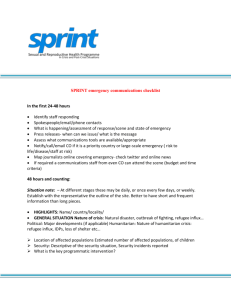
SPRINT's - CCT CORE
advertisement

STABILIZING PATIENTS RAPIDLY FOR INTERFACILITY TRANSPORT: THE SPRINT COURSE Assistance Advisors Burns Jim Johnson MD Christopher Lentz MD Cardiac Charles Bethea MD Raj Chandwaney MD Neurology David L. Gordon MD Anna Wanahita MD Obstetrics Michael Gardner MD Pediatrics Amanda L. Bogie MD Michael Gomez MD Cecilia C. Guthrie MD Surgery & Trauma John Blebea MD Jason Lees MD Michael Charles MD Referring Facility Course overview & “5 W’s” General principles/steps for all patients Principles related to specific diagnoses Recommendations summary Post-course follow-up & plans Discussion outline Receiving Hospital SPRINT overview: 5 W’s • • • • What is SPRINT? Why a new program? Who are audience targets? Where and when are courses? SPRINT general principles Core message: “Fast, Safe, and Sound” – Strive for quickness (while avoiding haste) – Keep patient safety as top priority – Practice sound, evidence-based medicine Goal: Minimize HEMS time at referring hospital – Time HEMS crew spends at patient’s bedside – SPRINT’s focus: “Patient stabilization time” (PST) SPRINT goal: Streamline PST • Efficiency is desirable in any acute patient • Incremental benefit with time savings – Trauma – Vascular emergencies • Categorical endpoint: meeting time window – Percutaneous coronary intervention for STEMI – Lysis therapy for ischemic stroke (iCVA) SPRINT and patient care timeline • SPRINT time frame after transport decision • SPRINT is not intended to address: – Making decision to transport – Determining transport mode/service – Designating receiving facility SPRINT is not meant to dictate transport decisions, modalities, or receiving centers SPRINT steps: Initial information Referring & receiving hospital data • Unit, physician, contact info • Bed status: Ready, not ready, etc. Patient parameters • Name and birthdate • Complaint/transport reason • Height, weight & widest girth SPRINT steps: Initial info Additional clinical parameters • Medications • Equipment (eg. pumps, vent) • Safety (eg. patient agitation) Other issues • Will family be at referring hospital with patient? • Weather questions on referring hospital end SPRINT steps: Logistics & paperwork Prepare the LZ and personnel • Refer to LZ training courses • Prepare to assist crew as needed SPRINT steps: Airway • #1 issue (for flight crews & receiving doctors) • Endotracheal intubation (ETI) problems: – HEMS ETI is widely perceived as too frequent – Flight crew ETI is associated with prolonged PST • Flight crew can offer significant ETI expertise • Decision on ETI pre-transport vs. in-flight: – Estimation of ETI difficulty isn’t always precise – Patient and logistics factors contribute to decision – Bottom line: Situational judgment is best • Guides to assist referring providers: – If airway needs management, manage it – When in doubt, secure airway • Discuss prn with en route crews • When airway is managed – Describe difficulties to crew – Note airway, size, and depth SPRINT steps: Airway SPRINT steps: Breathing • Breathing problem: manage airway • Mechanical ventilation preferred • Optimize/report vent settings • Vascular access – 2 functioning and secured lines usually required – If IV access is problematic, alert en route HEMS crew • Fluids: Discuss with receiving; prepare infusates SPRINT steps: Circulation SPRINT steps: Medications • Drug Rx often causes preventable delays • Execute/consider following time savers: – – – – Administer all ordered medications Clarify allergies Anticipate medications that may be needed Alert transport crews to drugs/times given: Antibiotics Analgesics Sedatives Paralytics Cardiovascular support (cardio-/vaso-active agents) Disease-specific therapy SPRINT steps: Other procedures • Gastric tube • Foley catheter • Pneumothorax tx SPRINT steps: Flight crew arrival • • • • • • Crew to pt for pass-off Assure 2 IVs Transfer infusions to HEMS pumps Assure ordered meds given Discuss situation with family Situationally consider: – – – – “ABCs” management Spinal immobilization Analgesia, sedation, antiemetics, other prn meds Foley, gastric tube, Dx-specific therapy SPRINT steps: Patient hand-off 1) Patient demographics 2) Chief complaint & HPI 3) Dx and basic therapies – Labs, radiography, meds – Identify treatment as: • Fully completed • Partly complete • Planned/ordered – Admin times for key meds • • • • Analgesia Antiepileptics Sedation Paralytics 4) Ventilator patients – – – – – Airway/lung assessment ETI medications/problems ETT size, depth ETT confirmation method Vent changes/responses 5) Summarize working dx 6) Ask if report complete 7) Receiving crew review – Presentation key points – Interventions/meds – Points to consider Diagnosis-specific principles Burns Cardiac Neurology Obstetrics Pediatrics Trauma Vascular Streamlining PST: Burns 1) Airway: “Aggressive can be conservative” – Inhalational/airway, facial burns: ETI likely – Save PST on by managing airway early 2) Fluids (warm if possible) – Use formula (BRI, Parkland) to calculate fluids – Monitor and report urine output 3) Dressings: Use minimalist approach 4) Thermoregulation: Keep patients warm Streamlining PST: STEMI for PCI 1) Administer meds – ASA almost always – No clopidogrel – Heparin bolus 50-70 u/kg 2) No IV infusions – No heparin drip – No nitroglycerin drip 3) Consider R-sided EKG 4) Gown patient Streamlining PST: Seizures 1) Stop seizures 2) Report what worked (and when) 3) Avoid paralytics Streamlining PST: Stroke 1) Avoid paralytics 2) Generate BP plan – Hemorrhage mgmt? – Lysis-eligible: 185/110 – Post-lysis: 180/105 Streamlining PST: Obstetrics 1) 2) 3) 4) Transport by air?: Contractions and cervix Perfusion: left lateral decubitus position Analgesics and antiemetics (both are fine) BP control: Formulate plan and start treating Streamlining PST: Pediatrics Airway: Intubate if needed Watch tube size/depth Streamlining PST: Pediatrics • VS: Pay attention to BP cuff, SpO2 site, temp • Fluids: Make plan for fluids and have them ready Streamlining PST: Trauma Airway, breathing, and circulation • • • • Consider managing airway Assure IV access in place Foley catheters Assure infusates (e.g. blood) are ready Spinal immobilization • In unclear cases: fully immobilize • Discuss with receiving surgeon • Clarify why spine (or parts) cleared Streamlining PST: Trauma 1) Fractures: Splint, treat pain 2) Guard against hypothermia 3) Pneumothorax/chest tubes – Thoracostomy: Heimlich valve – Pneumothorax: Decompress? Streamlining PST: Vascular 1) Cold extremities: Time is key – Clarify time of sx onset – Heparin bolus/infusion: almost always 2) Aortic disease (non-trauma) – Large-bore access; judicious analgesia – Permissive hypotension (AAA) – Anti-impulse Rx (dissection) • Decision to transfer → T0 • Execute logistics/admin jobs Summary • Develop a concrete clinical plan • Provide ordered and/or needed Tx • Expedite the report to transport crew • Facilitate movement to transport vehicle SPRINT: Post-course SThomasMD@GMail.com Thanks for your time – and for your time savings