Pharmacologic Options in the Invasive
advertisement

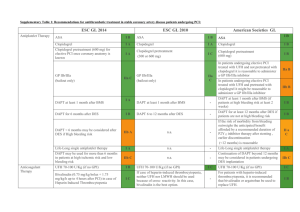
Pharmacologic Options in the Invasive Management of Acute Coronary Syndrome Ross J. Goodfellow, DO FACC FSCAI Health First Medical Group Cape Canaveral Hospital/Holmes Regional Medical Center Cocoa Beach & Melbourne, Florida Disclosures • Speaker • Astra Zeneca • Zoll Medical Acute Coronary Syndrome (UA, NSTEMI, STEMI) • 2014 • • Majority of patients undergo invasive strategy (cardiac cath within 24-48 hrs) FRISC-II, RITA, ICTUS • Meta-analysis demonstrated 19% RRR in CV Death or MI in patients managed with early invasive strategy Risk Stratification: TIMI Risk Score • Age 65 or older • 3 or more CAD risk factors • DM, Smoking, HTN, HDL<40mg/dl, FamHx of premature CAD • Known CAD • ASA use in past 7 days • 2 or more anginal episodes in 24 hours • ST changes > 0.5mV • Positive cardiac biomarkers ACS Pharmacology: Invasive Strategy • Decrease myocardial demand/increase supply • Beta Blockers, Nitrates, Calcium Channel Blockers • Analgesics • Morphine • Oral Antiplatelet Agents • ASA, Clopidogrel, Prasugrel, Ticagrelor • Intravenous Antiplatelet Agents • IIb/IIIa Antagonists (Abciximab, Eptifibitide, Tirofiban) • Anticoagulants • Heparin, Bivalirudin, LMWH (Enoxaparin, Dalteparin) Sites of action of antiplatelet and anticoagulant medications1 ANGIOMAX Platelet activation GP IIb/IIIa inhibitors Heparin LMWH AT Thrombin AT Factor Xa Aspirin and Thienopyridines ADP/TXA2 mediated platelet adhesion Fibrinogen Prothrombin Plasma clotting factors Collagen 1. Monroe DM et al. Arterioscler Thromb Vasc Biol 2002;22:1381-9 Tissue factor Platelet aggregation Fibrin Vessel Injury 8 Enoxaparin v. UFH • Meta-analysis of all trials demonstrates a 10% reduction in death or MI with enoxaparin over UFH • No significant differences in major bleedings • Meta-analysis included conservatively managed patients • Largest trial of invasively treated patients (SYNERGY) showed increased bleeding with enoxaparin Oral Antiplatelet Agents • ADP-P2Y12 interaction • Amplifies platelet activation • P2Y12 receptor antagonists • Thienopyridines • Ticlopidine • Clopidogrel (PLAVIX) • Prasugrel (EFFIENT) • CPTP (Cyclopentyltriazolopyrimidine) • Ticagrelor (BRILINTA) CURE Trial • Unstable angina/NSTEMI • ASA + Clopidogrel (300mg load/75mgqd) v. ASA alone • N=12,562 • 20% RRR in CV Death, MI, and Stroke in Clopidogrel group • Driven by decreased nonfatal MI • PCI-CURE • Clopidogrel pre-treatment (6 days) pre-PCI associated with 31% RRR in primary endpoint PCI-CURE CURRENT-OASIS 7 • Rationale • Attempt to address high on-treatment platelet reactivity seen in 10-30% pts. • Double-dose clopidogrel load/maintenance dose x 7 days v. standard dose in ACS pts. • 2 x 2 design also assessing ASA dose Wiviott SD et al AHJ 152: 627,2006 Study Design ACS (STEMI or UA/NSTEMI) & Planned PCI ASA N= 13,600 Double-blind CLOPIDOGREL 300 mg LD/ 75 mg MD PRASUGREL 60 mg LD/ 10 mg MD Median duration of therapy - 12 months 1o endpoint: CV death, MI, Stroke 2o endpoints: CV death, MI, Stroke, Rehosp-Rec Isch CV death, MI, UTVR Stent Thrombosis (ARC definite/prob.) Safety endpoints: TIMI major bleeds, Life-threatening bleeds Key Substudies: Pharmacokinetic, Genomic Enrollment Criteria •Inclusion Criteria Planned PCI for : Known Mod-High Risk UA/NSTEMI (TRS > 3) Anatomy STEMI: < 14 days (ischemia or Rx strategy) STEMI: Primary PCI •Major Exclusion Criteria: –Severe comorbidity –Increased bleeding risk –Prior hemorrhagic stroke or any stroke < 3 mos –Any thienopyridine within 5 days –No exclusion for advanced age or renal function Wiviott SD et al AHJ 152: 627,2006 Primary Endpoint CV Death,MI,Stroke 15 Primary Endpoint (%) Clopidogrel 12.1 (781) 9.9 (643) 10 Prasugrel HR 0.81 (0.73-0.90) P=0.0004 HR 0.80 P=0.0003 5 HR 0.77 P=0.0001 NNT= 46 LTFU = 14 (0.1%) ITT= 13,608 0 0 30 60 90 Wiviott SD et al NEJM 357: 2001, 2007 180 Days 270 360 450 Components of Endpoints Clopidogrel Prasugrel HR 12.1 9.9 0.81 CV Death 2.4 2.1 0.89 Nonfatal MI 9.5 7.3 0.76 1.0 1.0 1.02 CV Death, MI, Stroke Nonfatal Stroke 3.2 0.95 3.0 All Cause Mortality uTVR Stent Thrombosis 0.5 Prasugrel Better 1 HR 3.7 2.5 0.66 2.4 1.1 0.48 Clopidogrel Better 2 Wiviott SD et al NEJM 357: 2001, 2007 Balance of Efficacy and Safety 138 events 15 Clopidogrel 12.1 Endpoint (%) CV Death / MI / Stroke 9.9 10 HR 0.81 (0.73-0.90) P=0.0004 NNT = 46 Prasugrel 5 TIMI Major NonCABG Bleeds Prasugrel 35 events 2.4 1.8 Clopidogrel 0 0 30 60 90 180 Days 270 360 450 HR 1.32 (1.03-1.68) P=0.03 NNH = 167 Wiviott SD et al NEJM 357: 2001, 2007 Bleeding Events Safety Cohort (N=13,457) 3.0 ICH in Pts w Prior Stroke/TIA (N=518) Clopidogrel 2.4 Prasugrel 2.3 Clop 0 (0) % Pras 6 (2.3)% (P=0.02) % Events 1.8 1.4 1.5 0.9 0.9 1.1 0.8 0.0 0.4 0.1 TIMI Major Bleeds ARD 0.6% HR 1.32 P=0.03 NNH=167 Life Threatening ARD 0.5% HR 1.52 P=0.01 Nonfatal ARD 0.2% P=0.23 Fatal 0.3 0.3 ICH ARD 0.3% P=0.002 ARD 0% P=0.74 Wiviott SD et al NEJM 357: 2001, 2007 Net Clinical Benefit Death, MI, Stroke, Major Bleed (non CABG) 15 Clopidogrel ITT= 13,608 13.9 Endpoint (%) 12.2 Prasugrel 10 HR 0.87 P=0.004 Events per 1000 pts + 9 6 All Cause Mortality 0 5 -9 -19 -28 -23 Major Bleed (non CABG) MI 0 0 30 60 90 180 Days 270 360 Clop 3.2% Pras 3.0 % P=0.64 450 Wiviott SD et al NEJM 357: 2001, 2007 CV Death, MI, Stroke Major Subgroups UA/NSTEMI STEMI Reduction in risk (%) 18 21 B Male Female 21 12 <65 Age 65-74 >75 25 14 6 No DM DM 14 30 BMS DES 20 18 GPI No GPI 21 16 CrCl < 60 CrCl > 60 14 20 0.5 Pinter = NS 19 OVERALL Prasugrel Better 1 HR Clopidogrel Better 2 Wiviott SD et al NEJM 357: 2001, 2007 Net Clinical Benefit Bleeding Risk Subgroups Post-hoc analysis Risk (%) Prior Stroke / TIA + 54 Yes Pint = 0.006 No -1 >=75 Age Pint = 0.18 < 75 Wgt -16 -16 +3 < 60 kg Pint = 0.36 >=60 kg -14 -13 OVERALL 0.5 1 Prasugrel Better HR 2 Clopidogrel Better Wiviott SD et al NEJM 357: 2001, 2007 August 30, 2009 at 08.00 CET Ticagrelor (AZD 6140): an oral reversible P2Y12 antagonist HO N N N H N HO O F N N S Ticagrelor is a cyclo-pentyltriazolo-pyrimidine (CPTP) F OH • – – – • – – – Direct acting Not a prodrug; does not require metabolic activation Rapid onset of inhibitory effect on the P2Y12 receptor Greater inhibition of platelet aggregation than clopidogrel Reversibly bound Degree of inhibition reflects plasma concentration Faster offset of effect than clopidogrel Functional recovery of all circulating platelets PLATO study design NSTE-ACS (moderate-to-high risk) STEMI (if primary PCI) Clopidogrel-treated or -naive; randomised within 24 hours of index event (N=18,624) Clopidogrel If pre-treated, no additional loading dose; if naive, standard 300 mg loading dose, then 75 mg qd maintenance; (additional 300 mg allowed pre PCI) Ticagrelor 180 mg loading dose, then 90 mg bid maintenance; (additional 90 mg pre-PCI) 6–12-month exposure Primary endpoint: CV death + MI + Stroke Primary safety endpoint: Total major bleeding PCI = percutaneous coronary intervention; ASA = acetylsalicylic acid; CV = cardiovascular; TIA = transient ischaemic attack Cumulative incidence (%) K-M estimate of time to first primary efficacy event (composite of CV death, MI or stroke) 13 12 11 10 9 8 7 6 5 4 3 2 1 0 11.7 Clopidogrel 9.8 Ticagrelor HR 0.84 (95% CI 0.77–0.92), p=0.0003 0 60 120 180 240 300 360 Days after randomisation No. at risk Ticagrelor 9,333 8,628 8,460 8,219 6,743 5,161 4,147 Clopidogrel 9,291 8,521 8,362 8,124 6,743 5,096 4,047 K-M = Kaplan-Meier; HR = hazard ratio; CI = confidence interval Hierarchical testing major efficacy endpoints All patients* Primary objective, n (%) CV death + MI + stroke Secondary objectives, n (%) Total death + MI + stroke CV death + MI + stroke + ischaemia + TIA + arterial thrombotic events Myocardial infarction CV death Stroke Total death Ticagrelor (n=9,333) Clopidogrel (n=9,291) HR for (95% CI) 864 (9.8) 1,014 (11.7) 0.84 (0.77–0.92) <0.001 901 (10.2) 1,065 (12.3) 0.84 (0.77–0.92) <0.001 1,290 (14.6) 1,456 (16.7) 0.88 (0.81–0.95) <0.001 504 (5.8) 353 (4.0) 125 (1.5) 593 (6.9) 442 (5.1) 106 (1.3) 0.84 (0.75–0.95) 0.79 (0.69–0.91) 1.17 (0.91–1.52) 0.005 0.001 0.22 399 (4.5) 506 (5.9) 0.78 (0.69–0.89) <0.001 The percentages are K-M estimates of the rate of the endpoint at 12 months. p value† Secondary efficacy endpoints over time Cardiovascular death Myocardial infarction 7 Clopidogrel 6 6 5.8 5 Ticagrelor 4 3 2 1 HR 0.84 (95% CI 0.75–0.95), p=0.005 0 0 60 120 180 240 300 360 Cumulative incidence (%) Cumulative incidence (%) 7 6.9 Clopidogrel 5 4.0 4 Ticagrelor 3 2 1 HR 0.79 (95% CI 0.69–0.91), p=0.001 0 0 60 120 180 240 300 360 Days after randomisation Days after randomisation No. at risk 5.1 Ticagrelor 9,333 8,678 8,520 8,279 6,796 5,210 4,191 9,333 8,294 8,822 8,626 7119 5,482 4,419 Clopidogrel 9,291 8,560 8,405 8,177 6,703 5,136 4,109 9,291 8,865 8,780 8,589 7079 5,441 4,364 Stent thrombosis (evaluated in patients with any stent during the study) Ticagrelor (n=5,640) Clopidogrel HR (n=5,649) (95% CI) p value 106 (1.9) 0.009 Stent thrombosis, n (%) Definite 71 (1.3) Probable or definite 118 (2.1) Possible, probable, definite 155 (2.8) 0.67 (0.50–0.91) 158 (2.8) 0.75 (0.59–0.95) 0.02 202 (3.6) 0.77 (0.62–0.95) 0.01 *Time-at-risk is calculated from first stent insertion in the study or date of randomisation Time to major bleeding – primary safety event K-M estimated rate (% per year) 15 Ticagrelor 10 Clopidogrel 11.58 11.20 5 HR 1.04 (95% CI 0.95–1.13), p=0.434 0 0 60 120 180 240 300 360 Days from first IP dose No. at risk Ticagrelor 9,235 7,246 6,826 6,545 5,129 3,783 3,433 Clopidogrel 9,186 7,305 6,930 6,670 5,209 3,841 3,479 Total major bleeding 13 12 NS 11.6 Ticagrelor Clopidogrel 11.2 K-M estimated rate (% per year) 11 NS 10 8.9 NS 9 7.9 8 8.9 7.7 NS 7 5.8 6 5.8 5 4 3 2 NS 1 0.3 0.3 0 PLATO major bleeding TIMI major bleeding Red cell transfusion* PLATO lifethreatening/ fatal bleeding Fatal bleeding Major bleeding and major or minor bleeding according to TIMI criteria refer to non-adjudicated events analysed with the use of a statistically programmed analysis in accordance with definition described in Wiviott SD et al. NEJM 2007;357:2001–15; *Proportion of patients (%); NS = not significant Non-CABG and CABG-related major bleeding 9 7.9 8 K-M estimated rate (% per year) Ticagrelor Clopidogrel NS 7.4 7 NS 5.8 6 5.3 p=0.026 5 4 4.5 3.8 p=0.025 2.8 3 2.2 2 1 0 Non-CABG PLATO major bleeding Non-CABG TIMI major bleeding CABG PLATO major bleeding CABG TIMI major bleeding Holter monitoring & Bradycardia related events Holter monitoring at first week Ventricular pauses ≥3 seconds, % Ventricular pauses ≥5 seconds, % Holter monitoring at 30 days Ventricular pauses ≥3 seconds, % Ventricular pauses ≥5 seconds, % Bradycardia-related event, % Ticagrelor (n=1,451) 5.8 2.0 Ticagrelor (n= 985) 2.1 Clopidogrel (n=1,415) 3.6 1.2 Clopidogrel (n=1,006) 1.7 0.8 0.6 Ticagrelor (n=9,235) Clopidogrel (n=9,186) p value 0.01 0.10 p value 0.52 0.60 Pacemaker Insertion 0.9 0.9 p value 0.87 Syncope 1.1 0.8 0.08 Bradycardia 4.4 4.0 0.21 Heart block 0.7 0.7 1.00 Other findings Ticagrelor (n=9,235) Clopidogrel (n=9,186) p value* Any 13.8 7.8 <0.001 With discontinuation of study treatment 0.9 0.1 <0.001 Any 1.4 1.7 0.17 Malignant 1.2 1.3 0.69 Benign 0.2 0.4 0.02 All patients Dyspnoea, % Neoplasms arising during treatment, % *p values were calculated using Fischer’s exact test Conclusions • Reversible, more intense P2Y12 receptor inhibition for one year with ticagrelor in comparison with clopidogrel in a broad population with ST- and non-ST-elevation ACS provides – Reduction in myocardial infarction and stent thrombosis – Reduction in cardiovascular and total mortality – No change in the overall risk of major bleeding Ticagrelor is a more effective alternative than clopidogrel for the continuous prevention of ischaemic events, stent thrombosis and death in the acute and long-term treatment of patients with ACS IIb/IIIa Antagonists • Inhibit >80% of platelet aggregration • Early studies demonstrated short and long term event reduction in ACS patients compared with heparin alone • Driven by reduction in peri-procedural MI • Increased bleeding • Recent Trials • ISAR-REACT 2, EARLY ACS, ACUITY ACUITY Study Design – First Randomization UFH/Enox + GP IIb/IIIa (n=4,603) Moderateand highRisk ACS (n=13,819) Aspirin in all clopidogrel; dosing and timing per local practice R* Bivalirudin + GP IIb/IIIa (n=4,604) Bivalirudin Alone† (n=4,612) Angiography within 72h Moderate- and high-risk unstable angina or NSTEMI undergoing an early invasive strategy (N=13,819) Medical management PCI CABG *Stratified by pre-angiography thienopyridine use or administration †ANGIOMAX alone (with GP IIb/IIIa inhibition reserved for severe breakthrough ischemia and procedural complications during PCI) The safety and effectiveness of ANGIOMAX have not been established in patients with acute coronary syndromes (ACS) who are not undergoing PTCA or PCI. Stone GW et al. N Engl J Med. 2006;355:2203-2216 47 11 Overall ACUITY Management Strategy (N=13,819) Medical Rx (n=4,491) CABG (n=1,539) 11.1% 32.5% 56.4% PCI (n=7,789) UFH/Enox + GP IIb/IIIa N = 2,561 48 12 Stone GW et al. N Engl J Med. 2006;355:2203-2216 Bivalirudin + GP IIb/IIIa N = 2,609 Bivalirudin alone N = 2,619 Primary Results – 30 Days UFH/Enox + GP IIb/IIIa vs. Bivalirudin + GP IIb/IIIa vs. Bivalirudin Alone UFH/Enox+GP IIb/IIIa (N=2561) Bivalirudin+GP IIb/IIIa (N=2609) Bivalirudin alone (N=2619) 30 day events (%) 20% P=.10 13% P=.057 15% P=.16 P=.45 P=.32 P<.001 12% 8% 9% 9% 7% 8% 4% 0% Net clinical outcome 49 16 Composite ischemia Major bleeding (non-CABG) Stone GW et al. Lancet. 2007;369:907-919. Please refer to important ANGIOMAX safety information on slide 28 and see full Prescribing Information Early and Late Mortality UFH/Enox + GP IIb/IIIa vs. Bivalirudin + GP IIb/IIIa vs. Bivalirudin Alone 4.0 30-day Estimate UFH/Enoxaparin + IIb/IIIa Bivalirudin + IIb/IIIa Bivalirudin alone Mortality (%) 3.0 0.9% 1.2% 1.1% P (log rank) — 0.45 0.63 1-year Estimate P (log rank) 3.1% 2.4% 2.2% — 0.70 0.48 p=0.78 2.0 1.0 0.0 0 31 62 92 123 154 185 215 246 277 308 338 369 400 Days from Randomization Data on file, The Medicines Company, Parsippany, NJ. Please refer to important ANGIOMAX safety information on slide 28 and see full Prescribing Information 50 19 Harmonizing Outcomes with Revascularization and Stents in AMI 3602 pts with STEMI with symptom onset ≤12 hours Aspirin, thienopyridine R 1:1 UFH + GP IIb/IIIa inhibitor (abciximab or eptifibatide) Bivalirudin monotherapy (± provisional GP IIb/IIIa) Emergent angiography, followed by triage to… CABG – Primary PCI 3006 pts eligible for stent randomization Paclitaxel-eluting TAXUS stent – Medical Rx R 3:1 Bare metal EXPRESS stent Clinical FU at 30 days, 6 months, 1 year, and then yearly through 3 years; angio FU at 13 months Stone, GW N Engl J Med 2008;358:2218-30. Harmonizing Outcomes with Revascularization and Stents in AMI 3602 pts with STEMI R 1:1 Randomized UFH + GP IIb/IIIa N=1802 28 1-Year FU Eligible 1-Year FU 3-Year FU Bivalirudin N=1800 • • • Not true MI* • • • N=1774 29 N=1771 26 • • • Withdrew • • • 22 46 • • • Lost to FU • • • 53 N=1702 N=1696 17 • • • Withdrew • • • 18 57 • • • Lost to FU • • • 44 N=1628 N=1634 * Biomarkers WNL and no DS >50% by core lab determination (30 day FU only) Stone, GW Lancet 2011 Published online June 13. DOI:10.1016/S0140-6736(11)60764-2 3-Year Major Bleeding (non-CABG)* Bivalirudin alone (n=1800) Heparin + GPIIb/IIIa (n=1802) 12 10.5% Major Bleeding (%) 10 9.4% 8 6.9% 6 6.0% 3-yr HR (95%CI) 4 0.64 (0.51, 0.80) P=0.0001 2 0 0 3 6 9 12 15 18 21 24 27 30 33 36 Months * Intracranial, intraocular, retroperitoneal, access site bleed requiring intervention/surgery, hematoma ≥5 cm, hgb ↓ ≥3g/dL with or ≥4g/dL w/o overt source; reoperation for bleeding; or blood product transfusion Stone, GW Lancet 2011 Published online June 13. DOI:10.1016/S0140-6736(11)60764-2 Time in Months ' Time in Months 3-Year Cardiac Mortality Heparin + GPIIb/IIIa (n=1802) 3-yr HR (95%CI) 0.56 (0.40, 0.80) P=0.001 6 5 Cardiac Mortality (%) Bivalirudin alone (n=1800) 5.1% 4 3.8% 2.9% 3 2 2.1% 1 0 0 3 6 9 12 15 18 21 24 Months Stone, GW Lancet 2011 Published online June 13. DOI:10.1016/S0140-6736(11)60764-2 27 30 33 36 3-Year Reinfarction Bivalirudin alone (n=1800) Heparin + GPIIb/IIIa (n=1802) 10 9 8.2% Reinfarction (%) 8 7 6.2% 6 5 4.4% 4 3 3-yr HR (95%CI) 0.76 (0.59, 0.99) P=0.04 3.6% 2 1 0 0 3 6 9 12 15 18 21 24 Months Stone, GW Lancet 2011 Published online June 13. DOI:10.1016/S0140-6736(11)60764-2 27 30 33 36 Conclusions: Pharmacology Randomization ● In this large-scale, prospective, randomized trial of pts with STEMI undergoing primary PCI, the initial treatment with bivalirudin alone compared to heparin plus GPIIb/IIIa inhibitors at 3 years resulted in: – A significant 36% reduction in major bleeding and a significant 24% reduction in reinfarction, with non significantly different rates of stent thrombosis, TVR and stroke – A significant 44% reduction in cardiac mortality and a 25% reduction in all-cause mortality, the latter representing 18 lives saved per 1000 patients treated with bivalirudin (NNT = 54 to save 1 life) Stone, GW Lancet 2011 Published online June 13. DOI:10.1016/S0140-6736(11)60764-2 Other Issues to Consider... • • Timing of intervention • Emergent v. Urgent (24-48 hours) Access site • • • Femoral, Radial, Brachial Closure device Maintaining access vessel patency (upper extremity) My preferences • Emergency PCI (STEMI, Unstable NSTEMI) • Patient on antiplatelet therapy • Bivalirudin (or UFH) • Reload in ED (Ticagrelor 180mg) • IIb/IIIa antag as “bailout” • Patient antiplatelet naive • Bivalirudin/UFH • Lower threshold to use IIb/IIIa antagonist • Oral antiplatelet on table (Ticagrelor) My preferences (Cont’d) • Delayed angiography/PCI • Bivalirudin/UFH • IIb/IIIa antagonists if markedly rising enzymes • Ticagrelor, Clopidogrel The Future... • CANGRELOR • BRIDGE Trial • Cangrelor “bridging” decreased platelet reactivity in patients with prior stents scheduled for CABG • CHAMPION-PHOENIX Trial • Cangrelor v. Clopidogrel in PCI patients • Early results show decreased ischemic events at 48 hours in cangrelor group v. clopidogrel • Platelet function assays to guide antiplatelet Rx • Pharmacogenomic Studies, etc. QUESTIONS? THE END