Anesthesia and pulmonary diseases
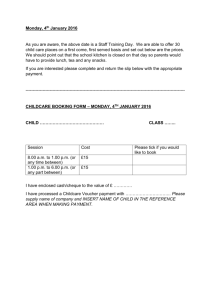
advertisement

Anesthesia and pulmonary diseases Dr abdollahi 1 Monday, March 14, 2016 Thoracic and upper abdominal operations are a particular risk for patients with chronic pulmonary disease. 2 Monday, March 14, 2016 Obstructive airway diseases Asthma and chronic obstructive pulmonary disease (COPD), the two major categories of obstructive airway disease, affect millions of Americans and cause significant morbidity and mortality worldwide. 3 Monday, March 14, 2016 Asthma is a chronic inflammatory disorder of the airways characterized by variable airflow obstruction, airway inflammation, and bronchial hyperresponsiveness. 4 Monday, March 14, 2016 In contrast, the airflow obstruction in COPD is defined as progressive and not fully reversible. The chronic inflammation of the airways and lung parenchyma in COPD is most often secondary to cigarette smoke exposure. 5 Monday, March 14, 2016 Together, asthma and COPD constitute a major public health concern, and a basic understanding of these diseases is important when caring for patients who receive anesthesia. 6 Monday, March 14, 2016 ASTHMA Asthma is a disease that is defined by the presence of: (1) Chronic inflammatory changes in the submucosa of the airways (2) Airway hyperresponsiveness (3) Reversible expiratory airflow obstruction. 7 Monday, March 14, 2016 Airway hyperresponsiveness characterizes this disease, even in asymptomatic patients, and is demonstrated by the development of bronchoconstriction in response to stimuli (allergens, exercise, mechanical airway stimulation) that have little or no effect on normal airways. Airway hyper responsiveness elicited during methacholine bronchoprovocation and airway bronchodilation in response to inhaled albuterol help diagnose asthma. 8 Monday, March 14, 2016 Clinical Symptoms The classic symptoms associated with asthma are cough, shortness of breath, and wheezing. However, symptoms of asthma may vary and range from cough with or without sputum production to chest pain or tightness. Chronic, nonproductive cough may be the sole initial complaint. 9 Monday, March 14, 2016 Some asthmatics also experience symptoms exclusively with exertion ("exercise-induced asthma"), and this diagnosis is a consideration in the pediatric and young adult population. 10 Monday, March 14, 2016 The presence or absence of wheezing on physical examination is a poor predictor of the severity of airflow obstruction. Thus, the presence of wheezing suggests airway narrowing, which should be confirmed and quantified by spirometry. 11 Monday, March 14, 2016 Degrees of obstraction are defined according to the FEV1 % predicted . Reversibility of obstruction after the administration of a bronchodilator suggests a diagnosis of asthma. 12 Monday, March 14, 2016 An increase in FEV1 % predicted of more than 12% and an increase in FEVl of greater than 0.2 L suggest acute bronchodilator responsiveness and variability in airflow obstruction. In contrast, the airways of patients with COPD do not demonstrate reversibility of airflow obstruction to the same degree as do those with asthma, a characteristic that can help distinguish these two causes of airflow obstraction. 13 Monday, March 14, 2016 14 Monday, March 14, 2016 15 Monday, March 14, 2016 During severe asthma exacerbations, intravenous therapy with glucocorticoids is the mainstay of therapy. In rare circumstances, when life-threatening status asthmaticus persists despite aggressive pharmacologic therapy, it may be necessary to consider general anesthesia (isoflurane or sevoflurane) in an attempt to produce bronchodilation. 16 Monday, March 14, 2016 Management of Anesthesia Pulmonary function studies (especially FEV1) obtained before and after bronchodilator therapy may be indicated in a patient with asthma who is scheduled for a thoracic or abdominal operation. Measurement of arterial blood gases before proceeding with elective surgery is a consideration if there are questions about the adequacy of ventilation or arterial oxygenation. 17 Monday, March 14, 2016 All asthmatics who have persistent symptoms should be treated with either inhaled or systemic corticosteroids (depending on the severity of their airflow obstruction), in addition to scheduled dose of inhaled beta agonists. Therapy should be continued throughout the perioperative period. Supplementation with cortisol may be indicated before major surgery for corticosteroid-dependent asthmatics because of suppression of the hypothalamic-pituitary-adrenal axis. 18 Monday, March 14, 2016 REGIONAL ANESTHESIA Regional anesthesia may be preferred when the surgery is superficial or involves the extremities. Notably, however, bronchospasm has been reported in asthmatics who have received spinal anesthesia, although it is generally accepted that regional anesthesia is associated with lower complication rates related to bronchospasm in the asthmatic population. 19 Monday, March 14, 2016 GENERAL ANESTHESIA The goal during induction and maintenance of general anesthesia in patients with asthma is to depress airway reflexes in order to avoid bronchoconstriction in response to mechanical stimulation of the airway. Before tracheal intubation, a sufficient depth of anesthesia should be established to minimize bronchoconstriction with subsequent stimulation of the airway. Rapid intravenous induction of anesthesia is most often accomplished with the administration of propofol or thiopental. Propofol may blunt tracheal intubation-induced bronchospasm in patients with asthma. 20 Monday, March 14, 2016 ketamine (1 to 2 mg/kg IV) is an alternative selection for rapid induction of anesthesia because its sympathomimetic effects on bronchial smooth muscle may decrease airway resistance. The increased secretions associated with the administration of ketamine, however, may limit the use of this drug in patients with asthma. Sevoflurane and isoflurane are potent volatile anesthetics that depress airway reflexes and do not sensitize the heart to the cardiac effects of the sympathetic nervous system stimulation produced by beta-agonists and aminophylline. 21 Monday, March 14, 2016 Bronchodilation with sevoflurane and isoflurane depends on the ability of the normal airway epithelium to produce nitric oxide and prostanoids. Halothane is also an effective bronchodilator but may be associated with cardiac dysrhythmias in the presence of sympathetic nervous system stimulation. Desflurane may be accompanied by increased secretions, coughing, laryngospasm, and bronchospasm as a result of in vivo airway irritation. 22 Monday, March 14, 2016 Although case reports suggest that bronchodilation follows the intravenous administration of lidocaine, the clinical significance of this response is unclear and the data are equivocal. 23 Monday, March 14, 2016 In asthmatic patients undergoing tracheal intubation, premedication with inhaled albuterol should be the first choice of therapy to prevent intubation-induced bronchoconstriction. Neuromuscular blocking drugs that are not associated with endogenous histamine release may also be used in patients with asthma . 24 Monday, March 14, 2016 Although histamine release has been attributed to succinylcholine,there is no evidence that this drug is associated with increased airway resistance in patients with asthma. 25 Monday, March 14, 2016 Intraoperatively, Pao2 and Paco2 can be maintained at normal levels by mechanical ventilation of the lungs at a slow breathing rate (6 to 10 breaths/min) to allow adequate time for exhalation, an important maneuver in patients with increased airway resistance. This slow breathing rate can usually be facilitated by the use of a high inspiratory flow rate to allow the longest possible time for exhalation. Positive end-expiratory pressure (PEEP) should be used cautiously because of the inherent, impaired exhalation in the presence of narrowed airways. 26 Monday, March 14, 2016 At the conclusion of elective surgery, the trachea may be extubated while the depth of anesthesia is still sufficient to suppress airway reflexes. After the administration of anticholinesterase drugs to reverse the effects of nondepolarizing neuromuscular blocking drugs, bronchospasm may occur but is not usual, which may reflect the protective effects (decreased airway resistance) of simultaneously administered anticholinergics. When extubation is delayed for reasons of safety until the patient is awake (possible presence of gastric contents), intravenous administration of lidocaine may decrease the likelihood of airway stimulation as a result of the endotracheal tube in an awake patient. 27 Monday, March 14, 2016 Intraoperative Bronchospasm Airway instmmentation can cause severe reflex bronchoconstriction and bronchospasm, especially in asthmatic patients with hyperactive airways. The bronchospasm that occurs intraoperatively is usually due to factors other than acute exacerbation of asthma. The frequency of perioperative bronchospasm in patients with asthma is low, especially if their asthma is asymptomatic at the time of surgery. 28 Monday, March 14, 2016 It is important to first consider mechanical causes of obstruction and inadequate levels of anesthesia before initiating treatment of intraoperative bronchospasm. Fiberoptic bronchoscopy may be useful to rule out mechanical obstraction in the tracheal tube. Asthma related bronchospasm may respond to deepening of anesthesia with a volatile anesthetic. 29 Monday, March 14, 2016 If the bronchospasm is due to asthma and persists despite an increase in the concentration of delivered anesthetic drug, albuterol should be administered by attaching a metered-dose inhaler to the anesthetic delivery system. When bronchospasm persists despite B2- agonist therapy, it may be necessary to add intravenous corticosteroids. 30 Monday, March 14, 2016 CHRONIC OBSTRUCTIVE PULMONARY DISEASE: EMPHYSEMA AND CHRONIC BRONCHITIS COPD consists of two entities, emphysema and chronic bronchitis. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines provide criteria for diagnosis and classification of severity in patients with symptoms of chronic cough, sputum production, or exposure to cigarette smoke . 31 Monday, March 14, 2016 32 Monday, March 14, 2016 Emphysema is characterized by loss of elastic recoil of the lungs, which results in collapse of the airways during exhalation and increased airway resistance. 33 Monday, March 14, 2016 Chronic bronchitis is defined by the presence of cough and sputum production for 3 months in each of 2 successive years in a patient with risk factors, most commonly cigarette smoking. It has been estimated that 25% of surgical patients smoke and a further 25% are ex-smokers, thus making COPD an important diagnosis to consider in any patient undergoing anesthesia. 34 Monday, March 14, 2016 Prediction of Postoperative Outcome The need for preoperative pulmonary function studies in patients with COPD is controversial because of the questionable correlation of these tests with postoperative outcome. Although the FEV! % predicted has been used to grade the severity of airflow obstraction, data have shown that using a multidimensional grading system to assess the respiratory and systemic extent of COPD is a better predictor of mortality than using FEV, % alone. 35 Monday, March 14, 2016 BODE index. This grading system is based on four variables1=Body mass index (B) 2=Severity of airflow obstraction (0) 3=Functional dyspnea (D) 4=Exercise capacity as assessed by the 6-minute walk test (E) 36 Monday, March 14, 2016 37 Monday, March 14, 2016 Patients with higher BODE scores were at higher risk for death. Hypercapnia and hypoxemia, as detected by arterial blood gas analysis, may also characterize patients with moderate to severe airflow obstmction. Chronic hypoxemia may lead to pulmonary hypertension and cor pulmonale. Preoperative detection plus treatment of hypoxemia-induced cor pulmonale with supplemental oxygen is an important part of preoperative management. 38 Monday, March 14, 2016 Management of Anesthesia The presence of COPD does not dictate the use of specific management of anesthesia. If general anesthesia is selected, a volatile anesthetic with humidified inhaled gases and mechanical ventilation of the lungs is useful. drugs or techniques (regional or general) for the management of anesthesia. 39 Monday, March 14, 2016 Nitrous oxide may be used, but potential disadvantages include limitation of the inhaled concentrations of oxygen and passage of nitrous oxide into emphysematous bullae. Nitrous oxide could lead to enlargement and rupture of these bullae and result in the development of tension pneumothorax. 40 Monday, March 14, 2016 Opioids are acceptable but are less ideal for maintenance of anesthesia because of the frequent need for high inhaled concentrations of nitrous oxide to ensure amnesia and associated decreases in inhaled concentrations of oxygen. To avoid this problem, administration of a volatile anesthetic at a low concentration may be substituted for nitrous oxide. Postoperative depression of ventilation may also reflect the residual effects of opioids administered intraoperatively. 41 Monday, March 14, 2016 MANAGEMENTOF VENTILATION Patients with COPD are ventilated in a manner similar to those with asthma. Small tidal volumes may be delivered to decrease the likelihood of gas trapping and barotrauma. Slow breathing rates are used to permit maximal time for exhalation. Continued tracheal intubation and mechanical ventilation of the lungs in the postoperative period are often necessary after major surgery in patients with severe emphysema. Postoperative depression of ventilation may also reflect the residual effects of opioids administered. 42 Monday, March 14, 2016 Hypercapnia secondary to chronic hypoventilation should not be corrected intraoperatively because it may then be difficult to wean the patient from mechanical ventilation as a result of the decreased respiratory drive in patients who chronically hypoventilate. 43 Monday, March 14, 2016 Pulmonary HYPERTENSION Pulmonary hypertension is defined as an elevation in mean pulmonary artery pressure to levels higher than 25 mm Hg at rest or higher than 30 mm Hg with exercise. Most cases of pulmonary hypertension are secondary to cardiac or pulmonary disease; in a minority of cases, the etiology is unknown and the pulmonary hypertension is considered primary. 44 Monday, March 14, 2016 Classification The World Health Organization has proposed a classification of pulmonary hypertension that includes pulmonary hypertension secondary to left heart disease, pulmonary disease, vascular disease, and primary pulmonary hypertension. Indicators of disease severity include dyspnea at rest, hypoxemia, syncope, metabolic acidosis indicating low cardiac output, and signs of right heart failure on physical examination (elevated jugular venous pressure, hepatomegaly, and peripheral edema). 45 Monday, March 14, 2016 Diagnostic Evaluation Diagnostic evaluation for pulmonary hypertension includes the electrocardiogram; echocardiogram; chest roentgenogram; assessment for secondary causes such as pulmonary embolism (computed tomographic angiography or ventilation/perfusion scanning), underlying pulmonary disease (pulmonary function testing), collagen vascular disease, or liver failure; and right heart catheterization. 46 Monday, March 14, 2016 Right heart catheterization is the gold standard for diagnosis because it provides data on the severity of pulmonary artery hypertension, as well as pulmonary venous pressure and cardiac output, which have prognostic significance. In addition, right heart catheterization is a necessary part of testing for vasodilator response, the first step in the algorithm to determine appropriate therapy for pulmonary artery hypertension. 47 Monday, March 14, 2016 Pathophysiology Chronic elevation of pulmonary artery pressure leads to elevated right ventricular systolic pressure, hypertrophy and dilatation of the right ventricle, and resultant right ventricular failure. Right ventricular preload and pulmonary blood flow are dependent on venous return in this setting. 48 Monday, March 14, 2016 Management of Anesthesia Intraoperative considerations for a patient with severe pulmonary hypertension include maintaining adequate preload, minimizing tachycardia and cardiac dysrhythmias that may decrease cardiac output, and avoiding arterial hypoxemia and hypercapnia, which can increase pulmonary vascular resistance (PVR). Cardiac output from a failing right ventricle is critically dependent on filling pressure from venous return and pulmonary pressure. 49 Monday, March 14, 2016 Options for treatment of pulmonary hypertension during surgery include inhaled nitric oxide (10 ppm), inhaled prostacyclin (either intermittent or continuous), and phosphodiesterase inhibitors such as milrinone. Pulmonary artery catheters have been used for intraoperative monitoring. 50 Monday, March 14, 2016 PARTURIENTS Mortality in pregnant patients undergoing vaginal delivery is near 50% and may be even higher when cesarean delivery is performed. Most often, vaginal deliveries are preferred, although regional anesthesia may be used successfully during cesarean sections. The danger of decreased venous return secondary to the sympathetic nervous system blockade produced by regional anesthesia should be considered. 51 Monday, March 14, 2016 POSTOPERATIVE PERIOD In the postoperative period, care must be taken to avoid large-volume fluid shifts, arterial hypoxemia, systemic hypotension, and hypovolemia in patients with pulmonary hypertension. Morbidity and mortality in the postoperative period are significant concerns, with possible causes including pulmonary vasospasm, increases in pulmonary artery pressure, fluid shifts, cardiac dysrhythmias, and heightened sympathetic nervous system tone. 52 Monday, March 14, 2016 OBSTRUCTIVE SLEEP APNEA Patients with obstructive sleep apnea (OSA) are at high risk for postoperative complications when undergoing general anesthesia. OSA is reported to occur in 2% of middle-aged women and 4% of middle-aged men. It is suspected, however, that up to 80% of cases of OSA are undiagnosed, thus suggesting that those with this disorder may be a significant portion of the surgical population. 53 Monday, March 14, 2016 Obesity is the most significant risk factor for the development of OSA, with a body mass index greater than 30 and a large neck circumference (>44 cm) being positively correlated with severe OSA. Obese patients with OSA or suspected OSA are at risk for complications during tracheal intubation and extubation, as well as during the postoperative period., 54 Monday, March 14, 2016 Comorbid medical illnesses such as hypertension cardiovascular disease, and congestive heart failure are also more prevalent in patients with OSA than in the general population, a fact that contributes to their postoperative morbidity. Systemic hypertension has been reported in up to 50% of patients with OSA and is independent of obesity, age, and gender. 55 Monday, March 14, 2016 Treatment of OSA by noninvasive ventilation results in better control of systemic hypertension. In addition to systemic hypertension, pulmonary hypertension is more prevalent in these patients than in the general population, One common mechanism that may explain both the systemic and pulmonary hypertension in patients with OSA is the chronic decrease in Pa02 during apneic episodes. 56 Monday, March 14, 2016 Management of Anesthesia Evaluation of the oral cavity in patients with OSA may not reveal the true nature of their pharyngeal space because increased fat deposition in the lateral pharyngeal walls has been demonstrated in these patients and shown to correlate with the severity of OSA. Neck circumference reflects pharyngeal fat deposition and correlates more strongly with the incidence and severity of OSA than general obesity dose. 57 Monday, March 14, 2016 IMPACT OF SEDATIVE DRUGS Relaxation of the upper airway musculature in response to benzodiazepines may significantly reduce the pharyngeal space and result in longer periods of hypopnea, arterial hypoxemia, and hypercapnia in patients with OSA than in the general population. 58 Monday, March 14, 2016 Any medications that depress the central nervous system must be administered carefully because airway patency and skeletal muscle tone, maintained in the awake state, may be lost at the onset of sleep. In addition, opioid analgesics may decrease the central respiratory drive and thus further add to the possible complications of sedation. 59 Monday, March 14, 2016 ANTICIPATION OF DIFFICULT AIRWAY MANAGEMENT Full preparation for difficult airway management, including the availability of orotracheal tubes of various size, a Fastrach laryngeal mask, and a fiberoptic bronchoscope, should be made before initiating direct laryngoscopy for tracheal intubation. 60 Monday, March 14, 2016 Adequate preoxygenation is necessary in obese patients with OSA because of their reduced functional residual capacity and risk for arterial hypoxemia with induction of anesthesia. Tracheal extubation should be performed only when the patient is breathing spontaneously with adequate tidal volumes, oxygenation, and ventilation. 61 Monday, March 14, 2016 MANAGEMENTIN THE POSTOPERATIVE PERIOD Respiratory depression and repetitive apnea in the postoperative period can occur in patients with OSA, especially in the setting of opioid administration for pain control. It should also be noted that in patients with OSAwho hypoventilate (obesity-hypoventilation syndrome), careful documentation of preoperative arterial blood gases is necessary to establish the baselinc set point for ventilation, an important factor whcn considering the patient's respiratory drive after extubation. 62 Monday, March 14, 2016 Relativc hyperventilation intraoperatively to maintain a norma] Paco2 in subjects who chronically hypoventilate may result in prolonged apnea when attempting extubation. 63 Monday, March 14, 2016 Smoking Cessation The risk for postoperative pulmonary complications among smokers as opposed to nonsmokers is greatly increased.The length of preoperative smoking cessation necessary to decrease this risk is not clear. It is generally accepted that the increased incidence of postoperative pulmonary complications in smokers can be reduced significantly by persuading the patient to stop smoking before surgery, although there is no consensus on the minimal or optimal duration of preoperative abstinence. 64 Monday, March 14, 2016 DISCONTINUATION OF SMOKING Smoking increases airway irritability and secretions, decreases mucociliary transport, and increases the incidence of postoperative pulmonary complications. Cessation of smoking for 12 to 24 hours before surgery decreases the level of carboxyhemoglobin, shifts the oxyhemoglobin dissociation curve to the right, and increases the oxygen available to tissues. 65 Monday, March 14, 2016 In contrast to these short-term effects, improvement in mucociliary transport and small airway function and decreases in sputum production require prolonged abstinence (8 to 12 weeks) from smoking. The incidence of postoperative pulmonary complications decreases with abstinence from cigarette smoking for 66 Monday, March 14, 2016 Nevertheless, it is useful to encourage smoking abstinence in the perioperative period, especially because smoking shortly before surgery may be associated with an increased incidence of ST-segment depression on the electrocardiogram. 67 Monday, March 14, 2016 68 Monday, March 14, 2016 Tuberculosis 69 Monday, March 14, 2016 Tuberculosis Mycobacterium tuberculosis is an obligate aerobe responsible for TB. This organism survives most successfully in tissues with high oxygen concentrations, which is consistent with the increased presentation of TB in the apices of the lungs. 70 Monday, March 14, 2016 Almost all M. tuberculosis infections result from aerosol (droplet) inhalation. It has been estimated that up to 600,000 droplet nuclei are expelled with each cough and remain viable for several days. Although a single infectious unit is capable of causing infection in susceptible individuals, prolonged exposure in closed environments is optimal for transmission of infection. 71 Monday, March 14, 2016 It is estimated that 90% of patients infected with M. tuberculosis never become symptomatic and are identified only by conversion of the tuberculin skin test. Often patients who acquire the infection early in life do not become symptomatic until much later. Patients who are HIV seropositive or immunocompromised are at much higher risk of becoming symptomatic 72 Monday, March 14, 2016 Sputum smears and cultures are also used to diagnose TB. Smears are examined for the presence of acid-fast bacilli. This test is based on the ability of mycobacteria to take up and retain neutral red stains after an acid wash. It is estimated that 50% to 80% of individuals with active TB have positive sputum smears. Although the absence of acid-fast bacilli does not rule out TB, a positive sputum culture containing M. tuberculosis provides a definitive diagnosis. 73 Monday, March 14, 2016 Health care workers are at increased risk of occupational acquisition of TB. For example, TB is twice as prevalent in physicians as in the general population. Persons involved with autopsies are uniquely at risk. 74 Monday, March 14, 2016 Diagnosis The diagnosis of TB is based on the presence of clinical symptoms, the epidemiologic likelihood of infection, and the results of diagnostic tests. Symptoms of pulmonary TB often include persistent nonproductive cough, anorexia, weight loss, chest pain, hemoptysis, and night sweats. The most common test for TB is the tuberculin skin (Mantoux) test. The skin reaction is read in 48 to 72 hours, and a positive reading is generally defined as an induration of more than 10 mm. 75 Monday, March 14, 2016 For patients with AIDS, a reaction of 5 mm or more is considered positive. The skin test is limited, and alternative screening and diagnostic tests are undergoing evaluation. The skin test is nonspecific and may be positive if people have received a bacille Calmette-Guérin vaccine or if they have been exposed to TB, or perhaps even other mycobacteria, even if there are no viable mycobacteria present at the time of the skin test. 76 Monday, March 14, 2016 Chest radiographs are important for the diagnosis of TB. Apical or subapical infiltrates are highly suggestive of infection. Bilateral upper lobe infiltration with the presence of cavitation is also common. Patients with AIDS may demonstrate a less classic picture on chest radiography, which may be further confounded by the presence of PCP. Tuberculous vertebral osteomyelitis (Pott's disease) is a common manifestation of extrapulmonary TB. 77 Monday, March 14, 2016 Anesthesiologists are at increased risk of nosocomial TB by virtue of events surrounding the induction and maintenance of anesthesia that may induce coughing (tracheal intubation, tracheal suctioning, mechanical ventilation).Bronchoscopy is a high-risk procedure associated with conversion of the tuberculin skin test in anesthesiologists. As a first step in preventing occupational acquisition of TB, anesthesia personnel should participate in annual tuberculin screening such that those who develop a positive skin test may be offered chemotherapy. The decision to take chemotherapy is not trivial as treatment for TB carries the serious toxicity. A baseline chest radiograph is indicated when a positive tuberculin skin test first manifests 78 Monday, March 14, 2016 79 Monday, March 14, 2016 80 Monday, March 14, 2016 Treatment Anti-TB chemotherapy has decreased mortality from TB by more than 90%.With adequate treatment, more than 90% of patients who have susceptible strains of TB have bacteriologically negative sputum smears within 3 months. In the United States, vaccination with bacille Calmette-Guérin is not recommended, as it may not confer immunity and confounds the diagnosis of TB. 81 Monday, March 14, 2016 Some argue that, for protection of the community, people who have positive skin tests should receive chemotherapy with isoniazid. However, the flipside is that isoniazid is a toxic drug and treatment is only strictly indicated if there are radiographic features of pulmonary TB or if there are suggestive symptoms. The toxicity of isoniazid manifests in the peripheral nervous system, liver, and possibly the kidneys. Neurotoxicity may be prevented by daily administration of pyridoxine. Hepatotoxicity is most likely to be related to metabolism of isoniazid by hepatic acetylation. Depending on the genetically determined traits, patients may be characterized as slow or rapid acetylators. Hepatitis appears to be more common in rapid acetylators, consistent with the greater production of hydrazine, a potentially hepatotoxic metabolite of isoniazid. Persistent elevations of serum transaminase concentrations mandate that isoniazid be discontinued, but mild, transient increases do not. 82 Monday, March 14, 2016 Other drugs used to treat TB include pyrazinamide, rifampicin, and ethambutol. Adverse effects of rifampicin include thrombocytopenia, leukopenia, anemia, and renal failure. Hepatitis associated with increases in serum aminotransaminase concentrations occur in approximately 10% of patients being treated with rifampicin. In order to be curative, treatment for pulmonary TB is recommended for 6 months. Extrapulmonary TB usually requires a longer course. Noncompliance with therapy contributes to the emergence of resistant TB strains. 83 Monday, March 14, 2016 Management of Anesthesia The preoperative assessment of patients considered to be at risk of TB includes a detailed history, including the presence of a persistent cough and the tuberculin status.Elective surgical procedures should be postponed until patients are no longer considered infectious. Patients are considered noninfectious if they have received antituberculous chemotherapy, are improving clinically, and have had three consecutive negative sputum smears. 84 Monday, March 14, 2016 If surgery cannot be delayed, it is important to limit the number of involved personnel, and high risk procedures (bronchoscopy, tracheal intubation, and suctioning) should be performed in a negativepressure environment whenever possible. Patients should be transported to the operating room wearing a tight-fitting N-95 face mask to prevent casual exposure of others to airborne bacilli. Staff should also wear N-95 masks. 85 Monday, March 14, 2016 If patients have TB of the cervical spine, special precautions should be taken not to injure the spine during airway manipulation. A high efficiency particulate air filter should be placed in the anesthesia delivery circuit between the Y connector and the mask, laryngeal mask airway, or tracheal tube. Bacterial filters should be placed on the exhalation limb of the anesthesia delivery circuit to decrease the discharge of tubercle bacilli into the ambient air. Sterilization of anesthesia equipment (laryngoscope blades) is with standard methods using a disinfectant that destroys tubercle bacilli. 86 Monday, March 14, 2016 Use of a dedicated anesthesia machine and ventilator is recommended. Positive-pressure ventilation has been associated with massive hemoptysis in a patient with old pulmonary TB leading to the recommendation that maintenance of spontaneous breathing may be indicated in selected patients. Postoperative care should, if possible, take place in an isolation room, preferably with negative pressure. 87 Monday, March 14, 2016 lists important considerations in regard to tuberculosis. 1. 2. 3. 4. 5. 88 With the acquired immunodeficiency syndrome epidemic, tuberculosis is reemerging worldwide. Multidrug resistant and extensively drug-resistant strains are resistant to therapy and have increased virulence. Symptoms include persistent cough, anorexia, weight loss, chest pain, hemoptysis, and night sweats. Anesthesiologists are at increased risk of nosocomial tuberculosis. Treatment for pulmonary tuberculosis is recommended for 6 months. Monday, March 14, 2016 6. Noncompliance with therapy contributes to the emergence of resistant tuberculosis strains. 7. Staff and patients should wear N-95 masks. 8. A dedicated anesthesia machine and ventilator should ideally be used. 9. Postoperative care should take place in an isolation room with negative pressure. 89 Monday, March 14, 2016 UPPER RESPIRATORY TRACT INFECTIONS Patients may arrive at the hospital for elective tonsillectomy and adenoidectomy with an acute upper respiratory tract infection. Surgery for these patients is usually postponed until resolution of the upper respiratory tract infection, which is typically 7 to 14 days. Laryngospasm with airway manipulation may be more likely to occur in the presence of an upper respiratory tract infection. 90 Monday, March 14, 2016 URI has diffuse effects on the respiratory epithelium, mucociliary function, and airway reactivity. These effects combine to provide the potential for an increased risk for anesthesia in specific clinical settings. If the planned surgical procedure is short and airway support is restricted to the use of a facemask, the risk for an adverse respiratory event is minimal. 91 Monday, March 14, 2016 If an endotracheal tube is required, the risk for an adverse respiratory event is increased (up to 10- fold) over that in an infant without a URI whose trachea is not intubated. An LMA seems to be associated with risks midway between those associated with a facemask and those with an endotracheal tube.Younger age plus a ORI seems to be associated with an increased risk from anesthesia. URIs develop recurrently in 1- to 6-year-olds, and if reactive airways accompany the infection, the effect on the airway persists for 2 to 6 weeks. 92 Monday, March 14, 2016 Ultimately, the preoperative evaluation must weigh the inconvenience of rescheduling against ignoring possible risks. If the decision is to proceed with elective surgery, the infant should be considered to have reactive airways. 93 Monday, March 14, 2016 The decision to cancel surgery on a child with an uncomplicated ORI always requires assessment from the viewpoint of a specific patient and family, a specific procedure, and a specific surgeon. A strict protocol for when to cancel surgery is impractical. The patient's age, medical and anesthetic history, current physical examination, planned surgery (placement of tympanostomy tubes versus surgery for craniofacial repair), and anticipated postoperative care (need for mechanical ventilatory support) must be analyzed. 94 Monday, March 14, 2016 Ultimately, the preoperative evaluation must weigh the inconvenience of rescheduling against ignoring possible risks. If the decision is to proceed with elective surgery, the infant should be considered to have reactive airways. 95 Monday, March 14, 2016 Epiglottitis Acute epiglottitis is an infectious disease caused by Haernopbilus infiuenzae type B. It can progress rapidly from a sore throat, to airway obstruction, to respiratory failure and death if proper diagnosis and treatment are delayed. Patients are usually between 2 and 7 years of age, although epiglottitis has been reported in younger children and adults. 96 Monday, March 14, 2016 Characteristic signs and symptoms of acute epiglottitis include (1) a sudden onset of fever, dysphagia, drooling, thick muffled voice, and preference for the sitting position with the head extended and leaning forward (2) retractions, labored breathing, and cyanosis when respiratory obstruction is present. 97 Monday, March 14, 2016 Treatment Direct visualization of the epiglottis should not be attempted in an awake patient because it could lead to airway compromise and death. Interactions with the patient should be kept to a minimum. Stimulation of the patient or the onset of struggling during attempted treatment procedures may result in exacerbation of the airway obstruction. Induction of anesthesia is often accomplished with the inhalation of sevoflurane (alternatively, halothane) while maintaining spontaneous ventilation. 98 Monday, March 14, 2016 It is important to secure the airway without stimulating the reactive airway. An emergency airway cart and tracheostomy tray should be available and open, with appropriate personnel present should an emergency surgical airway be needed. 99 Monday, March 14, 2016 Postoperative management takes place in the intensive care unit and consists of continued observation and radiographic confirmation of tracheal tube placement. Tracheal extubation is usually attempted 48 to 72 hours later when a significant leak around the endotracheal tube is present and visual inspection of the larynx by flexible fiberoptic bronchoscopy confirms a reduction in swelling of the epiglottis and surrounding tissue. 100 Monday, March 14, 2016 101 Monday, March 14, 2016