holloway 01-10-14
advertisement

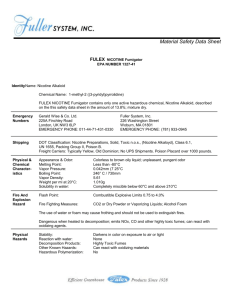
Maternal smoking and risk of metabolic syndrome in the offspring: Evidence from animal studies Dr. Alison Holloway Department of Obstetrics and Gynecology Reproductive Biology Division McMaster University October 1st 2014 What is metabolic syndrome? Metabolic syndrome is the name for a group of risk factors that raises your risk for heart disease and other health problems, such as diabetes and stroke. These include: Central obesity Elevated serum triglycerides (≥ 150 mg/dL (1.7 mmol/L)) Reduced HDL cholesterol (< 40 mg/dL (1.03 mmol/L*) males and < 50 mg/dL (1.29 mmol/L*) Raised blood pressure (systolic BP ≥ 130 or diastolic BP ≥ 85 mm Hg) Raised fasting plasma glucose (≥ 100 mg/dL (5.6 mmol/L), or type 2 diabetes Why worry? • The prevalence of metabolic syndrome continues to grow unabated • Worldwide it is estimated that there are 1 billion overweight and 300 million obese adults (World Health Organization) •Overweight and obesity are associated with increased mortality and morbidity (including an increased risk of chronic diseases such as diabetes, hypertension, asthma, heart disease, and cancer) Estimated prevalence of obesity among all Canadians by province, 2000-2012 15-19% 20-24% 25-29% 30-34% ≥35% 2000 2003 2005 2007 2008 2009 2010 2011 2012 Sources: Gotay C, Katzmarzyk P, Janssen I, Dawson M, Aminoltejari K, Bartley N (2013). Updating the Canadian obesity maps: An epidemic in progress. Canadian Journal of Public Health 104(1). Retrieved from http://journal.cpha.ca/index.php/cjph/article/view/3513. Adults with BMI >30kg/m2 in each province calculated from the self-reported height and weight surveys conducted by the CCHS and corrected to account for misreporting of height and weight. Statistics Canada. Table 105-0501 - Health indicator profile, annual estimates, by age group and sex, Canada, provinces, territories, health regions (2012 boundaries) and peer groups, occasional, CANSIM (database). Accessed: 2013-10-20 . Permalink: http://www5.statcan.gc.ca/cansim/a05?lang=eng&id=1050501 Source: WHO Diabetes Programme (http://www.who.int/diabetes/facts/en/) Does Metabolic Syndrome Begin in the Womb? The Barker Hypothesis- original version Maternal Undernutrition Fetal Growth Retardation Coronary Heart Disease In Later Life Death from coronary heart disease before age 65 according to birthweight (Hertfordshire population) 1.6 P for trend=0.001 1.4 Hazard ratio 1.2 1.0 0.8 0.6 0.4 0.2 0.0 ≤5.5 5.5-6.5 6.5-7.5 7.5-8.5 Birthweight Barker et al.,1989 Lancet 2:577 8.5-9.5 ≥9.5 The Barker Hypothesis Also known as: 1) Fetal origins of adult disease hypothesis 2) Fetal programming hypothesis 3) Developmental origins of health and disease hypothesis Adverse environments in fetal life and early childhood establishes an increased risk of disease in adult life Causes of low birthweight in humans and animal models Prenatal glucocorticoid exposure Uteroplacental insufficiency/hypoxia Maternal / Fetal undernutrition Intrauterine Growth Restriction Hypertension Obesity Type 2 Diabetes Causes of low birthweight in humans and animal models Prenatal glucocorticoid exposure Uteroplacental insufficiency/hypoxia Maternal / Fetal undernutrition Maternal smoking Intrauterine Growth Restriction Hypertension Obesity Type 2 Diabetes Maternal cigarette smoking • Associated with preterm labour, low birthweight babies and other adverse obstetrical outcomes • Approximately 15-20% of all pregnant women smoke during their pregnancies 22.7% of pregnant women at McMaster reported smoking during pregnancy (Foster et al., 2005. Am J Obstet Gynecol 193:1900-1907) Q: What component of cigarette smoke is important for increased risk of postnatal disease? A: Nicotine? Why is nicotine important? • Nicotine addiction is primary reason women do not quit smoking during pregnancy • Nicotine replacement therapy (NRT) has been suggested as an acceptable therapy for pregnant women who can’t quit smoking by other means (OMA, 1999) •Nicotine administration alone during pregnancy in rats causes a reduction in birthweight (Newman et al., 1999 Behav Pharmacol 10:699-706) Locomotor behavioral effects of prenatal and postnatal nicotine exposure in rat offspring. Abstract The purpose of this study was to determine if prenatal/postnatal nicotine exposure results in hyperactive offspring. Rat offspring were exposed to nicotine, through implantation of osmotic minipumps in dams, at levels of 0.75, 1.5 and 3.0 mg/kg/day, for 19 days prenatally and 16 days postnatally. Offspring were measured for gestation length, body weight, litter size, sex difference and locomotor activity. No significant effects were shown for gestation length, litter size or male to female pup ratio. However, higher percentage of pup deaths resulted from nicotine-exposed dams than from control dams. Significantly less litter body weight was shown in nicotine-exposed offspring on postnatal day 1 when compared to controls. However, these offspring surpassed the control groups in litter body weight on postnatal day 14 and 21. Hyperactivity was shown in offspring exposed to prenatal/postnatal nicotine at levels of 0.75 and 3.0 mg/kg/day on postnatal day 14, but not on postnatal day 21 or at the 1.5 mg/kg/day condition. Results are consistent with the hypothesis that rat offspring are susceptible to the neurochemical and neurobehavioral effects of prenatal/postnatal nicotine exposure. Behav Pharmacol 1999 Nov;10(6-7):699-706 Effect of nicotine on fetal growth 7 Saline Nicotine * 6 * 5 Weight (g) 4 3 2 1 0 d15 Gruslin et al., 2009 Reprod Sci 16: 875-882 d18 d21 PND1 Hypothesis Nicotine exposure in utero will cause metabolic syndrome in the offspring Specific aims To assess the effect of in utero exposure to nicotine on: • Postnatal growth and adiposity • Markers of cardiovascular disease • Glucose homeostasis Introduction: Animal Model 2 weeks 3 weeks 3 weeks Mating Pregnancy Lactation Nicotine (1.0 mg/kg/d) Saline (Vehicle) Birth (Postnatal Day 1) Weaning (Postnatal Day 21) 23 weeks Outcome measures to determine changes related to: Obesity Hypertension T2DM Endpoint 26 weeks Birthweight 7.5 Birthweight (g) 7.0 * 6.5 6.0 5.5 5.0 4.5 4.0 saline nicotine Fetal exposure to nicotine reduced average birthweight approximately 20%. There was no effect on litter size OBESITY Fetal and neonatal exposure to nicotine increases body weight * 700 Body weight (g) 600 nicotine saline 500 * * 400 300 200 100 0 0 5 10 15 20 Age (weeks) 25 30 Fetal and neonatal exposure to nicotine increases fat pad weight 3 weeks of age WAT (% of bodyweight) +67% 26 weeks of age 6 5 +35% 4 3 2 1 0 (Somm et al., 2008 Endocrinology 149:6289-6299) * saline nicotine *P<0.05 Perivascular fat tissue (PVFT) at 26 weeks of age J Endocrinol. 2008 Apr;197(1):55-64 PVFT area (mm2) Saline Nicotine Mesenteric artery 7.7 ± 0.73 11.2 ± 1.27* Thoracic artery 2.6 ± 0.24 3.9 ± 0.25* *P<0.05 Nicotine-exposed animals have dyslipidemia Age 7 weeks Serum triglyceride concentration mg/dL Body weight (g) SALINE NICOTINE SALINE NICOTINE 71.6 ± 10.56 95.6 ± 6.29 264.2 ± 7.94 264.7 ± 1.43 p=0.052 15 weeks 115.9 ± 3.44 126.8 ± 2.89* 487.5 ± 11.65 545.0 ± 6.24* 26 weeks 149.5 ± 5.56 177.2 ± 16.48* 576.5 ± 14.44 653.9 ± 10.43* *P<0.05 What causes the increased weight gain in nicotine-exposed animals? Mechanisms of Programming? Nicotine (or other insults) PHYSIOLOGICAL SYSTEMS •Reorganisation of organ structure •Altered organ function •Altered cell number •Altered intracellular organization DNA •altered cell specific gene regulation •altered DNA binding proteins •changes in mitochondrial DNA EPIGENETIC CHANGES •altered DNA methylation Increased adipocyte differentiation (Somm et al., 2008 Endocrinology 149:6289-6299) *P<0.05 Food intake (g/rat/day) Increased food consumption and decreased activity * 32 28 24 20 16 saline nicotine *P<0.05 HYPERTENSION Blood pressure Mean arterial pressure (mm Hg) 170 160 Systolic BP 150 140 Diastolic BP 130 BP increased by 14-17 weeks of age 120 Same changes seen in WKY & SHR rats 110 100 saline nicotine Blood pressure at 26 weeks of age in saline- and nicotine-exposed male offspring (n=15 per group). What causes the increased blood pressure in nicotine-exposed animals? • Altered renal development? Elevated blood pressure does not appear to be related to changes in renal structure or function Saline Nicotine Kidney weight (g) 2.84 ± 0.05 2.93 ± 0.07 Kidney weight (% body weight) 0.69 ± 0.01 0.66 ± 0.01 Nephron density (per mm3) 108.2 ± 1.80 93.2 ± 5.04 Nephron number (x1000 per kidney) 65.4 ± 1.95 68.83 ± 3.99 Glomerulus area (µm2) 7298 ± 609 8115 ± 858 Urinary albumin (ng /mg creatinine) 0.38 ± 0.066 0.38 ± 0.063 Gao YJ et al., unpublished data What causes the increased blood pressure in nicotine-exposed animals? • Altered renal development? • Altered vascular reactivity? Vascular reactivity Contraction (% of KCl) 200 * Nicotine * 150 Saline 100 50 0 8 7 6 5 Phenylephrine (- log M) 4 What causes the increased blood pressure in nicotine-exposed animals? • Altered renal development? • Altered vascular reactivity? Conclusion Fetal and neonatal exposure to nicotine results in postnatal hypertension TYPE 2 DIABETES Fasting glucose * 3200 3000 2800 AUC Fasting serum glucose (mmol/l) 9.0 2600 2400 2200 nicotine 2000 SV NV 7.5 saline 6.0 4.5 0 5 10 15 20 25 30 Age (weeks) Basal fasting glucose at 4, 7, 15 and 26 weeks of age (n=15 per group). Measurements were made on the same animals at each age. The inset panel represents the total area under the curve (* p<0.05) Oral Glucose Tolerance Test •Animals fasted overnight •Fasting blood sample taken at t=0 •Glucose challenge (2g/kg) by gavage •Serial blood samples collected at 30’ and 120’ to assess peak glucose and ability to clear the glucose load respectively •Total glucose response to the challenge (area under the curve) calculated Nicotine-exposed offspring are dysglycaemic by 26 weeks of age 2 Weeks 3 Weeks 3 Weeks Mating Pregnancy Lactation 23 Weeks Nicotine (1.0 mg/kg/d) Saline (Vehicle) Birth Endpoint (26 weeks) Weaning (3 weeks) * 14 1400 * * 12 1300 nicotine AUC Serum glucose (mmol/l) 1500 10 saline 8 0 20 1100 1000 900 2g/kg glucose 6 1200 40 60 80 100 Time (minutes) 120 140 800 saline nicotine Conclusion Fetal and neonatal exposure to nicotine results in aberrant glucose control in adulthood What causes nicotine-induced dysglycemia? • Reduced beta cell mass? Beta cell mass 12 10 * saline Beta cell mass (mg) 8 6 2 nicotine * 4 * 0 0 5 10 15 20 25 30 Age (weeks) Beta cell mass from birth to 26 weeks of age measured by immunohistochemical staining for insulin and morphometric analysis at 26 weeks of age (n=5 per group). Data are presented as mean ± SEM (*p<0.05). What causes nicotine-induced dysglycemia? • Reduced beta cell mass? • Reduced insulin effect at target tissues? Insulin resistance Insulin response to OGTT * AUC insulin 300 250 200 150 100 50 0 saline nicotine Increased insulin response was not sufficient to normalize glucose response to OGTT . Insulin resistance Insulin response to OGTT 400 * 300 250 300 200 ROD AUC insulin Insulin receptor expression (skeletal muscle) 150 200 100 100 * 50 0 0 saline nicotine saline nicotine What causes nicotine-induced dysglycemia? Reduced beta cell mass? Reduced insulin effect at target tissues? Reduced beta cell function? Beta cell function: Glucose stimulated insulin secretion (islets) * 3.3 mmol glucose (basal) 16.7 mmol glucose (stimulated) Islet cells from nicotine-exposed animals are unable to release insulin in response to a glucose stimulus What causes nicotine-induced dysglycemia? Reduced beta cell mass? Reduced insulin effect at target tissues? Reduced beta cell function? Does in utero exposure to cigarette smoke affect postnatal health in humans? • Increased risk of obesity Ino T. 2010. Maternal smoking during pregnancy and offspring obesity: Meta-analysis. Pediatrics International 52: 94-99 • Increased risk of hypertension Power C et al. 2010. Maternal smoking in pregnancy, adult adiposity and other risk factors for cardiovascular disease. Atherosclerosis 211: 643-648. • Increased risk of type 2 diabetes Montgomery SM and Ekbom A. 2002. Smoking during pregnancy and diabetes mellitus in a British longitudinal birth cohort. BMJ 324: 26-27. Summary of studies assessing maternal smoking and diabetes risk in the offspring 1 Conclusions Fetal and neonatal exposure to nicotine results in increased postnatal body weight and adiposity The metabolic phenotype of nicotineexposed animals is consistent with what is seen in children born to women who smoked during pregnancy What about other smoking cessation drugs? Two non-NRTs approved for use for smoking cessation •Varenicline •Bupropion (Champix®) http://www.medix24.com/french/ images/champix-box.jpg (Zyban®) http://www.tristatemeds.com/upl oad/zyban_box1.jpg Smoking cessation pharmacotherapies nAChR Nicotine Full agonist Varenicline Partial agonist Bupropion Antagonist Beta cell function: Glucose stimulated insulin secretion (INS-1E cells) Insulin release (% of control at 3.3 mM glucose) 300 3.3 mmol glucose (basal) * 16.7 mmol glucose (stimulated) 250 200 150 100 50 0 Control Nicotine (1µM) Beta cell function: Glucose stimulated insulin secretion (INS-1E cells) 3.3 mmol glucose (basal) Insulin release (% of control at 3.3 mM glucose) 300 16.7 mmol glucose (stimulated) * 250 200 150 100 50 0 Control Nicotine (1µM) Varenicline (1µM) Beta cell function: Glucose stimulated insulin secretion (INS-1E cells) Insulin release (% of control at 3.3 mM glucose) 300 3.3 mmol glucose (basal) * 16.7 mmol glucose (stimulated) 250 200 150 100 50 0 Control Nicotine (1µM) Varenicline (1µM) Bupropion 1µM Beta cell function: Glucose stimulated insulin secretion (INS-1E cells) 3.3 mmol glucose (basal) Insulin release (% of control at 3.3 mM glucose) 300 16.7 mmol glucose (stimulated) * * 250 200 150 100 50 0 Control Nicotine (1µM) Varenicline (1µM) Bupropion 1µM Mecamylamine 100µM Bupropion use in pregnancy Bupropion is the most commonly prescribed non-SSRI antidepressant for use during pregnancy and during the post-partum period Andrade et al., 2008 Am J Obstet Gynecol 198: 194.e1-194.e5 % of pregnancies 6 5 4 3 2 1 0 SSRI TCA bupropion other Effect of fetal and neonatal exposure to bupropion (Zyban®) Saline Bupropion (5 or 10mg/kg/d) 2 wks Mating 3 wks 3 wks Parturition (PND1) Outcome measures to determine changes related to: Weaning (Week 3) Obesity T2DM 6 months: Endpoint Bupropion exposure does not increase adiposity in the offspring . Outcome measure Control Bupropion Bupropion 5mg/kg 10mg/kg P-value Body weight (g) 563.6 ± 13.1 607.6 ± 11. 9 574.7 ± 1 5.0 P=0.06 Mesenteric fat pad weight (g) 6.8 ± 0. 6 7.9 ± 0.6 7.2 ± 0.7 P=0.43 Perirenal fat pad weight (g) 13.0 ± 0. 6 15.5 ± 1.0 Epididymal fat pad weight (g) 7.3 ± 0.9 8.8 ± 0.6 7.6 ± 1. 2 P=0.46 Total fat pad weight (g) 27.0 ± 1. 8 32.2 ± 1.7 28.8 ± 3.6 P=0.33 Total fat (% of body wt) 4.8 ± 0.2 5.3 ± 0.3 4.9 ± 0.5 P=0.58 Data are presented as mean ± SEM. Reprod Sci. 2013 Oct;20(10):1156-61 14.0 ± 1.8 P=0.3 5 Glucose homeostasis GTT 22 Control Bupropion 5mg/kg/d Bupropion 10mg/kg/d 20 Glucose (mmol/l) 18 16 14 12 10 8 6 4 0 20 40 60 Time (minutes) 80 100 120 140 Conclusion Bupropion exposure during fetal and neonatal development did not affect metabolic homeostasis in the offspring Fetal and neonatal nicotine exposure may adversely affect the health of the offspring and raise concerns regarding the safety of NRT use during pregnancy What next? 25 * 20 15 10 5 0 Control Nicotine Experimental Groups N Ma, DB Hardy and AC Holloway, unpublished data Hepatic FAS: -actin mRNA Levels Hepatic triglyceride levels (mg/g) Examine why nicotine-exposed animals have dyslipidemia FAS 8 * 6 4 2 0 Control Nicotine Experimental Groups Acknowledgements Students and Staff Dr. Jenny Bruin Amanda Woynillowicz Bryce Poirier Jillian Hyslop Nicole DeLong Edward Hadzocos Igal Raizman Gareth Lim Lisa Kellenberger Alex Petre Sandra Stals Bart Hettinga Staff of the CAF Collaborators Dr. Yu-Jing Gao Dr. Jim Petrik Dr. Hertzel Gerstein Dr Dan Hardy Dr Robert Lee Dr Katherine Morrison Dr Sandeep Raha FUNDING Bupropion? nAChR Nicotine Full agonist Bupropion (Zyban®) Antagonist