Debra Ness - Consumer

Achieving Affordable Health Care:
The Role of Cost and Resource Use
Measures
Part I: Understanding How Cost and
Resource Use are Measured
Invitational Working Session
November 17, 2011
Agenda
• Overview
– Debra Ness, President, National Partnership for Women &
Families and Co-Chair, Consumer-Purchaser Disclosure Project
– Bill Kramer, Executive Director National Health Policy, Pacific
Business Group on Health and Co-Chair, Consumer-Purchaser
Disclosure Project
• Commentators
– Sue Knudson, Vice President, Health Informatics, HealthPartners
– Mark Rattray, MD, President, CareVariance LLC
– Phyllis Torda, Vice President for Strategy and the Quality
Solutions Group, National Committee for Quality Assurance
• Discussion and Wrap-Up
To Infinity, and Beyond
• Employer-sponsored health insurance premiums have more than doubled in the last 9 years, 3 times faster than cumulative wage increases.
(Kaiser Family Foundation & Health
Research and Educational Trust, 2008)
• Health care costs doubled from 1996 to 2006, and are projected to rise to 25% of GDP in 2025 and 49% in 2082.
(Congressional Budget Office, Jan 31 2008)
• From 2000 to 2008, the percentage of employees with an annual deductible greater than $1000 increased from
1% to 18%. Among small businesses, more than one in three workers must spend at least $1000 out of pocket before their health benefits kick in.
(Kaiser Family Foundation &
Health Research and Educational Trust, 2008)
The Triple Aim:
• Better Care: improving the individual experience of care.
• Better Health: improving the health of populations.
• Lower Costs: reducing the per capita costs of care for populations.
Obstacles: supply-driven demand, new technologies with limited impact on outcomes, physician-centric care, limited performance information and incentives to spur performance improvement.
Are We There Yet?
• A variety of models are being tried. How will we recognize improvement?
Measurement!
• By measuring health care outcomes and costs, we can identify what is working and what is not.
• Measurement will also encourage improvement.
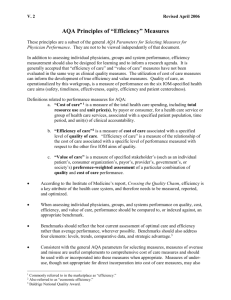
Overview: Cost Measurement
• Quality: “The degree to which health care services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.” IOM, 1990.
• Value: measure of stakeholder’s preference-weighted assessment of a particular combination of quality and cost of care performance. Need to measure quality and cost. AQA Alliance.
• Efficiency: the use of resources to get the best value.
Measurement Movers and Shakers
• The Center for Medicare and Medicaid Services (CMS)
• The Agency for Healthcare Research and Quality (AHRQ)
• The Medicare Payment Advisory Commission (MedPAC)
• The National Quality Forum (NQF)
• The Joint Commission
• The National Committee for Quality Assurance (NCQA)
• AQA Alliance (AQA)
• Hospital Quality Alliance (HQA)
• The Quality Alliance Steering Committee (QASC)
• Physician’s Consortium for Performance Improvement (PCPI)
• The Leapfrog Group
About The Consumer-Purchaser Disclosure Project
The Consumer-Purchaser Disclosure Project is an initiative that is improving health care quality and affordability by advancing public reporting of provider performance information so it can be used for improvement, consumer choice, and as part of payment reform. The Project is a collaboration of leading national and local employer, consumer, and labor organizations whose shared vision is for Americans to be able to select hospitals, physicians, and treatments based on nationally standardized measures for clinical quality, consumer experience, equity, and efficiency. The Project is funded by the Robert Wood
Johnson Foundation along with support from participating organizations.
For more information go to http://healthcaredisclosure.org
Or Contact:
Dena B. Mendelsohn, JD, MPH
Policy Analyst
Consumer-Purchaser Disclosure Project dmendelsohn@pbgh.org