Template for week 16 - Just my annual check up - PBL-J-2015
advertisement

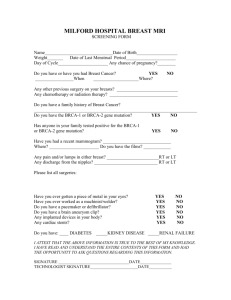
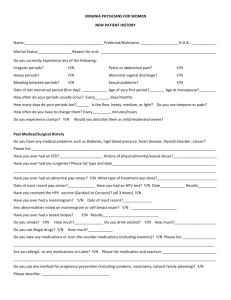
Outline of Key Learning Areas related to PBL week 16 ‘Just my annual check-up’ Relevant Symptoms (incl. relevant negatives) None on initial presentation – simply came in for a check-up: pap smear performed and referral provided for mammogram Other Significant History 49 year-old nulliparous woman LMP 6/12 ago - perimenopausal Mother and aunt both died of breast cancer in their fifties (first-degree relatives) Examination and Signs Pap smear normal Mammogram showed ‘suspicious area’; fine needle aspirate showed malignant cells (appear irregular compared to benign neoplasia) Lymphovascular invasion No lymph node involvement Hormone receptor assay showed HER+ (positive receptor for oestrogen) and negative receptor for progesterone Provisional Diagnosis Differential Diagnoses Initial: Grade III Ductal carcinoma Fibroadenoma/ Breast cyst Fibrocystic change of the breast is a non-specific term, commonly understood as a Follow-up: Presented with back pain, lethargy, malaise, continuum of physiological changes that expand to the pathological spectrum. It is nausea and weight loss. These symptoms were a condition characterised by "lumpy" breasts, associated with pain and tenderness associated with pulmonary, bone and liver metastases, that fluctuate with the menstrual cycle. leading to severely impaired renal function Mammographic calcifications that are large, are round, have sharp edges, and are diffuse are typically benign Risk Factors Genetic: BRCA1/BRCA2(tumour suppression and DNA repair) associated with 3% of breast cancers p53 (CDK inhibitor) CHEK2 1st degree family history of breast cancer Hormonal – exposure to oestrogen Female (99% of breast cancers occur in women) Age of menarche/menopause Nulliparity /Never lactating HRT Age peak = 75-80 years old Other Radiation/carcinogen exposure Aetiology Oestrogen levels, which are higher in women than in men, stimulate proliferation of breast epithelial cells in the lobules and ducts. Spontaneous mutations in epithelial cells, some of which provide a survival advantage to the cell, lead to precancerous changes. Further mutations lead to in situ or invasive breast cancer. ) 1) Anatomy 3) Microbiology nil 4) Pathophysiology Carcinogenesis is a multi-step process (due to multiple mutations – either inherited or acquired) which results in: self-sufficient growth without external stimuli (protooncogenes mutate to oncogenes) insensitivity to growth inhibitory signals evasion of apoptosis defects in DNA repair Ductal carcinoma in situ (DCIS) is a potential precursor of invasive carcinoma and suggests that cancer will become invasive at that site. Metastasis Signifies the tumour is malignant Routes of metastasis include lymphatics Lymphatic drainage Blood vessels Direct extension CNS spread Transcoelomic Field effect – exposure can cause multiple primary tumours Method of metastatic spread: Breach of ECM - breach of basement membrane and migration of tumour cells Dissemination - Formation of tumour cell embolus and adhesion to endothelium of a DISTANT site Formation of secondary deposit – digestion of basement membrane and CT, proliferation of cells in new location Angiogenesis – support blood vessels to supply the new growth. Histopathology Most breast cancers (95%) are adenocarcinomas Divided into: in situ carcinomas (neoplastic proliferation confined to the ducts/lobules by the basement membrane – usually impalpable) invasive carcinomas Neoplasm that has penetrated the basement membrane and can present with macroscopic changes Tumour grading Surface anatomy 2) Physiology/Biochemistry The influence of oestrogen on breast tissue Foetus/neonate Mammary glands consist almost entirely of lactiferous ducts with few alveoli Histologic Grade Grade 2. Grade 1. Well moderately Differentiated differentiated , or low grade , or intermediate Grade 3. Poorly differentiated , or high grade Puberty: Under the influence of oestrogen, lactiferous ducts sprout and branch to develop alveolar precursors Breasts enlarge mostly due to fat deposition Nipples become prominent Resting adult: Glandular part consists mostly of ducts – small lobules When oestrogen levels peak in the menstrual cycle, duct cell proliferation Increases Pregnancy: Large increase in breast size, mainly due to alveolar proliferation, differentiation and duct branching Amount of CT and fat stays the same but decreases relative to glandular tissue Lactation Alveolar cells become smaller and low cuboidal - cytoplasm contains fat droplets and may appear vacuolated Secretion distends the alveoli and milk collects in the lactiferous ducts Post-Menopause The glandular component of the breast involutes and is replaced by fat and CT grade Total score of each parameter A+B+C 3-5 6-7 8-9 Scoring Summary Relative Score or each parameter 1 2 3 A. Tubules Assessmen t in % >75%= 1 10-75%=2 <10%=3 B. Nuclear Grade Assessmen t Uniform Nuclei with minimal nuclear variation in size and shape= 1 moderate nuclear variation in size and shape = 2 Marked nuclear variation and bizarre nuclei ( sometimes with prominent nuceloli ) = 3 C. Mitotic Index Assessmen t 5-10 mitoses =1 11-19 = 2 >20 = 3. Cancer staging (TNM) T = (Primary) Tumour Size � T0 = impalpable � T1 = 0-2cm � T2 = 2-5cm � T3 = ≥ 5cm ± fixation to underlying muscle � T4 = any size, with fixation to chest wall or skin o N = Lymph Node Status � N1 = regional nodes involved � N2,N3 = more distant nodal Groups o M = Metastases � M0 = no detectable spread � M1 = metastases present (specify sites) Investigations and Results 1) Blood tests nil 2) Imaging Mammogram (right) A mammographic finding of clustered calcifications, either focal or diffuse, and absence of a soft tissue abnormality suggests ductal carcinoma in situ (DCIS). 3) Other Hormone receptor assay Oestrogen and progesterone receptor status is measured by immunohistochemical staining of fixed tumour tissue. Results can help to guide treatment. ER + means the tumour relies on oestrogen for growth Diagnosis confirmed by triple test: 1)clinical – inspection and palpation 2) radiological – mammogram 3) Pathological – aspirate and histological assessment Imaging con’d Bone scan Fine needle aspiration and biopsy (below) Benign Malignant Showed multiple ‘hot spots’ Management Plan Problem Goal/desired outcome Ductal carcinoma Removal Hormone-related growth of neoplastic cells Interruption of oestrogen growth stimulus to prevent further growth of Method (incl. patient actions) Excision of lump (lumpectomy) and axillary dissection Oestrogen antagonist administered Resources/health professional s involved Oncologist tumour Locally invasive tumour Radiotherapy Potentially metastatic or recurring tumour Pain related to metastatic cancer Prevention of metastatic spread/return of cancer Analgesia Poor prognosis Palliative care Medications Mode of action Tamoxifen Tumour cells that express the oestrogen receptor ERα are sensitive to hormone-based therapy, leading to a good therapeutic outcome Chemotherapy Morphine administered for pain associated with metastases Holistic approach Family involvement Symptom relief Pain management Multi-disciplinary approach Side effects Menopause-like symptoms It is an oestrogen agonist/antagonist (with the predominant effect depending on the tissue). It is effective in preventing disease recurrence in oestrogen receptor-positive ductal carcinoma in situ (DCIS) and invasive breast cancers, as well as in decreasing the risk of oestrogen receptor-positive cancers developing in the contralateral breast. Chemotherapy Duration of treatment is 5 years drug therapy, usually given through I.V line, which targets dividing cells Oncologist, radiotherapist Systemic symptoms Palliative care team Palliative care nurse Any specific monitoring required? Consideration of preservation of oocytes, fertility treatment causing them to stop dividing and selfdestruct regimes usually last 4-6 months, require hospital stays and have various side-effects Radiotherapy reduces the chance of breast cancer returning by about 1/3 Uses high-powered radiation beams which deliver radioactive particles or X-rays to targeted tissue causing the death of cells Whole-breast radiotherapy is an essential component of local therapy following breast-conserving surgery and has been shown to reduce 5-year local recurrence. skin changes like sunburn, pigmentation of skin, woodiness of breast tissue, fatigue, depression, it rarely can damage other organs Other Psychosocial/ethical/legal/patient-centred considerations Depression related to poor prognosis Informed decision-making about end-of-life care PPH/PPD implications Screening Mammogram Early detection is highly effective in reducing mortality associated with breast cancer, with impalpable cancers being detected 1-2 years earlier than relying on examination alone. Nonetheless, screening leads to over-diagnosis and over-treatment of breast disease in many women, and women invited to screening should be informed of both the benefits and harms. In Australia, women are encouraged to have mammogram screening every two years from age 50-70. If more than 2 risk factors are present, women can access mammogram screening earlier or even elect to have a prophylactic mastectomy Self-examination All adult women can perform a monthly breast self-examination to detect lumps. However, ductal carcinoma in situ is generally detected by mammography before it is palpable, so this physical examination of the breast is more likely to detect invasive cancer. Breast examination is rarely of benefit to detect lobular carcinoma in situ. Epidemiology Breast cancer is the most common cancer in females, affecting 1 in 11-15 women in Australia Resources used/discovered