Chronic Renal Failure(CRF)
advertisement

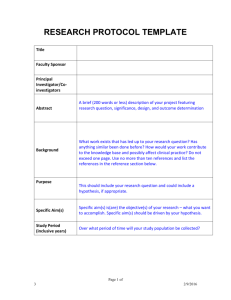
Chronic Renal Failure(CRF) Shanghai Ruijin Hospital affiliated to Shanghai Second Medical University, Dept.of Nephrology Qian Ying CRF Definition: final stage of numorous renal diseases resulting from progressive loss of glomerular, tubular and endocrine function in both kidneys. This leads to disturbed excretion of end products of metabolism disturbed elimination of electrolytes and water disturbed secretion of hormones(eg. Erythropoietin, renin, prostaglandins, active form of vitamin D) CRF Regional and racial incidence of CRF • Britain 70-80/per million • China 100/per million • USA 60-70/per million CRF Etiology overseas diabetic nephropathy, hypertensive glomerular sclerosis, chronic GN china chronic GN, obstructive nephropathy, diabetic nephropathy CRF Pathogenesis (unknown) uremic toxins • small molecular weight: urea, creatinine, uric acid, guanidine, phenol, amines, indoles • middle molecular weight: PTH • large molecular weight: 2-MG CRF Major hypothesis • intact nephron hypothesis final common pathway (hemodynamically mediated glomerular injury) CRF glomerular injury adaptive single nephron hyperfiltration glomerular capillary plasma flow, hydraulic pressure Intact nephron hypertrophy and sclerosis CRF • Trade-off hypothesis CRF Calcium phostate PTH SHPT bone,heart,blood,nerves injury • Hypertension and compensatory hypertrophy of glomeruli • Hypermetabolism of renal tubuli • cytokines and lipid disturbances CRF • Stage 1: the normal stage of renal function GFR>70 ml/min, BUN<6.5 mmol/L, Scr<110 umol/L • Stage 2:imcompensation stage of renal GFR 50-70 ml/min, 6.5 <BUN< 9 mmol/L, 110 <Scr< 178 umol/L no any signs and symptoms except for the underlying disorders CRF • Stage 3: azotemic stage GFR<50 ml/min,BUN>9 mmol/L Scr>178 umol/L there may be slight fatigue,anorexia and anemia • Stage 4: uremic stage GFR<25 ml/min,BUN>20 mmol/L Scr>445 umol/L a constellation of uremic syndrome may appear in this stage CRF Signs and symptoms of uremia General Gastrointestinal tract Neuropathy Bone Blood Electrolyte disorders Heart Skin Muscles Infection Lung Endocrine and metabolic CRF CRF Cardiovascular disorders • Hypertension 80% Water and sodium retention Alterations of RAAS Glomerular capillary pressure> systemic arterial pressure CRF Atherosclerosis hypertriglycerid, hypercholesterolemia vascular calcification inadequate perfusion of the limbs CRF Pericarditis • Uremic • Dialysis associated Signs and symptoms • Chest pain • Friction rub • Pericardial effusion and tamponade CRF Hematologic disorders • Anemia, bleeding, granulocyte, platelet dysfunction Causes: • • • • • • Relative deficiency of erythropoietin Decreased erythropoietin production Reduced red cell survival Increased blood loss Folate and Iron deficiency Hypersplenism CRF Neuropathy • Central nervous system Tiredness, insomnia, agitation, irritability, depression, regression, rebellion • Peripheral nervous system Restless leg syndrome the patient’s legs are jumpy during the night, painful paresthesis of extremities, twitching, loss of deep tendon reflexes , musclar weakness, sensory deficits CRF Renal osteodystrophy Type I: high turn-over bone disease Type II: low turn-over bone disease Type III: mixture CRF Causes of renal osteodystrophy • 1, 25(OH)2D3 • calcium phosphate • SHPT • malnutrition • iron and aluminum overload CRF CRF Water, electrolyte and acid-base disturbances • potassium sodium • calcium phosphate • Metabolic acidosis • magnesium CRF Diagnosis of hyperkalemia • Plasma K>5.5mmol/L • Plasma K>7.0mmol/L cardiac arrest CRF CRF Causes of hyperkalemia Increased intake: rapid adminstration of K by mouth or intravenously Drugs containing K(chinese medical herbs) Impaired excretion Chronic renal failure(GFR<15ml/min) CRF Causes of hyperkalemia Shift of K out of cells Metabolic acidosis Tissue breakdown Bleeding into soft tissues, GI tract or body cavities Hemolysis Catabolic states CRF Diagnosis: • Case history • Physical examination • Laboratory studies including urinalysis , renal function tests , biochemical analysis of blood • X-ray, ultrosound and radiorenogram CRF Treatment of CRF Non-dialysis dialysis CRF Non-dialysis • Diet therapy • Treatment of reversible factors • Treatment of the underlying disease • Treatment of complcations of uremia • Chinese medical herbs CRF Diet therapy • Protein restriction (0.5-0.8mg/kg/d) • Adequte intake of calories(30-35kcal/kg/d) • Fluid intake:urine volume +500ml • Low phosphate diet(600-1000mg/d) • Supplement of EAA(ketosteril) CRF Reversible factors in CRF • Hypertension • Reduced renal perfusion (renal artery stenosis, hypotension , sodium and water depletion, poor cardiac function) • Urinary tract obstruction • Infection • Nephrotoxic medications • Metabolic factors(calcium phosphate products ) CRF Management of complications of uremia Hyperkalemia • Identify treatable causes • Inject 10-20ml 10% calcium gluconate • 50% gluconate 50-100ml i.v.+insulin 6-12u • Infusion 250ml 5% sodium bicarbonate • Use exchage resin • Hemodialysis or peritoneal dialysis CRF Cardiac complications • Diuretics • Digitalis • Treat hypertension • dialysis CRF Antihypertensive therapy Target blood pressure 130/85mmHg • ACE inhibitors • Angiotension II receptor antagonists • Calcium antagonists • -blockers • vesodialators CRF Treatment of anemia • Recombinant human erythropoietin(rhEPO) • 2000-3000u BIW H • Target hemoglobin 10-12g/L • hemotocrit 30-33% CRF Side effects of rhEPO • Hypertension • Hypercoagulation • Thrombosis of the AVF CRF rhEPO resistant • Iron deficiency • Active inflamation • Malignancy • Secondary hyperparathyroid • Aluminum overload • Pure red cell aplasia CRF Treatment of renal osteodystropy Low phosphate diet Calcium carbonate (1-6g/d) Vitamin D (0.25ug/d for prophylactic, 0.5ug/d for symptomatic, pulse therapy 2-4ug/d for severe cases) parathyroidectomy CRF Renal replacement therapy • Hemodialysis • Peritoneal dialysis • Renal transplantation CRF Indications of HD • GFR<10ml/min • the uremic syndrome • hyperkalemia • acidosis • fluid overload Hemodialysis Hemodialysis 弥散 Diffussion 渗透 Dialysis Hemodialysis 超滤 Ultrofiltration 正压 对流 Conduction 负压 Contraindications of HD • • • • • Shoke Severe caidioc complications Severe bleeding malignency , sepsis poor condition in vascular system CRF Indications of CAPD child old people with cardiovascular disease dibetic nephropathy trouble of AVF 治疗 Choice of HD or CAPD HD PD young no eldly yes Blood No bleeding Bleeding Vascular condition good poor Ecnomic situation better poor Age Cardiovascular disease CRF Indications of RT • maitenance dialysis patients without contraindications of RT • age<60 years CRF Prognosis 5-year survival Home HD 80% RT 60% Hospital HD 60% CAPD 50% CRF Drug dosing in CRF Redused dose and adminstration interval Ccr(ml/min)=[(140-years old)×body weight(kg)]/[72×Scr(mg/dl)] for female: ×0.85 Acute heart failure in uremia (key treatment?) • • • • Diuretics Digitalis Treat hypertension dialysis