Antiprotozoal drugs_E
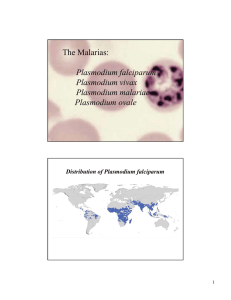
advertisement

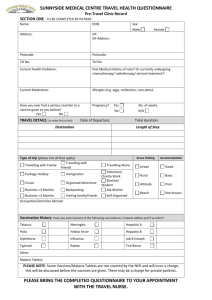
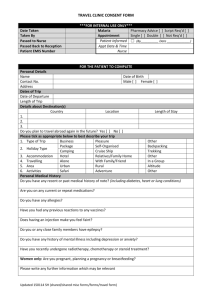
Medical University of Sofia, Faculty of Medicine Department of Pharmacology and Toxicology Antiprotozoal drugs (Abstract) Assoc. Prof. Ivan Lambev e-mail: itlambev@mail.bg 1. Malaria Malaria is the most important of the transmissible parasitic diseases. Over 90 million cases occur each year. DRUG-RESISTANT MALARIA Plasmodium falciparum is now resistant to chloroquine in many parts of the world. Areas of high risk for resistant parasites include Sub-Saharan Africa, Latin America, Oceania, and some parts of South-East Asia. Chloroquine-resistant Plasmodium vivax is also reported. The incubation period of malaria is 10–35 days. Female anopheles mosquitoes require a blood meal for egg production and in the process of feeding they inject salivary fluid containing sporozoites into humans. Since no drugs are effective against sporozoites, infection with the malaria parasite cannot be prevented. Hepatic cycle Sporozoites enter liver cells where they develop into tissue (liver) schizonts which form large numbers of merozoites which, usually after 5–16 days but sometimes after months or years, are released into the circulation. Plasmodium falciparum differs in that it has no persistent hepatic cycle. Primaquine, proguanil, and tetracyclines (tissue schizonticides) act at this site and are used for: • Radical cure, i.e. an attack on persisting hepatic forms. This is most effectively accomplished with primaquine. • Preventing the initial hepatic cycle. This is also called causal prophylaxis. Primaquine may be used safely; proguanil is weakly effective; doxycycline may be used short-term. Erythrocyte cycle Merozoites enter red cells where they develop into blood schizonts which form more merozoites which are released when the cells burst giving rise to the features of the clinical attack. The merozoites reenter red cells and the cycle is repeated. Chloroquine, quinine, mefloquine, halofantrine, proguanil, pyrimethamine, and tetracyclines (blood schizontocides) kill these asexual forms. Drugs which act at this stage in the cycle may be used for: • Treatment of acute attacks of malaria. • Prevention of attacks by early destruction of the erythrocytic forms. This is called suppressive prophylaxis as it does not cure the hepatic cycle. Sexual forms Some merozoites differentiate into male and female gametocytes in the erythrocytes and can develop further only if they are ingested by a mosquito where they form sporozoites and complete the transmission cycle. Quinine, mefloquine, chloroquine, artesunate, artemether and primaquine (gametocytocides) act on sexual forms and prevent transmission of the infection because the patient becomes noninfective and the parasite fails to develop into mosquito. In summary, drugs may be selected for: • treatment of clinical attacks • prevention of clinical attacks • radical cure. Life cycle of malaria parasites •Pl. falciparum •Pl. malariae •Pl. ovale •Pl. vivax Quinine as cinchona bark was introduced into Europe from South America in 1633. It was used for all fevers, amongst them malaria. Further advance in the chemotherapy of malaria was delayed until 1880, when Charles Louis Alphonse Laveran, Prof. of Military Medicine in Paris (Nobel prize winner 1907) finally identified the parasites in the blood. Quinine (Chinine) is an alkaloid, obtained from the bark of the South American Cinchona tree. It binds to plasmodial DNA to prevent protein synthesis. It is used to treat Plasmodium falciparum malaria in areas of multiple-drug resistance. Apart from its antiplasmodial effect, quinine is used for myotonia and muscle cramps because it prolongs the muscle refractory period. Quinine is included in dilute concentration in tonics and aperitifs for its desired bitter taste. Adverse effects include tinnitus, diminished auditory acuity, headache, blurred vision, nausea, and diarrhoea. Idiosyncratic reactions include pruritus, urticaria, and rashes. Hypoglycemia may be significant when quinine is given by i.v. infusion. Amodiaquine is closely related to chloroquine, and it probably shares its mechanisms of action and resistance. Amodiaquine has been widely used to treat malaria because of its low cost, limited toxicity, and, in some areas, effectiveness against chloroquineresistant strains of P. falciparum. Important toxicities of amodiaquine, including agranulocytosis, aplastic anemia, and hepatotoxicity, have limited use, but serious toxicity is rare. Chloroquine is concentrated within parasitised red cells and forms complexes with plasmodial DNA. It is active against the blood forms and also the gametocytes (formed in the mosquito) of Plasmodium vivax, Plasmodium ovale, and Plasmodium malariae. It is ineffective against many strains of Plasmodium falciparum and also its immature gametocytes. Chloroquine is readily absorbed from the GIT and is concentrated several-fold in various tissues, e.g. erythrocytes, liver, spleen, heart, kidney, cornea, and retina. The long t1/2 (50 d) reflects slow release from these sites. Chloroquine is partly inactivated by metabolism and the remainder is excreted unchanged in the urine. Adverse effects are infrequent at doses normally used for malaria prophylaxis and treatment, but are more common with the higher or prolonged doses given for resistant malaria or for rheumatoid arthritis or lupus erythematosus. Corneal deposits of chloroquine may cause halos around lights or photophobia. These reverse when the drug is stopped. Retinal toxicity may be irreversible. In the early stage it takes the form of visual field defects; late retinopathy classically gives the picture of macular pigmentation surrounded by a ring of pigment. The functional defect can take the form of scotomas, photophobia, defective colour vision resulting, in the extreme case, in blindness. Other reactions include pruritus (which may be intolerable), headaches, GI disturbance, precipitation of acute intermittent porphyria in susceptible individuals, mental disturbances and interference with cardiac rhythm; especially if the drug is given i.v. in high dose (it has a quinidine-like action). Long-term use is associated with reversible bleaching of the hair and pigmentation of the hard palate. Halofantrine (t1/2 2.5 d) is active against the erythrocytic forms of all four Plasmodium species, and at the schizont stage. It is used for the treatment of uncomplicated chloroquine-resistant Plasmodium falciparum and Plasmodium vivax malaria. Halofantrine may cause GI adverse effects; pruritus (but to a lesser extent than with chloroquine). It prolongs the cardiac QT interval and may predispose to arrhythmia. Mefloquine (t1/2 21 d) is similar in several respects to quinine. It is used for malaria chemoprophylaxis, to treat Pl. falciparum and chloroquine-resistant Pl. vivax malaria. It should not be given to patients with hepatic or renal impairment. Adverse effects include nausea, dizziness, vomiting, abdominal pain, diarrhoea, and loss of appetite. More rarely, hallucinations, seizures, and psychoses are observed. Primaquine acts at several stages in the development of the plasmodial parasite, possibly by interfering with its mitochondrial function. Its unique effect is to eliminate the hepatic forms of Plasmodium vivax and Plasmodium ovale after standard chloroquine therapy, but only when the risk of reinfection is absent. Adverse effects: anorexia, nausea, abdominal cramps, methaemoglobinaemia and haemolytic anaemia, especially in patients with genetic deficiency of erythrocyte glucose-6-phosphate dehydrogenase (G6PD). Subjects should be tested for G6PD and, in those that are deficient, the risk of haemolytic anaemia is greatly reduced by giving primaquine in reduced dose. Proguanil (t1/2 17 h) inhibits dihydrofolate reductase which converts folic to folinic acid, deficiency of which inhibits plasmodial cell division. Plasmodia, like most bacteria and unlike humans, cannot make use of preformed folic acid. Pyrimethamine and trimethoprim, which share this mode of action, are collectively known as the “antifols”. Their plasmodicidal action is markedly enhanced by combination with sulphonamides or sulphones because there is inhibition of sequential steps in folate synthesis. Poguanil must be used daily when given for prophylaxis, its main use, particularly in pregnant women (with folic acid 5 mg/d). Antifols Pyrimethamine (t1/2 4 d) inhibits plasmodial dihydrofolate reductase, for which it has a high affinity. It is well absorbed from the GIT and is extensively metabolized. Pregnant women should receive supplementary folic acid when taking pyrimethamine. Adverse effects reported include anorexia, abdominal cramps, vomiting, ataxia, tremor, seizures, and megaloblastic anaemia. Pyrimethamine acts synergistically with Sulfadoxine (as Fansidar®) to inhibit folic acid metabolism; sulfadoxine is excreted in the urine. The combination is chiefly used with quinine to treat acute attacks of malaria caused by susceptible strains of Pl. falciparum. Artesunate and artemether are soluble derivatives of artemisinin which is isolated from the leaves of the Chinese herb Artemisia annua. They act against the blood, including sexual forms of plasmodia and may also reduce transmissibility. Artesunate (i.v.) and artemether (i.m.) are rapidly effective in severe and multidrug-resistant malaria. They are well tolerated but should be used with caution in patients with chronic cardiac disorders as they prolong the PR and QT interval in some experimental animals. Doxycycline is commonly used in the treatment of falciparum malaria in conjunction with quinidine or quinine, allowing a shorter and better-tolerated course of quinine. Riamet® tablets contain artemether and lumefantrine. These are both antimalarial medicines. It is used for treatment of uncomplicated Pl. falciparum malaria in adults, children and infants weighing 5 kg and above. 2. Amoebiasis Infection occurs when mature cysts of E. histolytica are ingested and pass into the colon where they divide into trophozoites. Amoebiasis occurs in two forms, both of which need treatment. • Bowel lumen amoebiasis is asymptomatic and trophozoites (noninfective) and cysts (infective) are passed into the faeces. Treatment is directed at eradicating cysts with a luminal amoebicide; diloxanide furoate is the drug of choice; iodoquinol or paromomycin is sometimes used. Paromomycin is an aminoglycoside antibiotic that is not significantly absorbed from the GIT. It is used only as a luminal amebicide and has no effect against extraintestinal amebic infections. The small amount absorbed is slowly excreted unchanged. However, the drug may accumulate with renal insufficiency and contribute to renal toxicity. Paromomycin is an effective luminal amebicide that appears to have similar efficacy and probably less toxicity than other agents. • Tissue-invading amoebiasis gives rise to dysentery, hepatic amoebiasis, and liver abscess. A systemically active drug (tissue amoebicide) effective against trophozoites must be used, e.g. dehydroemetine, metronidazole, tinidazole. In severe cases of amoebic dysentery, tetracycline lessens the risk of opportunistic infection, perforation, and peritonitis when it is given in addition to the systemic amoebicide. Dehydroemetine (from Ipecacuanha), less toxic than the parent emetine, is claimed to be the most effective tissue amoebicide. Dehydroemetine inhibits protein synthesis. It is reserved for dangerously ill patients, but these are more likely to be vulnerable to its cardiotoxic effects. When dehydroemetine is used to treat amoebic liver abscess, chloroquine should also be given. Metronidazole, a nitroimidazole, is the drug of choice in the treatment of extraluminal amebiasis. It kills trophozoites but not cysts of E. histolytica and effectively eradicates intestinal and extraintestinal tissue infections. It has anaerobic antibacterial activity and antihelicobacater activity too. It is an enzyme inhibitor. Tinidazole appears to have similar activity and a better toxicity profile than metronidazole, and it offers simpler dosing regimens. 3. African trypanosomiasis (sleeping disease) It is caused by the hemoflagellates Trypanosoma brucei rhodesiense and Trypanosoma brucei gambiense. The organisms are transmitted by bites of tsetse flies (genus Glossina), which inhabit shaded areas along streams and rivers. The largest number of cases is in the Congo. Annual incidence estimates are about 100 000 cases and 48 000 deaths. American Trypanosomiasis (Chagas’ Disease) is caused by Trypanosoma cruzi. African trypanosomiasis – treatment: Suramin or pentamidine is effective during the early stages but not for the later neurological manifestations for which melarsoprol should be used. Eflornithine is effective for both early and late stages. American Trypanosomiasis – treatment: Prolonged (1–3 months) treatment with benznidazole or nifurtimox may be effective. 4. Leishmaniasis is a zoonosis. •Visceral leishmaniasis (kala azar) is caused mainly by Leishmania donovani in the Indian subcontinent and East Africa. Treatment: Sodium stibogluconate or meglumine antimoniate; resistant cases may benefit from combining antimonials with allopurinol, pentamidine, paromomycin, or amphotericin B. •(Muco-) Cutaneous leishmaniasis is caused mainly by Leishmania tropica, L. major, and L. donovani. Treatment: Mild lesions heal spontaneously, antimonials may be injected intralesionally. 5. Toxoplasmosis T. gondii, an obligate intracellular protozoan, is found worldwide in humans and in many species of animals and birds. The definitive hosts are cats. Humans are infected after ingestion of cysts in raw or undercooked meat, ingestion of oocysts in food or water contaminated by cats, transplacental transmission of trophozoites or, rarely, direct inoculation of trophozoites via blood transfusion or organ transplantation. Life cycle of Toxoplasma gondii Most infections are self-limited in the immunologically normal patient. Pyrimethamine with sulfadiazine is used for treattement of chorioretinitis, and active toxoplasmosis in immunodeficient patients; folinic acid is used to counteract the fatal megaloblastic anaemia. Alternatives include pyrimethamine with clindamycin or clarithromycin or azithromycin. Spiramycin is for treeatment of primary toxoplasmosis in pregnant women. Expert advice is essential. 6. Human Trichomoniasis (Metronidazole or tinidazole is effective) Human trichomoniasis caused by Tr. vaginalis, seen in both females and males. It is usually transmitted by coitus and is sometimes asymptomatic. The symptomatic condition in females may take the form of a severe vaginitis associated with discharge, burning, and pruritus. In males it may produce urethritis, enlargement of the prostate, and epididymitis. 7. Giardiasis It is a common infection of the human small intestine with the protozoan Giardia lamblia, spread via contaminated food or water, or by direct person-to-person contact. Treatment: Metronidazole, mepacrine, or tinidazole 8. Pneumocystis Pneumocystis carinii, the causative agent of interstitial plasma cell pneumonia, which can also cause extrapulmonary disease in immunocompromised patients (AIDS, etc) . Treatment: Co-trioxazole: i.v./p.o. in high daily doses