Prevention, Diagnosis, & Treatment of Key Opportunistic Infections
advertisement
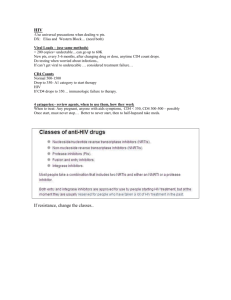
Prevention, diagnosis, and treatment of key Opportunistic Infections in HIV Infection Theodoros Kelesidis UCLA The Late Phase of HIV-1 1400 Plasma viral titer by PCR or bDNA assay Plasma viral titer by culture or p24 antigen + Number of CD4 cells 106 1200 1000 104 800 103 600 102 400 101 200 1 2 9 CD4+ Count Plasma Viremia 105 10 Time (Years) PCR=polymerase chain reaction; bDNA=branched DNA. Adapted with permission from Saag. In: DeVita et al, eds. AIDS: Etiology, Treatment and Prevention. 4th ed. Lippincott-Raven Publishers; 1997:203-213. Risk of Death Associated with ADEs Adjusted Hazard Ratio Herpes simplex 0.97 Mycobacterial disease 5.07 Toxoplasmosis 5.10 Cryptococcosis 9.00 PML 9.56 Non-Hodgkin’s lymphoma 19.31 Mocroft A, and ART Cohort Collaboration CROI 2007# 80. 33 YO with chest pain, fever and productive cough worsening over 3d Candidiasis • Oropharyngeal candidiasis is the most common opportunistic infection in persons infected with HIV • is usually associated with significant immunosuppression (CD4 counts <200 cells/microL) • Topical therapy for the initial episode of oropharyngeal candidiasis in HIV-infected patients with mild disease. • For patients with recurrent infection, moderate to severe disease, or in those with advanced immunosuppression (CD4 <100 cells/microL) (200 mg loading dose, followed by 100 to 200 mg daily for 7 to 14 days after clinical improvement) 37 YO HIV + male CD4 76 as of six months ago, now has DOE, fever, dry cough, and pleuritic chest pain. His symptoms have been progressing over the last month despite 10 days of Levaquin. 38C 120/70,HR120, pulse ox is 69% on room air. Ill appearing, in mild respiratory distress Pneumocystis • We now refer to the organism that causes human disease as pneumocystis jirovecii • In ‘80’s AIDS defining illness for 2/3rds of patients • Ugandan study found 38.6% of 83 pts admitted with pneumonia had PCP on BAL • Presentation: – Gradual onset dyspnea, fever, nonproductive cough, unremarkable lung exam, tachycardia – CXR: Diffuse bilateral interstitial infiltrates, is a leading cause of pneumothorax. – Cavitation, adenopathy and effusion should prompt search for other pathogens Diagnosis of PCP • hypoxemia, elevated LDH nonspecific • induced sputum • BAL • Specific dx should be sought in those with mod-severe disease Treatment • TMP/SMZ treatment of choice • Steroids ASAP but at least within 72 hours if pO2<70 or Aa gradient >35 mm/Hg • Pentamidine is second choice for moderate to severe disease • Discontinue prophylaxis in patients who have responded to ARVs with a CD4 cell >200 sustained for longer than 3 months 39 yo engineer from Belize with right sided weakness, tremor, expressive aphasia, and generalized seizure. Found to be HIV positive, CD4= 32. No history of IVDU. Toxoplasmosis • Most common cause of intracerebral lesions in persons with HIV. • 15-30% of US population is seropositive • 50-75% in some European countries. • Without prophylaxis 30% of seropositive with CD4<50 will develop CNS disease. • 95% of persons with Toxoplasmosis are antibody positive. Toxoplasmosis • Presentation: headache, fever, confusion, focal deficits, and seizures • Differential: CNS lymphoma, abscess, cryptococcoma, tuberculoma DIAGNOSIS – CT or MRI with contrast are not specific, – Serum and CSF IgG/IgM – CSF PCR is specific 96-100%, but sensitivity 50% Toxoplasmosis-Treatment • Pyr + sulfadiazine + leucovorin • Preferred alternative Pyr+ clinda + leucovorin • TMP-SMX which is inexpensive and readily available in developing countries may be suitable first line therapy for acute TE Toxoplasmosis treatment • Acute therapy for 6 weeks, until resolution of contrast enhancement • Adjunctive steroids for mass effect and edema • Chronic Maintenance therapy until CD4>200 x 6 months – Sulfadiazine 2-4 gm + Pyr 25-50 +leucovorin 10-25 Primary Prophylaxis • • • • CD4<100 and Toxoplasma IgG + Discontinue ppx when CD4>200 > 3 months TMP-SMZ SS or DS qd Alternatives – Dapsone + Pyrimethamine q week + Folinic acid q week – Mepron +/_ Pyrimethamine – ? Azithromycin 28YO M, HIV status unknown, brought in by his wife with headache, vomiting and confusion worsening over 9 days. 39.4C, combative, without obvious focal findings. CT with contrast increased intracranial pressure. Likely diagnoses include? a. Cryptococcal meningitis b. Tuberculous meningitis c. Cocci meningitis d. Lymphomatous meningitis e. Bacterial meningitis Cryptococcosis • PreHAART occurred in 6-10% of persons with AIDS in US, Europe & Australia • 7/1000 AIDS pts in 2000 in US • Cause of 20-45% of cases of community acquired meningitis in South Africa, moving ahead of tuberculous meningitis Cryptococcosis • Meningitis or meningoencephalitis is the most common manifestation • Presents with progressive headache, fever, AMS worsening over several weeks may have symptoms of increased ICP. • Meningismus, papillaedema, cranial nerve palsies not uncommon Diagnosis • High organism load in HIV, so India ink usually positive in AIDS, (sensitivity 75-85%) • Cryptococcal antigen high sensitivity 95% and specificity for diagnosis but little utility in assessing response to therapy • 75% with meningitis also have + blood cultures • opening pressure >200mm Hg in 75% • CSF lymphocytic pleocytosis • elevated protein, low glucose • cultures grow in 48-72 hours Use of Lumbar punctures • CT first, always check the opening pressure with each LP • Repeat LP for signs of increased ICP (HA, AMS, visual or hearing loss), may require lumbar drain • Daily LPs to achieve a closing pressure <20 or 50% of the opening pressure • If not improving or new symptoms repeat LP Treatment Guidelines • Preferred induction regimen: 2 weeks of – AmB + flucytosine – Consolidation if CSF culture neg – Fluconazole 400 mg/day x 8 weeks • Maintenance – Fluconazole 200 qd until CD4>200 x 6 months • Combination fluconazole and 5-FC, in small studies had response rates of 60–80%, comparable to ampBbased regimens SM • 59 YO Lebanese male admitted 9/30 with new onset seizures • PMH – pancytopenia with negative work up – PE word finding difficulty, flattening of R nasolabial fold • R hand decreased grip strength, decreased strength biceps • CT showed L frontal enhancing lesion with mass effect and a small R cerebellar enhancing lesion • CT of chest and abdomen showed 2.3 x 1.8 cm mass at the root of the mesentary along the superior mesenteric vessels What tests do you want? • • • • HIV1/2 serology Toxoplasma serology ppd Blood cultures Mycobacterium avium complex (MAC) • Most common bacterial OI in the developed world • 10-20% of persons with AIDS • independent predictor of mortality • Acquired through inhalation or ingestion, spreads through lymphatics • Fevers, night sweats, weight loss, • Labs: anemia, elevated alkaline phosphatase Prophylaxis and treatment • Prophylaxis: Start CD4<50 Stop CD4>100 x 3 months • Azithromycin 1200 q week • Combination therapy is essential resistance seen in 46% after 16 weeks on Clarithromycin alone • Clarithromycin + Ethambutol +/- Rifabutin or • 12 months of treatment and • CD4>100 x more than 6 months Fever in patient with CD4<50 • 34 YO with fever to 102, weight loss, heartburn and diarrhea, no cough, no visual changes, no headache, no marked adenopathy. • Labs: Hct 29, LDH 255, LFTS normal • stool studies show a few red blood cells • Chest x-ray unremarkable Fever in patient with CD4<50 Mycobacterium avium complex Cytomegalovirus Cryptococcus M. tuberculosis Lymphoma Endemic mycoses Epidemiology-CMV • Developed world 40-70% healthy adults infected. • In persons with HIV especially IVDU and MSM, close to 100% are also seropositive for CMV • Autopsy studies show up to 90% of persons dying with HIV in preHAART era had CMV disease • 40% developed sight threatening disease after CD4 dropped to <50 • CMV retinitis Remains the most common cause of visual loss in developed countries Cytomegalovirus Reactivation when CD4<100 • 85% retinitis • 17% GI tract esophagitis, gastritis, duodenitis, colitis • 1% encephalitis, polyneuritis, polyradiculopathy • ?% pneumonitis CMV Treatment • Ganciclovir- IV, PO or intravitreal • Foscarnet- IV, intravitreal • Cidofovir- IV • +/-Prophylaxis if CD4<50 • Preemptive therapy for viremia? • Treatment of symptomatic disease with induction followed by maintenance therapy • In the absence of immune reconstitution drug resistance emerges with serial accumulation of mutations Summary of prophylaxis Infection Preferred drug Indications Pneumocystis carinii pneumonia Trimethoprimsulfamethoxazole (double-strength tablet daily) CD4 count <200 cells/microL; thrush; unexplained fever for more than two weeks; history of PCP Toxoplasmosis Mycobacterium avium complex Trimethoprimsulfamethoxazole (double-strength tablet daily) Azithromycin (1200 mg weekly) CD4 count <100 cells/microL and Toxoplasma seropositive CD4 count <50 cells/microL Take home messages • OIs are the most common presentations of AIDS/HIV • Usually occur when CD4 < 200 • Most important: PCP, MAC, Cryptococcus, Toxoplasma, CMV • Candida infection is the most common OI and MAC is the most common bacterial OI • Life Threatening: PCP, Cryptococcus • Prophylaxis if CD4 <200: bactrim, azithromycin