious agent in their blood (bacteria, viruses), it is common practice in the lab to simply assume that every blood, tissue, or fluid sample you deal with is tainted with something harmful. As a result, it is important to 1 remember to wear disposable gloves whenever you are handling blood or any materials that have come into contact with blood (even if it is your own). Disinfecting solutions will be supplied by the department and will be in the lab for your use. Anything that comes in contact with blood must be disinfected and materials that will be disposed of (microscope slides, gloves, lancets) must be placed in designated “biohazard” receptacles and NOT the regular trash! Wash your hands before leaving the lab. Blood Plasma: It is important to understand some of plasma’s properties, even though it is not the major focus of this lab. Plasma makes up approximately 55-60% of our blood volume and is nearly 90% water. The remaining 10% of plasma consists of ions (i.e., electrolytes), many different proteins, antibodies, and hormones. When fresh blood is allowed to settle, the formed elements sink to the bottom and a yellow-tan (straw colored) fluid rises to the top. This yellow fluid is the blood plasma. Blood plasma contains many important molecules such as antibodies needed to fight infections as well as critical clotting factors. These molecules are very much sought after for therapeutic/clinical applications, which explains why plasma centers often pay cash for poor college student’s blood plasma! Since plasma is 90% water, it is a major reservoir for water in our bodies. When we become dehydrated our tissues pull water from our plasma and our overall blood volume drops. If we are over-hydrated, the extra fluid volume is added to the blood stream (plasma) where it can eventually be removed by the kidneys and excreted as urine. In addition to acting as a reservoir for water, plasma also plays an important role in maintaining the pH, or acid/base, balance of the body. Plasma contains buffer molecules which allow the blood and most other tissues of the body to maintain a relatively constant pH of roughly 7.4. Finally, plasma plays an important role in maintaining body temperature near 98.6oF. Water has a great capacity to absorb and release heat. As a result on a hot day, plasma supplies the water in sweat that helps cool our bodies. On a cold day, delivery of warm plasma from our body’s core to our extremities (i.e. fingers) hopefully keeps them from freezing when we are outside enjoying the Minnesota winter! It is important to be aware of the composition of plasma as we study our hematocrits later on in lab . . . Exercise #1: Formed elements of blood: Keep in mind that the formed elements of blood consist of erythrocytes, leukocytes, and platelets. In this exercise, we will be studying the formed elements of blood using the blood smear slides found in your slide boxes (Slide #6). Since these are prepared slides and have been sterilized, you won’t be needing gloves for this exercise. Our focus will be on the morphology of erythrocytes as well as the various different types of leukocytes found in human blood. NOTE: the identification of most of the different types of leukocytes is most easily accomplished by looking at the relative size of the leukocyte and also at the structure of the nucleus (remember, erythrocytes don’t have a nucleus). The vast majority of the cells that you see on a blood smear will be erythrocytes (no nucleus), so when identifying the different leukocytes, just look for cells that have a dark-stained nucleus. That being said, you won’t be able to identify EVERY cell that has a nucleus since some cells will have been damaged during the processing of the slide. As you proceed, make sure you look at the images in your text book to familiarize yourself with what a “typical” WBC looks like and search your slide for that rather than simply picking a random cell and trying to determine its identity. Make sure everyone in your group can 2 identify the various white cells. Check out Chapter 18 in Saladin for images and descriptions of the different leukocytes (Figure 18.1) or use one of the Histology textbooks in the lab. The appearance of the slide and the cells are shown above. The clinician has to determine the percentage of each cell type and determine if this is a normal or abnormal relative to what was expected. They use cell size determinations and also the shape of the nucleus of individual cells to discern cell type. Erythrocytes: By far, erythrocytes are the most numerous of the cells you will see on a blood smear. From your Bio 211 experience, you will remember that erythrocytes are small (7.5 microns in diameter), round, and have an indented center. Basically, they look like little doughnuts that lack a nucleus. Platelets: Platelets will often have an irregular shape and be much SMALLER (1-2 microns in diameter) than an erythrocyte. Platelets also lack a nucleus since they are really only fragments of a cell. They tend to stain dark in color. Leukocytes: There are two main categories of leukocytes in human blood, GRANULOCYTES and AGRANULOCYTES. Granulocytes will possess visible stained granules (look like speckles within the cell), while agranulocytes will not. Additionally, granulocytes tend to possess a nucleus which is more lobed in appearance (often makes them look like they are multinucleated), while agranulocytes tend to possess a more rounded nuclei that we commonly expect to see in most cells. Granulocytes: 1. Neutrophils – the most common granulocyte. These cells should be pretty easy to identify based on their sheer numbers. Neutrophils are phagocytic cells which play an important role both in the bloodstream as well as in tissues where infections may occur. Their numbers will increase dramatically when an individual is sick with a viral or bacterial infection. This phenomenon is commonly referred to as an “elevated white cell count” by clinicians and is confirmed through a blood test. However, neutrophils are not the only cells which increase in number in response to an infection. Neutrophils typically possess a nucleus consisting of three or more “lobes” that often can be seen connected by thinner strands. However, some cells may simply appear to have more than one nucleus, even though in reality there is only one. 2. Eosinophils – much less common than neutrophils, and you may need to spend a few minutes to identify one. Eosinophils are phagocytic cells like the neutrophils but contain large granules that tend to stain a distinctive orange or red due to the fact that the granules absorb and bind a dye known as EOSIN. Eosinophils possess a nucleus that consists of two large lobes. 3. Basophils – MUCH LESS common than neutrophils and eosinophils. The granules of these cells possess histamine and heparin which is released in response to inflammation and tissue injury. As 3 a result, these cells spend more time within a tissue than in the bloodstream and may be difficult to find. Eosinophils are not phagocytic and contain many dark-staining granules that may hide the nucleus. When you can see one, the nucleus of a basophil often appears U- or S-shaped. You may have to look at a couple of slides before you see one, but at least be sure you are familiar with their appearance by looking at a photo in your textbook!! Agranulocytes: 1. Lymphocytes – fairly common in the bloodstream. Since lymphocytes are agranulocytes, you won’t be able to see any granules in the cytoplasm of the cell. Lymphocytes are a very diverse group but tend to be categorized as small and large lymphocytes. Lymphocytes can be identified by their very large rounded nucleus that sometimes may have a slight indentation. The nucleus actually is so large that you often will only be able to see a very small, thin ring of cytoplasm surrounding the nucleus. This is in contrast to most other human cells we’ve seen that have a smaller nucleus and a more expansive cytoplasm. Aside from the size variation, there are at least two different types of lymphocytes known as “B”lymphocytes (or “B” cells) and “T”-lymphocytes (“T” cells). A major function of “B” cells is to produce and secrete antibodies needed by the immune system to fight infections. “T” cells play a slightly different role by secreting factors which recruit phagocytes and macrophages to an infection site, while some specialized “T” cells are also able to directly attack damaged or infected cells. “B” cells and “T” cells are pretty much indistinguishable from one another on a microscope slide so don’t try to tell them apart. You may learn more about these cell types when the immune system is discussed. 2. Monocytes – relatively large agranulocytes, much less abundant than lymphocytes, but you should still be able to identify them on your slides. Monocytes have a smaller nucleus than lymphocytes which often has a large indentation and has a kidney bean appearance. Monocytes eventually will leave the bloodstream and enter tissues where they will mature into macrophages that phagocytose bacteria, viruses, and damaged cell debris. Exercise #2: Making a Differential White Blood Cell Count In this exercise, we will be performing what is known as a differential white blood cell count. The goal of this clinical test is to assess the relative numbers of different leukocytes in a given blood sample. This is an important diagnostic test since the numbers of certain leukocytes will rapidly change in response to an infection or inflammation of a tissue. Differential counts are important for the diagnosis of many diseases. A high differential count for lymphocytes may be suggestive of lymphocytic leukemia. A low differential count for neutrophils is often suggestive of radiation exposure or chemotherapy. A high differential count for eosinophils often results from intestinal parasitic infection. Allergic reactions often are associated with high differential count for basophils. A chronic infection such as tuberculosis often results in a high differential count for monocytes. Again using your blood smear slide (slide #6), you will start at one edge of the slide and systematically keep track of the numbers of different leukocytes you see. A good way to do 4 this is to count all the different cells in one field of view and then move the slide either directly across or directly down and count the cells in the adjacent field of view, making sure you are not re-counting the same cells. You can ignore all of the erythrocytes and platelets you see since we are only interested in the leukocytes. Keep moving to new adjacent regions of the slide until you have counted and identified 100 leukocytes. Keep track of the numbers in the table below. (You want a total of 100 when you are done.) The figure on page 4 illustrates a pattern for how you should scan up and down over a blood smear to identify white blood cells for this differential count. Total Number of Cells Counted:_____________ Exercise #3: Characterizing Erythrocytes and Oxygen Carrying Capacity Erythrocytes (red blood cells) contain the protein hemoglobin. There is an iron ion (Fe2+) as a co-factor at the center of the porphyrin ring for each heme. Oxygen is carried from the lungs to the body bound to the iron of the heme group. Persons who do not have very many erythrocytes or whose erythrocytes do not have enough hemoglobin cannot deliver enough oxygen to meet the demands of the body. These persons have a poor ability to deliver oxygen, grow tired quickly, and are typically diagnosed as anemic. Persons who have too many erythrocytes (polycythemia) can have so many cells that the blood becomes too viscous and forms clots that can lead to heart attack or stroke. In this exercise, we will be performing some of the very common clinical tests including determination of hematocrit, average red cell size (MCV=Mean Corpuscular Volume), hemoglobin concentration per red cell (MCH=Mean Corpuscular Hemoglobin), and the amount of hemoglobin relative to the size of the red cell (MCHC=Mean Corpuscular Hemoglobin Concentration) using your own blood. Please work in groups of 2-4 for this part of the lab. Again -- If you are not comfortable with blood donation, if you know you are sick, if you have history of fainting, if you consider yourself at risk for transmitting a blood-borne disease, etc., then please do not draw your own blood. Work to safely support your peers in the laboratory group to examine their blood. A hematocrit measures the volume of cells (formed elements) in a given sample of blood. The other measures (MCV, MCH and MCHC) are collectively called RBC indices and are values that describe the size and hemoglobin content in red cells. These measures are used in a variety of clinical diagnostics, many specific to anemia. The MCV is the average volume of a red blood cell and is a measure of red cell size. Small red blood cells have low MCV values while large red cells have high MCV values. The way this value is determined is to divide the hematocrit by the RBC count and then multiply by 10 (with units of fL). MCHC is the mean 5 corpuscular hemoglobin concentration in the red cells. This measure categorizes red blood cells based on their hemoglobin content and typically indicates if the cells might be swollen or shrunk (i.e., crenated). This value is determined by dividing the sample’s hemoglobin concentration by the hematocrit and then multiplying by 100 (with units in the g/dL). The MCH is the hemoglobin concentration of the red cells and correlates with the MCV. This value is determined by dividing the hemoglobin concentration by the red blood cell count and then multiplying by 10 (units are pg/cell). PATIENT SAMPLE ID: Measure Normal Values Hematocrit (Hct) 37 – 42 women % 42—48 men Red Cell Count from Sheet 5 x106 cells/liter HGB (hemoglobin conc.) 11.5 – 16.5 g/dL Calculations for Patient Blood (Hct/RBC)x10 = MCV MCV 80--100 fL ([Hb]/Hct)x100 = MCHC MCHC 32 – 36 g/dL ([Hb]/RBC)x10 = MCH MCH 27 – 31 pg/cell (1 liter is 1x10-6 liters) PART 1: Hematocrit In order to obtain your own blood, you will be performing a “finger stick” using a lancet with a VERY small needle. If you happen to be diabetic, you are probably a pro at this since diabetics need to test their blood sugar levels several times a day. For this exercise, you will need an alcohol swab, capillary tube with a colored band on ONE end, a lancet, and a paper towel. 1. Wash your hands in warm water and dry vigorously with a paper towel. Hold the hand that you plan to obtain blood from below your waist for a minute or so to allow more blood to flow to the tips of your fingers. 2. Using an alcohol swab, clean the side of your ring or middle finger. 3. With your hand still below your waist, prepare the lancet (instructor will demonstrate) and press it firmly against the side of your finger about halfway down your distal phalange (basically off to the side of your fingernail). 4. Lance your finger and wipe away the first small drop of blood that appears with a paper towel. 5. Have one of your team members place the capillary tubes on the edge of the table and have that person hold the tubes in place with their finger. As the second drop appears, move your finger with the drop of blood on it up to the capillary tube – it will automatically flow into the tube by capillary action. You want the tube to be about 1/2 to 2/3rds of the way full. [You may have to squeeze your 6 finger a bit to keep the blood flowing (not too hard though). NOTE: If you are planning on doing the blood typing experiment, you may want to harvest some blood at this time in order to avoid having to stick yourself a second time. For the blood typing exercise, you will want to place two small drops of blood on a clean microscope slide. It is important to space these two drops apart on the slide (one drop on each half of the slide). 6. Place your finger over the end of the capillary tube to create a seal. Now using the tray of clay, push the capillary tube into the clay to seal off the open, non-colored end of the capillary tube and place it flat on the paper towel. 7. Clean up any waste materials and disinfect contaminated objects. Do not forget to spray disinfectant on the area where you were working! Be Smart - Be Safe. In order to determine the proportion of formed elements versus plasma in your blood, we will spin the capillary tubes in a special centrifuge (instructor will do this). After 3-5 minutes of centrifugation the heavier formed elements will accumulate at the bottom of the capillary tube and a tan/yellow fluid will be seen at the top (this is the plasma). The vast majority of the formed elements seen at the bottom of the tube will be erythrocytes, with a smaller thin layer of leukocytes and platelets in between the erythrocytes and plasma. You are now ready to determine the percentage of formed elements versus plasma in your blood. This can be accomplished simply by using a millimeter ruler or a fancier hematocrit reader (instructor will demonstrate). Using a millimeter ruler: Percentage of elements in blood = Height of the layer being measured (mm formed elements or plasma) X 100 Overall height (mm) of the total sample % of formed elements = % of plasma = _______________ = hematocrit _______________ Is your hematocrit within the normal range? You may also want to try to be a little more specific and identify the proportions of individual formed elements as well. To do this, you will need to be able to identify the thinner middle layer that contains the leukocytes and platelets (often appears as a distinct layer that is not as red as the lower erythrocytes, and more reddish than the above plasma). % of erythrocytes = % of platelets and leukocytes = % of plasma = _____________ _____________ _____________ “Normal” ranges of a hematocrit are given in the reference table. Small deviations are common especially in young women. But all values may be a little low if you had to squeeze your finger to obtain a blood sample. An abnormally high hematocrit reading indicates an excessive number of erythrocytes and is known as POLYCYTHEMIA. A low hematocrit is indicative of ANEMIA. 7 Part 2: Red Cell Indices: Go up to the front desk and obtain a handout of the differential blood count for a patient. Take this sheet back to your desk and review the contents. The page can be divided into three sections: Patient Information, Tables of Results, Graphs used by machine to determine differential counts. You will want to focus your attention on the first two sections: Patient Information and Results. 1. Record your patient sample number into the blank above the table. 2. Transfer the RBC count, HGB concentration and HCT from your patient sheet into the table. As you do so note if the values are within the normal range. 3. Now use these values to calculate MCV, MCH and MCHC. Use the formulas given in the table. 4. Check with another group for their patient information and run through the calculations a second time. Microcytic anemia (low MCV) is common with chronic illness, low iron in diet or inherited anemia (e.g. thalassemia). Macrocytic anemia is present in B12 and folic acid deficiencies. Low MCHC will be common in thalassemia (a hemoglobinopathy) and/or in low iron diet conditions. MCH should correlate with MCV values for the various pathologies. Exercise #4: Determination of Blood Type (ABO and Rh-factor) In this exercise, we will be testing your blood type. Most cells in our bodies possess a characteristic group of glycoproteins on the cell membrane that specify “self” versus “non-self”. As a result our immune systems will react and attempt to destroy cells which it views as being foreign. This is a common problem when an organ from one person is transplanted into another person. These glycoproteins on the cell surface are known as ANTIGENS. Every person in this room has a slightly different set of antigens on their cells, making each of us unique. Erythrocytes also contain many antigens on their surfaces, but luckily for us there are only a couple of different antigens that are clinically most important. There are many classes of erythrocyte surface antigens, but the two most important are the ABO and Rh blood groups. The ABO blood group describes a type on antigen found on erythrocytes in human blood. A person with Type A blood will have erythrocytes that only possess the “A” antigen, Type B blood only possesses the “B” antigen, Type AB blood contains both types of antigen, and Type O blood does not possess either “A” or “B” antigens. 8 In order for our bodies to keep track of “self” versus “non-self” cells, plasma from a person with Type A blood will contain antibodies that will detect the presence of cells possessing the “B” antigen. Plasma from a person with type B blood will contain antibodies against the “A” antigen, a person with type O blood will have antibodies against both “A” and “B” antigens, and a person with type AB blood will not contain any antibodies against either antigen. This is summarized in the table to the left. Administration of the wrong blood type to a person often has devastating consequences. For example if a person with Type A blood receives Type B blood their anti-B plasma antigens will stick to the transfused Type B blood cells and cause them to clump together. This is called AGGLUTINATION. Large clumps of the transfused cells will create blood clots that quickly occlude blood vessels, often leading to death. In this exercise we will be using commercial antibodies against either the “A” antigen or “B” antigen to determine your blood type. Type A blood will form clumps in the presence of antibodies against the “A” antigen (these antibodies come from plasma of a person with Type B blood), Type B blood will clump in the presence of “B” antibodies, Type AB blood will clump in the presence of either antibody, and finally Type O blood will not clump at all in the presence of either antibody. 1. Remember to wear your gloves when dealing with someone else’s blood. 2. Using a wax pencil label one side of a clean microscope slide “A” and the other half “B” 3. Place one drop of blood on each half of the microscope slide. 4. On the “A” side, place one drop of the Anti-A antibody NEXT to the blood drop, not on top of it. Do the same on the other side with the Anti-B antibody 5. Using a clean toothpick carefully mix the drop of blood with the antibody 6. After several minutes, examine the slide to see if the blood exposed to either antibody has clumped. If after 5 minutes you cannot detect any clumping in the presence of either antibody, it can be safe to assume that you have type O blood. (The blood should not be dried on the slide.) 7. Remember to clean up your work area and place your used microscope slides in the appropriate biohazard container OR in a container of bleach/water. Since Type O blood cells do not contain either the “A” or “B” antigen, they can be transfused into any person. So, a person with Type O blood is considered a “universal donor”. Blood cells from a person with Type AB blood will have both “A” and “B” antigens on their surface. Consequently, people with Type AB blood do not have antibodies against either type of antigen. So, people with Type AB blood are considered “universal recipients” since they can safely receive type A, B, AB, or O blood! Draw your results in the circles below. Anti-A Anti-B Anti-D Control The Rh-factor is the second type of blood group antigens that you may be familiar with. This blood group is genetically determined and is distinct from the antigens of the ABO group. Like the ABO group, the frequency of occurrence of this group varies with ethnicity. The difference between the groups is that antiRh agglutinins (Anti-D) are not normally present in the blood. They are formed only in Rh(-) individuals (one 9 that would never express the antigen on the surface of their red cell) only after exposure to Rh(+) blood (red cells covered with these antigens). This means the first exposure of an Rh(-) individual to Rh(+) blood will initiate an immune response that generates antibodies. But it takes time for the body to build these new plasma proteins, these agglutinins (anti-Rh antibodies). So the person is in little danger with the first time of exposure. It is the second exposure to this different blood type that a life-threatening situation can occur. This is extremely important during pregnancy when an Rh(-) mother is carrying an Rh(+) child. The plasma proteins from the mother cross the placenta and create a condition called hemolytic disease of newborn (or erythroblastosis fetalis). In a clinical setting, this situation is prevented by the administration of Rhogam to an Rh(-) woman to suppresses Rh antibody production. In this lab, put a drop of your blood on the slide and a drop of the anti-Rh solution. You may want to hold the slide in the palm of your hand to warm the slide slightly. This enhances the pace of the reaction. If the mixture takes on a grainy appearance, the person has Rh and would be AB+, A+, B+ or type O+. If no clumping is observed, the person is Rh-negative (they do not have any Rh-factor antigens on the cell surface). 10