CMS Quality Strategy and Quality Measurement
advertisement

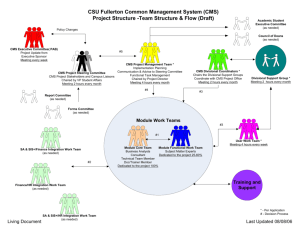
CMS Quality Strategy and Quality Measurement AHA Annual Meeting Dr. Patrick Conway, M.D., MSc CMS Chief Medical Officer and Deputy Administrator for Innovation and Quality Director, Center for Medicare and Medicaid innovation Director, Center for Clinical Standards and Quality May 5, 2014 The Six Goals of the CMS Quality Strategy 1 Make care safer by reducing harm caused in the delivery of care 2 5 6 Strengthen person and family engagement as partners in their care 3 Promote effective communication and coordination of care 4 Promote effective prevention and treatment of chronic disease Work with communities to promote healthy living Make care affordable INFORMATION NOT RELEASABLE TO THE PUBLIC UNLESS AUTHORIZED BY LAW: This information has not been publicly disclosed and may be privileged and confidential. It is for internal government use only and must not be disseminated, distributed, or copied to persons not authorized to receive the information. Unauthorized disclosure may result in prosecution to the full extent of the law. CMS framework for measurement maps to the six national priorities Greatest commonality of measure concepts across domains Care coordination Clinical quality of care •Transition of care measures •Admission and readmission measures •Other measures of care coordination •HHS primary care and CV quality measures •Prevention measures •Setting-specific measures •Specialty-specific measures Person- and Caregivercentered experience and engagment •CAHPS or equivalent measures for each settings •Shared decision-making Population/ community health •Measures that assess health of the community •Measures that reduce health disparities •Access to care and equitability measures Efficiency and cost reduction Safety •Healthcare Acquired Infections •Healthcare acquired conditions • Harm •Spend per beneficiary measures •Episode cost measures •Quality to cost measures – Measures should be patientcentered and outcomeoriented whenever possible – Measure concepts in each of the six domains that are common across providers and settings can form a core set of measures CMS Quality Strategy: Foundational Principles Eliminate disparities Strengthen infrastructure and data systems Enable local innovations Foster learning organizations 4 CMS Vision for Quality Measurement • Align measures: – With NQS and 6 measure priorities/domains. – With external stakeholders (private payers, states) – Across CMS programs whenever possible • Create parsimonious or cores measure sets • Implement measures filling critical gaps (patientreported outcomes, care coordination, appropriate use, etc.) in rapid cycle • Remove “topped-out” measures. • Goal is improvement over time 5 Future Hospital Quality Measurement • Robust quality measures covering the 6 goals from the CMS Quality Strategy • Adopt Quality Measurement across care settings • Integrated quality reporting and pay-forperformance programs • Submit once and fulfill multiple quality programs 6 Hospital Value Based Purchasing • Additional stakeholder input – Pre-rulemaking process to allow stakeholders to submit measure concepts and given input – Enables CMS to more quickly target measurement goals identified in Quality Strategy • Evolution of Quality Measures/Domains – Expanding measures’ focus to outcomes, patient experience and efficiency – New quality domains for FY 2017 based on Quality Strategy – Monitoring and evaluation efforts ongoing 7 Hospital Readmission Reduction Program • 5 condition specific measures – AMI, HF, PN, COPD, THA/TKA • Strive to be parsimonious – All Cause Hospital Wide Readmissions (HWR) measure • Stakeholder support for this measure recognized by CMS • Likely lack statutory authority to implement measure as currently designed. 8 Hospital Acquired Conditions Reduction Program • FY 2017: 5 Hospital Associated Infections will be implemented in addition to PSI-90 – CLABSI, CAUTI, SSI, MRSA, C. difficile • FY 2015 IPPS/LTCH PPS proposed rule – Seeking stakeholder input on electronically specified measures of all-cause harm 9 Future State for CMS Programs • Improve quality of care using: – Robust quality measures. – Timely feedback to providers. – EHR’s in a meaningful manner. • Minimize reporting burden by: – Synchronizing performance and reporting periods. – Reduce number of required submissions by professionals for eCQM data to one. • Maximize efficiency by: – Using eCQM reported data for multiple quality programs. 10 The Future of Quality Measurement for Improvement and Accountability • Meaningful quality measures increasingly need to transition away from setting-specific, narrow snapshots • Reorient and align measures around patient-centered outcomes that span across settings • Measures based on patient-centered episodes of care • Capture measurement at 3 main levels (i.e., individual clinician, group/facility, population/community) • Example gaps areas to be filled: patient reported outcomes, care coordination, patient engagement, efficiency, etc • Why do we measure? – Improvement Source: Conway PH, Mostashari F, Clancy C. The Future of Quality Measurement for Improvement and Accountability. JAMA 2013 June 5; Vol 309, No. 21 2215 - 2216 Contact Information Dr. Patrick Conway, M.D., M.Sc. CMS Deputy Administrator for Innovation and Quality and CMS Chief Medical Officer 410-786-6841 patrick.conway@cms.hhs.gov 12