grade - Cochrane Community
advertisement

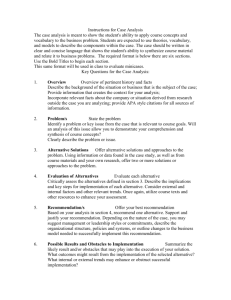
Holger Schünemann, MD, PhD Professor and Chair, Dept. of Clinical Epidemiology & Biostatistics Professor of Medicine Michael Gent Chair in Healthcare Research McMaster University, Hamilton, Canada HOW GRADE COULD HELP TO IMPLEMENT THE EVIDENCE Content Pulmonary rehabilitation compared to usual community care for COPD with recent exacerbation Bibliography: Puhan M, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2010, Issue 11. Outcomes No of Participants (studies) Follow up Quality of the evidence (GRADE) Relative effect (95% CI) Hospital admission 250 (6 studies) 3-18 months ⊕⊕⊕⊕ HIGH OR 0.22 (0.08 to 0.58) Mortality 110 (3 studies) 3-48 months ⊕⊕⊕⊝ MODERATE2 due to imprecision OR 0.28 (0.1 to 0.84) Anticipated absolute effects Risk with Usual community care Risk difference with Pulmonary rehabilitation (95% CI) 405 per 1000 275 fewer per 1000 (from 122 fewer to 353 fewer) Low1 100 per 1000 70 fewer per 1000 (from 15 fewer to 89 fewer) High1 Systematic Reviews & GRADE 500 per 1000 281 fewer per 1000 (from 43 fewer to 409 fewer) Quality of life (CRQ) dyspnea Chronic Respiratory Questionnaire3. Scale from: 1 to 7. 258 (5 studies) 12 and 76 weeks ⊕⊕⊕⊝ MODERATE4 due to imprecision The mean quality of life (sgrq) total in the control groups was 3.1 The mean quality of life (crq) dyspnea in the intervention groups was 0.97 higher (0.35 to 1.58 higher) Quality of life (SGRQ) total St George's Respiratory Questionnaire5. Scale from: 0 to 100. 127 (3 studies) 12 and 26 weeks ⊕⊕⊕⊝ MODERATE4 due to imprecision The mean quality of life (sgrq) total in the control groups was 50 The mean quality of life (sgrq) total in the intervention groups was 9.88 lower (5.37 to 14.4 lower) Ambulation (as measured by 6 min walking distance) distance in meters 6 299 (6 studies) 1 - 208 weeks7 ⊕⊕⊕⊝ MODERATE4,8 due to imprecision Resource use not reported - - The mean ambulation (as measured by 6 min walking distance) in the intervention groups was 77.7 higher (12.21 to 143.2 higher) - See footnote Evidence & judgments See footnote Recommendation, health policy & implementation Content Examples and summary from leading/co-leading 15 guideline projects • 11 World Health Organization • World Allergy Organization, Allergic Rhinitis in Asthma, American Thoracic Society Systematic Evidence & Recommendation, (2) Reviews & GRADE judgments health policy & Pulmonary rehabilitation compared to usual community care for COPD with recent exacerbation Bibliography: Puhan M, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2010, Issue 11. Outcomes No of Participants (studies) Follow up Quality of the evidence (GRADE) Relative effect (95% CI) Hospital admission 250 (6 studies) 3-18 months ⊕⊕⊕⊕ HIGH OR 0.22 (0.08 to 0.58) Mortality 110 (3 studies) 3-48 months ⊕⊕⊕⊝ MODERATE2 due to imprecision OR 0.28 (0.1 to 0.84) Anticipated absolute effects Risk with Usual community care Risk difference with Pulmonary rehabilitation (95% CI) 405 per 1000 275 fewer per 1000 (from 122 fewer to 353 fewer) Low1 100 per 1000 70 fewer per 1000 (from 15 fewer to 89 fewer) High1 500 per 1000 281 fewer per 1000 (from 43 fewer to 409 fewer) Quality of life (CRQ) dyspnea Chronic Respiratory Questionnaire3. Scale from: 1 to 7. 258 (5 studies) 12 and 76 weeks ⊕⊕⊕⊝ MODERATE4 due to imprecision The mean quality of life (sgrq) total in the control groups was 3.1 The mean quality of life (crq) dyspnea in the intervention groups was 0.97 higher (0.35 to 1.58 higher) Quality of life (SGRQ) total St George's Respiratory Questionnaire5. Scale from: 0 to 100. 127 (3 studies) 12 and 26 weeks ⊕⊕⊕⊝ MODERATE4 due to imprecision The mean quality of life (sgrq) total in the control groups was 50 The mean quality of life (sgrq) total in the intervention groups was 9.88 lower (5.37 to 14.4 lower) Ambulation (as measured by 6 min walking distance) distance in meters 6 299 (6 studies) 1 - 208 weeks7 ⊕⊕⊕⊝ MODERATE4,8 due to imprecision Resource use not reported - - The mean ambulation (as measured by 6 min walking distance) in the intervention groups was 77.7 higher (12.21 to 143.2 higher) - See footnote See footnote implementation Guideline development Process Critical Outcome Critical Outcome Important Outcome Not High Moderate Low Very low Summary of findings & estimate of effect for each outcome Systematic review Grade down Outcome Grade up P I C O Randomization increases initial quality 1. Risk of bias 2. Inconsistency 3. Indirectness 4. Imprecision 5. Publication bias 1. Large effect 2. Dose response 3. Confounders Guideline development Formulate recommendations: • For or against (direction) • Strong or conditional/weak (strength) By considering: Quality of evidence Balance benefits/harms Values and preferences Revise if necessary by considering: Resource use (cost) Grade overall quality of evidence across outcomes based on lowest quality of critical outcomes • • • • “We recommend using…” “We suggest using…” “We recommend against using…” “We suggest against using…” Outcome generation and selection • Multidisciplinary panels – Researchers, epidemiologists, public health officers, methodologists, patient representatives… • Delphi process – 3 rounds 1. List of possible outcomes from literature – Panel members review and add 2. List of all outcomes grouped by theme – Panel members rate importance 3. Final agreement and results Outcomes for screening on a scale of 1 (not important) to 9 (critical) Mortality from cervical cancer Cervical cancer Incidence Detected CIN 2,3 Major Infections (requiring hospital admission and antibiotics, e.g. PID) Maternal bleeding Premature delivery Fertility Identification of STIs (benefit) Minor infections (requiring outpatient treatment only) 8.2 8.3 7. 9 6.0 5.8 5.7 5.4 5.0 3.8 Challenges and advantages of this approach • Often starting with many outcomes • Experts initially focused on what they know from research studies • Requires detailed explanations • ↓ Participation of panel members • Perspective taken • Complete • Everyone involved – Independent ratings • Numerical estimates • Well documented and kept record • Transparent • Reduces work WHO influenza guidelines • New guideline on pharmacological management of influenza – Previously few randomized trials • Low quality evidence for many outcomes (imprecision) • Industry sponsored – publication bias • Not all outcomes • Review of observational studies – To inform guidelines Methods • Standard systematic review – MEDLINE, EMBASE, CENTRAL, CINAHL, SIGLE, the Chinese Biomedical Literature Database, Panteleimon and LILACS for relevant studies up to November 2010 – contacted pharmaceutical companies and international agencies – RevMan 5.1 • 10 PICO → recommendations approach – Outcomes determined through Delphi process previously • QoE according to GRADE approach – GRADEpro (www.gradeworkinggroup.org) – Risk of bias using modified Ottawa Newcastle scale Results Question: Should oseltamivir vs. no antiviral treatment be used for influenza (follow-up: 30 days)? Quality assessment Participants Risk of bias Inconsistency Indirectness Imprecision Publication bias (studies) Summary of Findings Overall quality of evidence Study event rates (%) With no antiviral treatment Relative effect Anticipated absolute effects With oseltamivir (95% CI) Risk with no antiviral treatment Absolute effect with Oseltamivir (95% CI) Mortality 681 (3 studies) no serious no serious no serious no serious undetected1 ⊕⊕⊝⊝ risk of bias inconsistency indirectness imprecision LOW1 1557 (9 studies) serious2 59/242 (24.4%) no serious no serious no serious undetected1 ⊕⊝⊝⊝ 61/320 inconsistency indirectness imprecision VERY LOW1,2 (19.1%) due to risk of bias 31/439 (7.1%) adj OR 0.23 (0.13 to 0.43) 240 deaths per 1000 172 fewer deaths per 1000 (from 120 to 201 fewer) 228/1237 (18.4%) OR 0.51 (0.23 to 1.14)3 240 deaths per 1000 101 fewer deaths per 1000 (from 172 fewer to 25 more) Hospitalisation 150710 (5 studies) no serious no serious no serious no serious undetected4 ⊕⊕⊝⊝ risk of bias inconsistency indirectness imprecision LOW4 242762 (6 studies) serious2 1238/100585 431/50125 (1.2%) (0.86%) adj OR 0.75 (0.66 to 0.89) 12 hospitalisations per 1000 3 fewer hospitalisations per 1000 (from 1 to 4 fewer) 1086/96352 (1.1%) OR 0.75 (0.66 to 0.86) 12 hospitalisations per 1000 3 fewer hospitalisations per 1000 (from 2 to 4 fewer) no serious no serious undetected1 ⊕⊝⊝⊝ indirectness imprecision VERY LOW1,6 due to risk of bias, inconsistency 200/1032 (19.4%) - - 647/50017 (1.3%) adj OR 0.83 (0.59 to 1.16) 21 pneumonias per 1000 4 fewer pneumonias per 1000 (from 9 fewer to 3 more) 1273/99020 (1.3%) OR 0.64 (0.46 to 0.88) 20 pneumonias per 1000 7 fewer pneumonias per 1000 (from 2 to 10 fewer) no serious no serious no serious undetected4 ⊕⊝⊝⊝ 1738/ inconsistency indirectness imprecision VERY LOW2,4 146410 due to risk of bias (1.2%) ICU admissions/mechanical ventilation/respiratory failure 1032 Serious5 (6 studies5) serious6 Complications - Pneumonia 150466 (3 studies) no serious serious6 risk of bias no serious no serious undetected4 ⊕⊝⊝⊝ indirectness imprecision VERY LOW4,6 due to inconsistency 265276 (6 studies) serious2 no serious no serious undetected4 ⊕⊝⊝⊝ 3244/ indirectness imprecision VERY LOW2,4,6 166256 due to risk of bias, (2%) inconsistency serious6 2111/ 100449 (2.1%) Content Pulmonary rehabilitation compared to usual community care for COPD with recent exacerbation Bibliography: Puhan M, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2010, Issue 11. Outcomes No of Participants (studies) Follow up Quality of the evidence (GRADE) Relative effect (95% CI) Hospital admission 250 (6 studies) 3-18 months ⊕⊕⊕⊕ HIGH OR 0.22 (0.08 to 0.58) Mortality 110 (3 studies) 3-48 months ⊕⊕⊕⊝ MODERATE2 due to imprecision OR 0.28 (0.1 to 0.84) Anticipated absolute effects Risk with Usual community care Risk difference with Pulmonary rehabilitation (95% CI) 405 per 1000 275 fewer per 1000 (from 122 fewer to 353 fewer) Low1 100 per 1000 70 fewer per 1000 (from 15 fewer to 89 fewer) High1 Systematic Reviews & GRADE 500 per 1000 281 fewer per 1000 (from 43 fewer to 409 fewer) Quality of life (CRQ) dyspnea Chronic Respiratory Questionnaire3. Scale from: 1 to 7. 258 (5 studies) 12 and 76 weeks ⊕⊕⊕⊝ MODERATE4 due to imprecision The mean quality of life (sgrq) total in the control groups was 3.1 The mean quality of life (crq) dyspnea in the intervention groups was 0.97 higher (0.35 to 1.58 higher) Quality of life (SGRQ) total St George's Respiratory Questionnaire5. Scale from: 0 to 100. 127 (3 studies) 12 and 26 weeks ⊕⊕⊕⊝ MODERATE4 due to imprecision The mean quality of life (sgrq) total in the control groups was 50 The mean quality of life (sgrq) total in the intervention groups was 9.88 lower (5.37 to 14.4 lower) Ambulation (as measured by 6 min walking distance) distance in meters 6 299 (6 studies) 1 - 208 weeks7 ⊕⊕⊕⊝ MODERATE4,8 due to imprecision Resource use not reported - - The mean ambulation (as measured by 6 min walking distance) in the intervention groups was 77.7 higher (12.21 to 143.2 higher) - See footnote Evidence & judgments See footnote • Systematic and transparent approach • Transparently lay out rationale for recommendations • Manage COI Recommendation, health policy & implementation Judgments/explanations 1 Although we did not downgrade, publication bias cannot be excluded and is of concern. 2 Studies not adjusted for potential confounding factors. 3 Significant differences in effect for pandemic versus seasonal influenza (see subgroup analyses table). 4 Publication bias a concern since large studies had forprofit funding and weighted heavily in analyses. 5 No independent comparison group. 6 High heterogeneity among studies. 7 Measured in select patients in trials. Getting from evidence to recommendations - GRADE Recommendations are based on judgments: – Quality of evidence (confidence in estimates of effect) – Balance between benefits and downsides – Values and preferences – Resource use But judgments need to be based on the best available evidence and transparent Balancing desirable and undesirable consequences ↑ herd immunity Conditional Strong ↓ Morbidity ↓ Death ↑ QoL For ↑ Resources ↑ Allergic reactions ↑ Nausea ↑ Local skin reactions Against Balancing desirable and undesirable consequences Conditional Strong For Against Balancing desirable and undesirable consequences Conditional Strong For Against Balancing desirable and undesirable consequences Conditional Strong For Against Balancing desirable and undesirable consequences Conditional Strong For Against Content Pulmonary rehabilitation compared to usual community care for COPD with recent exacerbation Bibliography: Puhan M, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2010, Issue 11. Outcomes No of Participants (studies) Follow up Quality of the evidence (GRADE) Relative effect (95% CI) Hospital admission 250 (6 studies) 3-18 months ⊕⊕⊕⊕ HIGH OR 0.22 (0.08 to 0.58) Mortality 110 (3 studies) 3-48 months ⊕⊕⊕⊝ MODERATE2 due to imprecision OR 0.28 (0.1 to 0.84) Anticipated absolute effects Risk with Usual community care Risk difference with Pulmonary rehabilitation (95% CI) 405 per 1000 275 fewer per 1000 (from 122 fewer to 353 fewer) Low1 100 per 1000 70 fewer per 1000 (from 15 fewer to 89 fewer) High1 Systematic Reviews & GRADE 500 per 1000 281 fewer per 1000 (from 43 fewer to 409 fewer) Quality of life (CRQ) dyspnea Chronic Respiratory Questionnaire3. Scale from: 1 to 7. 258 (5 studies) 12 and 76 weeks ⊕⊕⊕⊝ MODERATE4 due to imprecision The mean quality of life (sgrq) total in the control groups was 3.1 The mean quality of life (crq) dyspnea in the intervention groups was 0.97 higher (0.35 to 1.58 higher) Quality of life (SGRQ) total St George's Respiratory Questionnaire5. Scale from: 0 to 100. 127 (3 studies) 12 and 26 weeks ⊕⊕⊕⊝ MODERATE4 due to imprecision The mean quality of life (sgrq) total in the control groups was 50 The mean quality of life (sgrq) total in the intervention groups was 9.88 lower (5.37 to 14.4 lower) Ambulation (as measured by 6 min walking distance) distance in meters 6 299 (6 studies) 1 - 208 weeks7 ⊕⊕⊕⊝ MODERATE4,8 due to imprecision Resource use not reported - - The mean ambulation (as measured by 6 min walking distance) in the intervention groups was 77.7 higher (12.21 to 143.2 higher) - See footnote Evidence & judgments See footnote Recommendations, health policy & implementation Question/Recommendation: Should contacts of new or recurrent TB cases be investigated? Population: In people (at normal risk) who had contact with new or recurrent cases of TB (does) Intervention: contact investigation Setting (if relevant): high income countries Decision domain: Quality of evidence (QoE) Is there high or moderate quality evidence? The higher the quality of evidence, the more likely is a strong recommendation Comparison: no investigation Judgment Yes No Summary of reason for judgment Explanation There is very low quality evidence from observational studies that are moderate risk of bias for the critical outcomes. Balance of benefits versus harms and burdens Are you confident that the benefits outweigh the harms and burden or vice versa? The larger the difference between the benefits and harms and the certainty around that difference, the more likely is a strong recommendation. The smaller the net benefit or net harm and the lower the certainty for that net effect, the more likely is a conditional/weak recommendation. Yes No There is considerable benefit while little clinical harm or downsides are expected The yield for all tuberculosis (bacteriologically-confirmed and clinically diagnosed) was 4.5% of contacts investigated. Latent tuberculosis infection was found in 51.4% of contacts investigated. The yield for all tuberculosis (bacteriologically-confirmed and clinically diagnosed) was 7.0 % of pediatric contacts investigated. Latent tuberculosis infection was found in 40.4% % of pediatric contacts investigated. Subdomains influencing judgment QoE for benefits: Very low QoE for harms: Harms not explicitly evaluated QoE for resource use: Resource use not explicitly evaluated Key reasons for down- or upgrading? Risk of bias was a reason for downgrading for most critical outcomes All critical outcomes measured? Harms and resources not explicitly evaluated Baseline risk for benefits and harm and burden? Is the baseline risk similar across subgroups? Should there be separate recommendations for subgroups? Relative risk for benefits and harms: Are the relative benefits large? Yes, the relative benefits are probably large. Are the relative harms large? No, the relative harms are probably small. Recommendations for other groups are made separately, pediatric and adult index cases were considered together. Requirement for modeling: Is there a lot of extrapolation and modeling required for these outcomes? Yes, modeling is required. Values and preferences Are you confident about the assumed or identified relative values and are they similar across the target population? Yes No Benefits much higher valued than expected minor harms. The more certainty or similarity in values and preferences, the more likely a strong recommendation. Resource implications Are the resources worth the expected net benefit from following the recommendation? The lower the cost of an intervention compared to the alternative, and other costs related to the decision – that is, the fewer resources consumed – the more likely is a strong recommendation in favour of that intervention. Overall strength of recommendation Remarks Yes A high value was placed on avoiding consequences of TB, dissemination of TB and mortality. A low value was placed on possible adverse events. There is likely little variability and panel is quite certain No Resources required are worth the net benefit considering the benefit on mortality and new TB cases. ?Strong/con ditional? There are resources required to conduct contact investigation but these resources are worth the expected benefits and downstream treatment costs. Perspective taken: Patients or public Source of values: Guideline panels assessment Source of variability if any: Not a lot of variability Method for determining values satisfactory for this recommendation: Yes, given the expected small variability and difference between guideline panel and patients. Depending on contact investigation strategy used, resource utilization and are implications vary.unit? What the cost perwill resource Opportunity cost may be high. Feasibility: Opportunity Feasibilitycost: is dependent on existing Differences across settings: and well functioning programs. Resources worth in smear positive index cases The guideline panel recommends that contacts of patients with TB who are at normal risk be investigated. (NOTE: this is a hypothetical recommendation developed for this article and not intended for clinical decision making.) This recommendation places a high value on the benefits that can be expected (mortality reduction, reduction in TB dissemination) and a relatively low value on the required resources and side effects of treatment. Should cryotherapy versus LEEP be used in women with histologically confirmed cervical intraepithelial neoplasia? Quality assessment No. of studies Design Limitations Inconsistency No of patients Indirectness Imprecision Other Effect Cryotherapy LEEP Relative (95% CI) Absolute effect at 1 year (95% CI) Quality Importance 12/161 (7.5%) 4/168 (2.4%) OR 3.3 (1.04 to 10.46) 51 more per 1000 (from 1 to 179 more) O CRITICAL OO CRITICAL Recurrence CIN2–3 (follow-up 12 months randomized trials; 3–85 months observational studies) 1 randomized trials no serious limitations no serious inconsistency no serious indirectness seriousa,b none 3 observational studies no serious limitations no serious inconsistency no serious indirectness no serious imprecision none 2227/14 387 (15.5%) 319/7454 (4.3%) — OR 2.66 (1.89 to 3.75) 2.4%c 37 more per 1000 (from 20 to 60 more) Cervical cancer (follow-up 12 months randomized trials; 3–85 months to 26 years observational studies) 1 randomized trials no serious limitations no serious inconsistency no serious indirectness very seriousa none 0/200 (0%) 0/200 (0%) — 0 fewer per 1000d OO CRITICAL 2 observational studies no serious limitations no serious inconsistency no serious indirectness no serious imprecision none 2/679 (0.3%) 3/3350 (0.1%) — 0 fewer per 1000e OO CRITICAL none 15/170 (8.8%) 8/186 (4.3%) OR 2.15 (0.89 to 5.22) 45 more per 1000 (from 5 fewer to 147 more) OO CRITICAL 3/300 (1%) 2/298f (0.67%) — 0.4 more per 1000 (from 8 fewer to 9 more) OO CRITICAL 136 480 OO CRITICAL OOO CRITICAL Treatment unacceptable to women (follow-up 2 weeks; acceptability question) 1 randomized trials no serious limitations no serious inconsistency no serious indirectness very seriousf All severe adverse events (follow-up mean 12–16 months; stenosis and PID) 2 randomized trials no serious limitations no serious inconsistency no serious indirectness very seriousf none All severe adverse events (follow-up 33 months; PID, plug syndrome, stenosis, blood transfusion) 5 randomized trials no serious limitations no serious inconsistency serioush serioush none 4%i — OR 0.53 (0.1 to 2.88) 18 fewer per 1000 (from 36 fewer to 67 more) All severe adverse events (follow-up 12 months; PID, stenosis, major bleeding) 9 observational studies serious limitationsj no serious inconsistency seriousi seriousf none 1/2233 (0%) 38/960 (4%)a — 10 fewer per 1000 (from 20 fewer to 0) Recommendation • In settings where LEEP is available and accessible, and women present with CIN lesions extending into the cervical canal, the expert panel suggests treatment with LEEP over cryotherapy (conditional recommendation, OO quality evidence) • Remarks: The benefits of LEEP were greater than those of cryotherapy, and the harms were fewer in these women. However, since there are greater resource implications for LEEP than cryotherapy, and thus LEEP is not available in all settings, a conditional recommendation was made. Implications of a conditional/weak recommendation • Patients: The majority of people in this situation would want the recommended course of action, but many would not • Clinicians: Be more prepared to help patients to make a decision that is consistent with their own values/decision aids and shared decision making • Policy makers: There is a need for substantial debate and involvement of stakeholders Implications of a strong recommendation • Patients: Most people in this situation would want the recommended course of action and only a small proportion would not • Clinicians: Most patients should receive the recommended course of action • Policy makers: The recommendation can be adapted as a policy in most situations , can be used as quality indicator/performance measure Only two of six performance measures seemed reasonable WHO evaluation & feedback • WHO staff & guideline review committee members (GRC) invited to feedback (Jan 2011) about using GRADE approach – what worked – what did not work • Group discussion (NGT), 11 + 2 Summary of feedback • Transparency of the GRADE process helps • Requirement for a good Chair – methods knowhow to move the process • For observational studies we need better/ ¿different? summaries (e.g. narrative versions) • Integration and elicitation of values and preferences was frequently challenging • For global guidelines: issues around the description of baseline risks and applicability across countries require work Summary of feedback • Variability in baseline risk → weak or conditional recommendations should follow • A description of the modifying factors and the layout of the evidence could be a great benefit and will facilitate implementation • Measures should be taken to streamline the timing of the development of guidelines • Working with centers, training, and capacity building of these centers who collaborate with WHO a priority for implementing GRADE • Impact evaluation (of current process for development of guidelines) should take place Conclusions • (WHO) guidelines should be based on the best available evidence to be evidence based • GRADE not avoid judgments but provides framework • combines what is known in health research methodology and provides an approach to improve communication • GRADE process works – is it better? • Change in culture towards the use of evidence • Transparency in decision making and judgments is key Thanks • Nancy Santesso, Andy Oxman, Suzanne Hill • WHO staff who participated in providing feedback Results - PRISMA Records identified through database searching (all study designs) EMBASE, MEDLINE = 9873 SIGLE = 7 CINAHL = 1062 LILACS = 19 COCHRANE = 301 Chinese Biomedical Literature Database = 914 Panteleimon = 12 (Total n = 12176) Records after duplicates removed (n = 7456) Records screened (n = 7483) Studies awaiting assessment (n = 6) •Studies awaiting translation (1) •Papers could not obtain in full (5) Full-text articles assessed for eligibility (n = 920 ) Studies included N = 89 Question •51 + 5 studies •7 studies •6 studies •0 studies •8 •0 studies •16 •0 studies •1 study •2 studies Note: one study may be relevant to multiple questions Additional records identified through other sources Pharmaceutical companies (n = 12) Reference lists of relevant papers (n=15) Records excluded (n = 6563) Full-text articles excluded (n = 825) Excluded for •Not influenza or influenza like illness •Fewer than 25 people •Randomised controlled trial, or not an observational study •Not antiviral agent •Antiviral agents analysed together •Prophylaxis •No outcomes reported Results Should oseltamivir versus no treatment be used to treat influenza? Mortality (adjusted) oseltamivir no treatment Study or Subgroup log[Odds Ratio] Odds Ratio Total Hanshaoworakul 2009 -2.040221 0.58739416 315 130 28.5% 0.13 [0.04, 0.41] Liem 2009 (1) -0.941609 0.75113239 55 12 17.5% 0.39 [0.09, 1.70] McGeer 2009 (2) -1.309333 69 100 54.0% 0.27 [0.12, 0.62] 242 100.0% 0.23 [0.13, 0.43] 0.4270348 Total (95% CI) Total Weight Odds Ratio SE 439 IV, Random, 95% CI Heterogeneity: Tau² = 0.00; Chi² = 1.58, df = 2 (P = 0.45); I² = 0% IV, Random, 95% CI 0.1 0.2 0.5 1 2 5 10 Favours oseltamivir Favours no treatment Test for overall effect: Z = 4.63 (P < 0.00001) (1) Adjusted for neutropenia and hospital admission (2) Does not specify what was adjusted for Mortality (unadjusted) Oseltamivir Study or Subgroup Chemaly 2007 Events No treatment Total Events Odds Ratio Total Weight M-H, Random, 95% CI 0 25 3 8 5.2% 0.03 [0.00, 0.69] 150 328 5 8 13.4% 0.51 [0.12, 2.15] Hien 2009 5 25 2 4 8.6% 0.25 [0.03, 2.24] Huang 2009 2 17 1 57 7.3% 7.47 [0.63, 88.02] 0 118 0 27 18 55 8 12 14.4% 0.24 [0.06, 0.92] Estenssoro 2010 Li 2010 Liem 2009 McGeer 2009 Not estimable 8 68 34 100 18.9% 0.26 [0.11, 0.60] Siston 2010 (1) 21 476 5 74 17.3% 0.64 [0.23, 1.74] Xi 2009 24 125 3 30 14.9% 2.14 [0.60, 7.64] 320 100.0% 0.51 [0.23, 1.14] Total (95% CI) Total events 1237 228 61 Heterogeneity: Tau² = 0.70; Chi² = 16.76, df = 7 (P = 0.02); I² = 58% Test for overall effect: Z = 1.64 (P = 0.10) (1) Pregnant women Odds Ratio M-H, Random, 95% CI 0.001 0.1 1 10 1000 Favours oseltamivir Favours no treatment Recommendation - The Guidelines Group recommends that TB programs/clinicians use/do not use fluoroquinolones in the treatment of all patients with MDR (Strong (conditional) recommendation/ low (very low, low, moderate, high) grade of evidence) Example: Oseltamivir for Avian Flu Recommendation: In patients with confirmed or strongly suspected infection with avian influenza A (H5N1) virus, clinicians should administer oseltamivir treatment as soon as possible (strong recommendation, very low quality evidence). Remarks: This recommendation places a high value on the prevention of death in an illness with a high case fatality. It places relatively low values on adverse reactions, the development of resistance and costs of treatment. Schunemann et al. The Lancet ID, 2007 Other explanations Remarks: Despite the lack of controlled treatment data for H5N1, this is a strong recommendation, in part, because there is a lack of known effective alternative pharmacological interventions at this time. The panel voted on whether this recommendation should be strong or weak and there was one abstention and one dissenting vote. Recommendation: In settings where LEEP/LLETZ is available and accessible, the expert panel suggests treatment with LEEP/LLETZ over cryotherapy Population: Women with histologically confirmed CIN Intervention: Cryotherapy versus LEEP Decision Factor Explanation High or moderate evidence There is moderate-quality evidence from both randomized and (is there high- or moderate-quality observational controlled studies for recurrence rates. However, there evidence?) is low-quality evidence for other outcomes that were considered critical and important for decision-making (e.g. severe adverse Yes OO The higher the quality of evidence, the events, cervical cancer). There is uncertainty for fertility and other No more likely is a strong obstetric outcomes, and HIV acquisition/transmission was not recommendation. measured. Certainty about the balance of benefits versus harms and burdens (is there certainty?) The larger the difference between the desirable and undesirable consequences and the certainty around that difference, the more likely is a strong recommendation. The smaller the net benefit and the lower the certainty for that benefit, the more likely is a conditional/ weak recommendation. Yes No Recurrence rates of CIN1, CIN2–3 and all CINs are probably greater with cryotherapy: o CIN2–3, odds ratio (OR) 3.3 (CI 1.04 to 10.46) o CIN1, OR 2.74 (CI 0.62 to 12.07) o All CIN, OR 2.14 (CI 1.05 to 4.33). Cryotherapy may be less acceptable to patients than LEEP. There may be little difference in serious adverse events between cryotherapy and LEEP, but there may be fewer minor adverse events (such as pain) with cryotherapy. It is unclear whether there is a difference in fertility/obstetric outcomes. High value was placed on CIN recurrence, serious adverse events and acceptability to the patient. Low value was placed on minor adverse events. There is not a lot of variability The panel felt secure in assuming the populations value Need for more skilled providers to perform LEEP Need for more or expensive equipment/supplies for LEEP; electricity supply for LEEP Need for local anaesthesia with LEEP Benefits of LEEP were greater, and harms were fewer or similar Certainty in or similar values (is there certainty or similarity?) The more certainty or similarity in values and preferences, the more likely is a strong recommendation. Yes No Similar values across women Yes No More resources required for LEEP Resource implications (are resources worth expected benefits?) The lower the cost of an intervention compared to the alternative that is considered and other costs related to the decision – that is, fewer resources consumed – the more likely is a strong recommendation. Overall strength of recommendation Conditional Methods Types of participants • We included studies in all populations with influenza or influenza like-illness. Types of intervention • Oseltamivir, zanamivir, amantadine or rimantadine in any dose or by any route. Type of outcome measures • We determined a priori to report on the following outcomes because they were judged to be important or critical for decision making: • Mortality, Hospitalisation, ICU Admission, mechanical ventilation and respiratory failure, Duration of hospitalization, Time to alleviation of symptoms, Time to return to normal activity, Complications • Critical adverse events (e.g. major psychotic disorders, encephalitis, stroke and seizure), • Important adverse events (e.g. pain in extremities, clonic twitching, body weakness, dermatological changes such as uticaria and rash) • Viral shedding and Resistance GRADE Uptake World Health Organization Allergic Rhinitis in Asthma Guidelines (ARIA) American Thoracic Society American College of Physicians European Respiratory Society European Society of Thoracic Surgeons British Medical Journal Infectious Disease Society of America American College of Chest Physicians UpToDate® National Institutes of Health and Clinical Excellence (NICE) Scottish Intercollegiate Guideline Network (SIGN) Cochrane Collaboration Infectious Disease Society of America Clinical Evidence Agency for Health Care Research and Quality (AHRQ) Partner of GIN Over 60 major organizations GRADE Uptake World Health Organization Allergic Rhinitis in Asthma Guidelines (ARIA) American Thoracic Society American College of Physicians European Respiratory Society European Society of Thoracic Surgeons British Medical Journal Infectious Disease Society of America American College of Chest Physicians UpToDate® National Institutes of Health and Clinical Excellence (NICE) Scottish Intercollegiate Guideline Network (SIGN) Cochrane Collaboration Infectious Disease Society of America Clinical Evidence Agency for Health Care Research and Quality (AHRQ) Partner of GIN Over 60 major organizations Recommendation 1a • The panel recommends that people who had household contact with smear positive or M/XDR TB index cases be investigated for active TB (strong recommendation, very low quality evidence). Recommendation 1b • The panel recommends that people who had household contact with TB index cases who are children younger than 5 years of age be investigated for active TB (strong recommendation, very low quality evidence).