PEM|BRS: Signs & Symptoms & Dermatology Dislocation of the
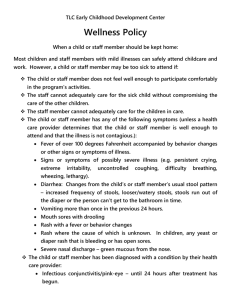
advertisement
PEM|BRS: Signs & Symptoms & Dermatology Dislocation of the patella: presents with knee in flexed position with the patella displaced laterally. Reduction is obtained by extending the knee with simultaneous pressure of the patella medially to reposition it. This can be done in the ED prior to radiographs. Post reduction films should be performed to rule out an avulsion fx. If child with RAD is wheezing and doesn’t respond to 3 nebs, a chest x-ray should be obtained. Oil of wintergreen is commonly used in aromatherapy massage blends for joint and muscle pain. Methyl salicylate is the ingredient of most concern for toxicity. Intoxicated patients will have hyperpnea to compensate for metabolic acidosis. Tinnitus, vomiting, confusion, coma, and bleeding are other common manifestations. Benzocaine toxicity leads to bradydysthrthmias, seizures, and methemoglobinemia Eucalyptus oil toxicity leads to altered mental status, respiratory distress, ataxia, muscle weakness, and dysphagia. Menthol has low toxicity and ill effects are extremely rare. Capsaicin (from chili peppers) is an irritant and causes a burning sensation. Physiologic leukorrhea is a common diagnosis in female neonates with vaginal discharge. Occurring between the 2nd and 3rd week of life as a result of maternal estrogen, the desquamation of epithelial cells presents as a clear or white odorless mucoid discharge. No treatment is necessary. GCS of 13-14 = mild brain injury GCS of 9-12 = moderate brain injury GSC of 8 or less = severe brain injury (automatically intubate) Jimson weed poisoning is common in adolescents because of its hallucinatory properties—think anticholinergic effects (mad as a hatter, dry as a bone, red as a beet, blind as a bat and hot as a hare) due to the atropine components of the plant. Ingestion of poppy seeds can produce a urine test positive for opiates. Morning glory seeds have hallucinogenic properties due to LSD. Ma Huang contains ephedra, which is both a stimulant and thermogenic A retro-orbital tumor or vascular malformation may cause proptosis, which may limit eye movements similar to an entrapment of extraocular muscles in an orbital blowout fracture. 1 A subacute orbital fracture will have enophthalmos instead of exophthalmos. Foods, supplements, and minerals that can cause black tarry stools that do not contain blood, causing false melena: Black licorice, blueberries, spinach, beets, and bismuth and iron preparations. Foods that do not produce melena but produce false positive heme tests are foods containing plant peroxidases such as horseradish, tomatoes, turnips, and fresh red cherries. Henoch-Schonlein Purpura (HSP) or anaphylactoid purpura is a vasculitis that may cause a tetrad: symmetrical palpable petechiae or purpura rash on the buttocks and lower extremities, colicky abdominal pain, arthritis/arthralgia, and hematuria; in children with severe, colicky abdominal pain, must exclude intussusception. Major morbidity is due to renal involvement. Treatment is supportive with NSAID’s, and occasionally steroids or cytotoxic drugs.; Occurs between 3-10 years of age; Due to deposition of IgA on the basement membranes; rash may be on face or upper extremities in children less than 2 years old; All patients need a U/A and should be referred to Renal if abnormal or hospitalized if renal disease and hypertension found. Neonates with seizures that are refractory to anticonvulsants should be considered to have pyridoxine dependent seizures. Occuring almost exclusively in infants younger than 3 months, it is inherited as an AR trait. Therefore, for a neonate in status epilepticus, give 2 doses of ativan (0.1 mg/kg) followed by phenobarb load (20mg/kg) , followed by pyridoxine 100mg IV if still seizing (also check d-stick and lytes) Auricular hematoma from repeated direct trauma needs to be I & D’d, followed by placement of a compression bandage in order to prevent asymmetrical cartilage growth (“cauliflower ear”). Regional and painful lympadenopathy proximal to an inoculation site from a cat is characteristic for cat scratch disease. Lymphadenopathy primarily involves the axillary nodes but may also affect the cervical and inguinal areas. May have constitutional symptoms of fever, malaise, anorexia, and fatigue. Treatment for the lympadenopathy associated with CSD beyond analgesics and warm compresses is unnecessary. For those who are immune compromised, give rifampin, Bactrim, or azithromycin. If the node is tender and fluctuant, needle aspiration may help relieve the pain. Toxicity from TCA’s occurs through a variety of mechanisms. Inhibition of myocyte fast sodium channels leads to prolonged QRS and QT intervals. The alpha- adrenergic blockade properties can lead to hypotension. Through GABA inhibition, you can see seizure, delirium, and coma. Anticholinergic action can give you fever, altered mental status, dry skin, and mucus membranes, and mydriasis. Sodium bicarb enhances protein binding of TCA’s, which results in a decrease in the QRS interval, stabilizing 2 arrhythmias, and increasing BP. This alkinization can also be stimulated by hyperventilation. Digitalis toxicity gives you bradycardia, visual aberrations (color distortions) and syncope. Calcium channel toxicity gives you bradycardia with various degrees of heart block, hypotension, and altered mental status. Phenothiazine OD may give depressed mental status, NMS, and extrapyramidal signs such as dystonic reactions. Organophosphate poisoning causes “DUMB ELFS” through a cholinergic crisis: diarrhea, urination, miosis, bronchorrhea, bronchospasm, emesis, lacrimation, fasciculations, and salivation. Transient synovitis is the most common cause of hip pain in children between the ages of 3-10 years. Symptoms improve within 1-2 days and fully resolve within 7-10 days. Give NSAIDs. Work-up is normal (x-rays and bloodwork) Hemolytic anemia (falling hemoglobin, normal MCV, increased reticulocyte count) can be hereditary (G6PD deficiency, hereditary spherocytosis, sickle cell anemia) or acquired (immune disorders, toxic chemicals and drugs, physical damage, or infections). Secondary teeth that have been avulsed should be re-implanted within 30 minutes of the incident for the best prognosis. First rinse teeth under sterile water and don’t scrub or touch root or crown. Patient should bite down on a piece of gauze to hold the teeth in place while awaiting the dentist. If immediate re-implantation is not possible, teeth should not be allowed to dry—instead, place in milk, viaspan, or hank’s balanced salt solution to preserve the periodontal ligaments of the root surface. Any joint dislocation or fracture resulting in signs of neurovascular compromise (decreased sensation, numbness, pulselessness, decreased capillary refill, abnormal skin color, or cool skin temperature) should be reduced as quickly as possible and should not be delayed by obtaining radiographic studies. For neck masses, a Contrast CT should be performed prior to any operative procedure. A classic hypoxemic “tet spell” results in decreased pulmonary blood flow. Children with Tet spells are at risk of death—therefore these must be immediately recognized and treated with calming, tucking in the knees or squatting, morphine, phenylephrine, oxygen. Fibromatosis colli or a sternocleidomastoid tumor of infancy is due to bleeding into the sternomastoid muscle from birth trauma. This may not be present at birth but may develop up to 3 weeks later as a painless smooth mass. Torticollis may result from shortening of the muscle, with chin pointing away from the affected side and the head 3 tilted towards the mass. Treatment involves stretching, range of motion exercises and massage therapy. In the treatment of hyperkalemia, first give calcium gluconate as it will rapidly compete with potassium in the myocardium and antagonize its effect. Start sodium bicarbonate, insulin and glucose, and albuterol after the calcium gluconate. Sodium polystyrene (kayexylate) is an exchange resin given rectally. If all those don’t help, dialysis is indicated. The most common side effects of prostaglandin E1 are apnea, followed by hypotension. Scheuermann’s kyphosis is a condition that affects children just prior to the major growth spurt of puberty around 10-13 years. Its etiology is unclear. This is primarily a cosmetic problem due to the wedging of the anterior bodies of the thoracic vertebrae. In severe cases, spinal cord compression can occur, requiring surgical repair. The main treatment modality is use of a Milwaukee brace. A barium esophagogram will assess the patency of the esophagus in a patient with TE fistula that has been repaired and is now complicated by a stricture. A spinal epidural hematoma is a rare and dangerous cause of back pain. It may occur spontaneously, especially in patients with bleeding disorders or who are treated with anticoagulants. Osmotic fragility is abnormal in patients with hereditary spherocytosis or thalassemia, both of which are hemolytic diseases in which the Coombs test would be normal (unlike in autoimmune hemolytic anemia, where it is positive). G6PD is an x-linked disorder usually affecting males, except in populations with a high incidence of disease. Rotary subluxation of the first two cervical vertebrae needs to be differentiated from torticollis (wry neck). In torticollis, spasm of the sternocleidomastoid causes the chin of the patient to point to the opposite shoulder. In rotary subluxation, the chin points to the same side as the muscle spasm. Rotary subluxation may occur spontaneously or after a URI. If suspected, obtain a cervical CT scan to reveal the rotary subluxation of C1 around the dens. Hematuria, either microscopic or macroscopic, occurs in at least 90% of patients with renal colic. In younger children, pain associated with urolithiasis may not present with the excruciating pain of stone passage seen in adults. Patients may present with abdominal pain, flank pain, and or pain referred to the scrotum. AVM beeding or rupture can present with sudden onset of severe headache, vomiting, nuchal rigidity, hemiparesis, focal seizures or sudden arrest. 4 Sever’s Disease is a self-limiting apophysitis of the calcaneus in males 6-10 years old. It is thought to be due to overuse and injury of the calcaneus at the Achilles tendon insertion. X-rays may be normal or show increased fragmentation of the apophysis. Treatment consists of limitation of activities, heel cord stretching excercises and oral analgesics. Arch supports, heel supports or elevation of the heel may be helpful. If you hear about a straw or pencil injury to the throat, think about a pharyngeal laceration resulting in a retropharyngeal emphysema. Patients are at risk for retropharyngeal infection with Group A Strep, other Gram positive and anaerobic bacteria. Therefore, prophylactic antibiotics (IV cephazolin) and emergent ENT consult are indicated. Dental pain transmitted along the fifth cranial nerve is a common source of ear pain. Oral analgesics are given for the pain of an erupting tooth. Cellulitis: infection of connective tissue in subcutaneous space; epidermis spared; erythema, edema, warmth, and tenderness with a gradual, tapered edge; caused by staph or strep Erysipelas: infection of the epidermis, with abrupt, well-demarcated edges; involved skin has an orange peel appearance and is intensely red, warm, and very painful—can have rapid spread and blistering; patients are commonly febrile and ill appearing. Caused by Group A Streptococcus; in neonates, can be due to GBS; Tx: PCN + Clindamycin Patients with simple abscesses and no surrounding cellulitis do not require ABX, just an I & D. Perianal Cellulitis presents with rectal pain with sitting or defecation and has intense edema and erythema of perirectal tissues—looks like erysipelas but child is wellappearing—almost always due to Group A Strep. Infections of earlobe are usually due to staph and are treated with local care and antistaph oral abx Infections of cartilage from piercing are due to Pseudomonas, staph, or strep, and are treated more aggressively with Cefepime, piperacillin/tazobactam, or ceftaxidime Varicella is the most associated factor with necrotizing fasciitis in children because it increases the risk for invasive Group A Strep infection (NSAID’s increase the risk of invasive Group A strep disease as well). Necrotizing fasciitis: risk factors in children are malnutrition, neoplasia, recent surgery, omphalitis, breast abscesses, and balanitis associated with circs; symptoms begin with pain followed by induration, edema, and erythema within 1-2 days. Pain extends beyond the area of suspected inflammation—signs of necrosis such as purple skin, ecchymosis, and blisters are seen later. Paresthesia or anesthesia is an ominous sign of underlying 5 necrosis; Tissue crepitance is a specific indicator; may also have toxic appearance, thrombocytopenia, generalized rash; Dx: tissue biopsy; Tx: prompt surgical intervention Superficial skin infections—due to staph or strep—tx with Keflex or mupirocin; Only use Bactrim if you’re sure it’s staph (bactrim doesn’t work against strep) Eczema herpeticum is treated with IV acyclovir Folliculitis is due to staph—tx with topical antiseptics (chlorhexidine, hexachlorophene, or clindamycin) Hot tube folliculitis is due to pseudomonas—a begin, self-limited condition that resolves in 1-2 weeks, may also treat with oral quinolone Erythema Multiforme (EM) and Stevens-Johnson syndrome (SJS) are hypersensitivity syndromes caused by infections, drugs, vaccinations, malignancy, and connective tissue disorders. Erythema Multiforme (EM) consists of “target” skin lesions and may have involvement of one mucous membrane, usually the oral mucosa; EM is often preceded by a HSV infection of the face, may have prodromal symptoms; typically, crops of lesions develop over a few days in the acral regions, especially the palms and dorsa of the hands, wrists, feet, and extensor surfaces of elbows and knees; may manifest Koebner’s phenomenon (target lesions appearing within areas of cutaneous trauma from scratching). Resolves in 1-2 weeks but may last 4 weeks.; Frequently misdiagnosed as urticaria—but urticaria involves transient and migratory lesions with a clear central zone instead of the dusky, hemorrhagic center of EM lesions. In addition, urticarial lesions will respond to Epi and EM lesions will not. Tx: withdrawal of suspected drug cause, tx with Benadryl/maalox Stevens-Johnson Syndrome (SJS): diagnosis requires that at least 2 mucous membranes are affected in addition to the “target” skin lesions; ophthalmologic consult is required for ocular mucosa involvement; requires hospitalization in PICU or burn unit, IV fluid and electrolyte replacement and meticulous skin care; SJS is usually preceded by a prodromal viral type syndrome for 1-2 weeks. Toxicity and generalized lymphadenopathy are common, hepatosplenomegaly occasionally occur. After 1-14 days, the rash starts suddenly and occurs in face, trunk, and limbs. Mucous membranes of the oral, conjunctival, vulvovaginal, rectal, and urethral areas may be involved. Epidermis may separate from the basal layer as a result of minor friction (Nikolsky’s sign) Bacterial tracheitis is a life-threatening complication of croup The most common cause of stridor in infants is laryngomalacia; presents at birth or within first 6 weeks; infants have high pitched inspiratory stridor that increases with 6 crying and when supine, stridor is relieved when prone and calm; usually resolves on its own by 2 years of age. Vocal cord paralysis: 2nd most common cause of neonatal stridor—diagnosed within the first 12 hours of life with weak or absent cry Disorders causing supraglottic obstruction cause inspiratory stridor (epiglottitis) Disorders causing glottic/tracheal obstruction cause biphasic stridor (croup and tracheitis) Expiratory stridor is usually due to intrathoracic obstruction (FB aspiration); stridor that changes its pattern and timing may be due to an obstruction that is migrating (FB). Congenital disorders (tracheomalacia and laryngomalacia) present in the neonatal period; FB Aspiration peaks at 2-3 years of age; Croup is usually under 3 years of age; Retropharyngeal abscesses are most common under 4 years of age since retropharyngeal nodes disappear by 5 years of age. Epiglottitis Radiologic findings: epiglottic width to 3rd cervical width > 0.5 Croup (Laryngotracheobronchitis): most often from 6 mo-3yrs old; males 2:1, most commonly due to parainfluenza type 1; late fall-early winter; cyanosis is a late ominous sign; If stridor at rest give racemic epi. (Dose = 0.25 to 1 cc of a 2.25% solution in 3 cc of NS given via Neb); Observe at least 3 hrs post administration of racemic epi—if any problems or need for redosing, patient should be admitted.; Give Dexamethasone 0.6 mg/kg IM, IV, or po as well; Try heliox in order to prevent need for intubation—if ETT needed, use one at least 1 mm smaller than predicted. Epiglottitis has an abrupt, explosive onset of symptoms that may progress rapidly to respiratory failure; child is toxic appearing, tripods, drooling, mouth open, chin up, leaning forward, marked retractions; lateral neck x-ray reveals: swollen epiglottis (“thumbprint sign”), thickened aryepiglottic folds, obliteration of the vallecula, and dilation of the hypopharynx; Tx with ceftriaxone to cover H flu; prophylax with Rifampin for close contacts under 4 years of age. Bacterial Tracheitis (Membranous laryngotracheobronchitis; Pseudomembranous Croup): It is caused by a bacterial infection of the subglottic area that complicates patients with croup. Average age is 3 years; Has copious purulent secretions and pseudomembrane formation in the airway; primary organism is S aureus; usually starts as a URI for 1-2 weeks followed by a croup like illness for 1-2 days, followed by a rapid deterioration over several hours—at that point, the child will clinically look like a child with epiglottitis (toxic, febrile, etc.) but the history of the illness progression is different from the more rapid Epiglottitis story above. May see pseudomembrane within the tracheal lumen on X-ray (shaggy); Definitive diagnosis is from laryngotracheobronchoscopy showing purulent tracheal secretions. Tx: emergent intubation (hopefully in OR) using a ETT 1.0 mm smaller than expected; Ceftriaxone + Clindamycin; Use Chloramphenicol if PCN or CFTX allergic. 7 Retropharyngeal Abscess: Peak in 6-12 months of age group; usually caused by Group A Strep and S. aureus ; may have toxic appearance, fever, neck pain, dysphagia, torticollis, “hot potato” voice or voice sounding like a duck quack “cri du canard”; Positive tracheal rock sign (pain elicited when moving the larynx and trachea from side to side gently); may have meningismus, from irritation of paravertebral ligaments; May see widened prevertebral space on extended lateral neck x-ray. CT of neck is imaging modality of choice. TX: CFTX + Clindamycin Measles (Rubeola, First Disease): includes a prodrome of fever, cough, coryza, conjunctivitis, and Koplik’s spots; child appears ill; caused by RNA virus, paramyxovirus; exanthem begins at the hairline and spreads downward to become an intensely erythematous and at times purpuric rash. Rash fades by day 10; Severe pneumonia and encephalitis are primary causes of death; Using Vitamin A doses on 2 consecutive days decreases mortality. Post exposure prophylaxis includes the measles vaccine if given within 72 hours or IgG, which can be given up to 6 days following exposure in infants or the immune compromised. Leukocytosis common Rubella (German Measles, Third Disease): A RNA virus, Rubivirus, causing a maculopapular rash and enlargement of the occipitocervical lymph nodes; Forschheimer spots on the soft palate may be present; Rash occurs 1-5 days after onset of symptoms and is a faint rose-pink, macular or popular eruption that starts on the face and spreads downward; Eruption is resolved by the 3rd day (“3 day measles”) and the child is afebrile and appears well—in contrast to measles; monoarticular arthritis or arthralgia may be present. Leukopenia common. In first trimester may cause congenital infection, “blueberry muffin” spots, sensorineural hearing loss, heart defects, glaucoma, cataracts, thrombocytopenia; No treatment Roseola Infantum (Exanthem Subitum, Sixth Disease): Occurs in infants 6mo-3years with peak at 6-7 months; 2-3 days of high fever in well-appearing infant followed by resolution of fever and pink morbilliform rash appears for a few days (caused by HHV-6, a DNA virus); a seizure with the onset of fever is noted in 25-36% of cases; Nagayama’s spots may appear on the uvula or soft palate. No treatment Erythema Infectiosum (Fifth Disease); Parvovirus B19; slapped check appearance of rash on the face; most common in school aged children; rash may wax/wane for 4 months; Purpuric gloves and socks syndrome may occur; symmetric arthritis in joints may occur; May cause aplastic crisis in children with hereditary hemolytic anemias; No Treatment Atopic dermatitis—Infantile phase: up to age 2 years; eruption begins on cheeks, forehead, scalp, and lateral aspects of extensor surfaces of the legs (symmetric), spares the tip of the nose and the perioral and periorbital regions Atopic dermatitis—Childhood phase: from age 2 years to puberty; Eruption in flexural areas (mostly antecubital and popliteal fossae), and wrists; may have nummular (coinshaped) patches. 8 Children with Atopic dermatitis (AD) are at risk of HSV superinfection called eczema herpeticum. Also at risk for bacterial superinfection (impetigo) Treatment of AD involves topical steroids: Low potency: Hydrocortisone 1% or 2.5% ointment (BID-QID) Medium potency: Hydrocortisone valerate 0.2% ointment (QD-QID) High potency: Mometasone 0.1% ointment (QD) Newest form of treatment for AD is topical immunomodulator agents (Tacrolimus ointment in children over 2 years of age); side effects are stinging, burning, and erythema on application; does not cause skin atrophy so may be used for long periods on the face and intertriginous areas In cases where diaper dermatitis has been present for 3 or more days, there is always a candidal superinfection present and should be treated with nystatin ointment For seborrheic dermatitis (yellow greasy scaly, crusting eruption on the scalp, face, eyebrows, postauricular areas, and intertriginous folds; treatment is oatmeal baths and tar shampoo (don’t use shampoos with salicylic acid in children because they may be irritating and cause absorption problems of salicylism); may use ketoconazole; adolescents can use selenium sulfide shampoo Allergic contact dermatitis (i.e. nickel dermatitis, poison ivy, rubber) is a Type IV hypersensitivity reaction; see Kobner’s phenomenon in poison ivy—linear vesicular pattern; treatment is oatmeal baths, calamine lotion, antihistamines and topical and possibly oral steroids. The hallmark symptom of scabies is intense pruitis; Failure to find mites on microscopic examination does not rule out scabies; most common complication is secondary bacterial infection with staph aureus; Treat with 5% permethrin (Elimite) cream—may use in neonates, pregnant patients, and those who are breast feeding; Apply Elimite to entire body including face and scalp and wash off in 12 hours. Repeat treatment in 1 week; In the past, 1% gamma benzene hexachloride (lindane, Kwell) lotion was used but it is absorbed and concentrated in the CNS causing seizures and death. All family members and close contacts should be treated. Normal laundering or dry cleaning cleans clothing; all other fomites should be sealed in plastic bags for 1 week; For crusted scabies, crusts must first be removed before Elimite applied, otherwise treatment will fail. In these cases, may use Oral Ivermectin. Empirical treatment after a tick bite is not recommended; Lyme Disease is caused by the spirochete Borrelia burgdorferi from the deer tick (Ixodes dammini or Ixodes scapularis); It takes more than 24 hours for transmission to occur; The pathognomonic skin manifestation is Erythema Migrans (EM), Lyme arthritis is often monoarticular mostly involving the knee; Treat with Amox, Azithromycin, or doxycycline, or cefuroxime. 9 Rocky Mountain Spotted Fever occurs in many geographic areas and must be considered in a child with a tick exposure who presents with fever, headache, myalgias, and rash; It is caused by the obligate intracellular bacteria Rickettsia rickettsii; rash occurs 1-4 days after the onset of symptoms and start in ankles and feet and spreads to wrists and hands and then centripetally to head and trunk. Rash starts macular and eventually becomes petechial; Treatment: Doxycycline; In pregnant patients, give chloramphenicol but if given close to delivery will cause “Gray baby Syndrome”. Head lice are uncommon in African Americans because they have oval-shaped hair shafts that are harder for lice to grasp. The nits fluoresce a pale blue color under a Woods Lamp; Treatment is Permethrin lotion to the scalp after showering—leave on for 10 minutes then wash off; Repeat in 1 week; Use warm damp towels soaked in white vinegar which loosens nits from hair prior to mechanical removal with a fine-toothed comb; Seal fomites in plastic bags for 2 weeks. For body lice, treat from head to toe with 5% permethrin cream for 12 hours, wash off, then repeat in 1 week. Treat pubic lice like head lice. For eyelash lice, use Vaseline ointment 3-5 times/day Scarlet fever is treated with PCN to prevent local suppurative complications and the development of ARF Tinea capitis is the most common cause of hair loss in children Erythromycin should no longer be used for Group A strep due to resistance rates that approach 50% A typical presentation of Staphylococcal Toxic Shock Syndrome involves a menstruating female who presents with a high fever, generalized erythroderma and hypotension. Abdominal pain, vomiting, and diarrhea precede the hypotensive state In pityriasis versicolor, KOH prep will reveal “spaghetti and meatballs” of budding yeast and hyphae. Kawasaki Disease: “ELF ROP” Eye findings: painless bulbar conjunctival injection, non-purulent, with sparing of limbus Lymph Nodes: swelling of cervical lymph nodes > 1.5cm, child complains of pain and may have torticollis Fever: FUO for > 5 days; high spiking and remitting Rash Oral: dryness, redness, fissuring, peeling, cracking, and bleeding of lips, or strawberry tongue, diffuse oral mucosa erythema Peripheral extremity: reddening of palms and soles, indurative edema, desquamation and fissuring at tips of fingers, palms and soles Thrombocytosis from 500,000 to > 1,000,000 occurs during week 2 ECG changes: prolonged PR interval or QT interval and ST and T wave changes 10 Tx: 2 g/kg of IVIG over 12 hours and ASA 100mg/kg QID, then after defervescence, ASA 4mg/kg QID; ASA d/c’d if no coronary artery abnormalities seen by 6 weeks after onset. Suspect diagnosis in a child with FUO > 5 days without a source. Glomerulonephritis typically is manifested by edema, hypertension, and hematuria, often accompanied by acute renal failure. In this case, the elevated creatinine and potassium concentrations are consistent with a diagnosis of acute renal failure. Immediate management should focus on treating the severe hyperkalemia. Hyperkalemia, which is classified as mild (5.5 to 6.0 mEq/L [5.5 to 6.0 mmol/L]), moderate (6.1 to 7.0 mEq/L [6.1 to 7.0 mmol/L]), or severe (>7.0 mEq/L [7.0 mmol/L]), is a medical emergency that requires immediate treatment with myocardial membranestabilizing medications such as intravenous calcium to prevent life-threatening arrhythmias. Subsequent management of hyperkalemia includes shifting the potassium to the intracellular compartment through the use of sodium bicarbonate, glucose, insulin, and albuterol. Sodium polystyrene sulfonate is used to reduce total body potassium concentrations. Its onset of action is within 1 to 2 hours of administration. Although a child's blood pressure may be at the 95th percentile for age and may require further management, this problem is not as emergent as hyperkalemia. Penicillin is the drug of choice for pharyngitis due to group A Streptococcus (GAS), the leading cause of glomerulonephritis, but treatment with antibiotics has no effect on the subsequent development of renal disease. Treatment is not warranted in the absence of symptoms of GAS pharyngitis. Although the differential diagnosis for febrile children who have rash and hypotension is broad, the multiorgan involvement described for the patient in the vignette strongly suggests toxic shock syndrome (TSS). This condition achieved notoriety with reports of its association with tampon use in menstruating females (“menstrual TSS”), but it also is associated with nonmenstruating situations such as nasal packing, wound infections, sinusitis, primary bacteremia, burns, pneumonia, and osteomyelitis (“nonmenstrual TSS”). TSS is an acute, life-threatening illness caused by the exotoxin TSST-1 that is produced by phage group 1 Staphylococcus aureus or streptococcal pyrogenic exotoxins A, B, C, and F produced by Streptococcus pyogenes. The illness is characterized by high fever, a diffuse erythematous rash (sunburn appearance or scarlatiniform), desquamation of skin, hypotension, and involvement of three or more organ systems. Symptoms often include alteration of consciousness, oliguria, shock, and disseminated intravascular coagulation. Among the complications are acute respiratory distress syndrome, myocardial dysfunction, and renal failure. Recovery occurs in 7 to 10 days in uncomplicated cases. Blood cultures often are negative; throat cultures and nasopharyngeal cultures may reveal the presence of S aureus. Research suggests that TSST-1 toxins are produced selectively in an environment of neutral pH, high Pco2, and aerobic Po2 (conditions present in the vagina with tampon use during menstruation). A concomitant low serum magnesium concentration may be an 11 additional risk factor. The toxins in TSS interact with major histocompatibility class II proteins and activate T cells, which leads to polyclonal activation and a massive release of the cytokines tumor necrosis factor-alpha and interleukin-6. These substances are responsible for multiorgan involvement and shock. TSS is a clinical diagnosis based on criteria established by the Centers for Disease Control and Prevention (Tables 1 and 2). Table 1: Criteria for Staphylococcal Toxic Shock Syndrome Fever of ( ≥102°F) ≥38.9°C Presence of diffuse macular erythroderma ("sunburn" appearance) Desquamation 1 to 2 wk after onset of illness, particularly of the palms and soles Hypotension, defined as a systolic blood pressure of ≤90 mm Hg for adults and <5th percentile for children younger than 16 years; an orthostatic decrease in diastolic blood pressure of ≥15 mm Hg with a position change from lying to sitting; orthostatic syncope; or orthostatic dizziness Involvement of three or more of the following organ systems: Gastrointestinal: history of vomiting or diarrhea at the onset of illness Muscular: elevated creatine phosphokinase level or severe myalgia Mucous membrane: nonpurulent conjunctivitis, oropharyngeal hyperemia, or vaginal hyperemia or discharge Renal: abnormal results of renal function tests or urinalysis Hepatic: elevated serum transaminase and bilirubin levels Hematologic: thrombocytopenia Central nervous system: disorientation or alteration in consciousness without focal neurologic signs and in the absence of hypotension or fever In addition, normal results of the following tests, if performed: Blood, throat, cerebrospinal fluid cultures (blood culture may be positive for Staphylococcus aureus); antibody tests for Rocky Mountain spotted fever, ehrlichiosis, leptospirosis, and rubella. Toxic shock syndrome is probable when at least four of the five criteria are fulfilled. Modified from American Academy of Pediatrics. Staphylococcal toxic shock syndrome. In: Peter G, ed. 1997 Red Book: Report of the Committee on Infectious Diseases. 24th ed. Elk Grove Village, Ill: American Academy of Pediatrics; 1997:481. 12 Table 2: Proposed Case Definition for the Streptococcal Toxic Shock Syndrome Modified from the Centers for Disease Control and Prevention. The Working Group on Severe Streptococcal Infection. Defining the group A streptococcal toxic shock syndrome: rationale and consensus definition. JAMA. 1993;269:390–391. Table from American Academy of Pediatrics. Group a streptococcal infections. In: Peter G, ed. 1997 Red Book: Report of the Committee on Infectious Diseases. 24th ed. Elk Grove Village, Ill: American Academy of Pediatrics; 1997:481. It should be noted that 40% to 50% of nonmenstrual TSS and 5% to 10% of menstrual TSS isolates do not produce TSST-1. Therefore, a role for other exo- or endotoxins has been proposed. The management of TSS consists of aggressive resuscitation with fluids and appropriate inotropes. Antibiotic therapy consists of a beta-lactamase–resistant antistaphylococcal antibiotic (or vancomycin if methicillin-resistant S aureus is common in the community) plus a protein synthesis-inhibiting antimicrobial drug such as clindamycin. Adjunctive treatment with systemic corticosteroids and intravenous immunoglobulin may be helpful in severe cases. 13 Staphylococcal scalded skin syndrome is characterized by a diffuse, tender, erythematous rash, a positive Nikolsky sign, and hemodynamic stability. Kawasaki syndrome (KS) is an acute generalized vasculitis that generally is associated with a normal or elevated platelet count, normal renal function, and hemodynamic stability. The clinical picture of Rocky Mountain spotted fever is similar to TSS, but the rash has a characteristic distribution. The rash is petechial, begins on the ankles and wrists, and eventually spreads to involve the entire body (centripetal spread). The rash of Stevens-Johnson syndrome is characterized by vesiculobullous skin lesions and involvement of two or more mucous membranes. The rash described for the infant in the vignette is consistent with diaper dermatitis (DD), the most common dermatologic condition in infants. Also known as irritant contact dermatitis, DD is a general term used to describe inflammation of the skin within the diaper area. The typical features of DD include an erythematous rash over the convex skin surfaces within the diaper area that spares the intertriginous areas. Moisture, friction, elevated pH, and digestive stool enzymes are believed to play key roles in the development of DD. Occlusion of the skin under a diaper allows these factors to cause overhydration, maceration, and subsequent irritation and inflammation of the exposed skin. The inflamed skin is more susceptible to secondary infection with yeast, bacteria, or less commonly, viruses. Management of primary DD is directed at eliminating or diminishing the causative factors. Because the use of diapers is the initiating factor, keeping the infant or child out of diapers as much as possible should be part of the treatment plan, although this is obviously not practical for most infants most of the time. Increasing the frequency of diaper changes can decrease the exposure of skin to moisture and stool. In addition, the use of ultra-absorbent disposable diapers, which contain polymers in their cores to pull liquid away from the skin, significantly reduces the incidence and severity of DD. Those diapers that have “breathable” outer surfaces also allow water vapor to leave the diaper and have been shown in several studies to decrease the incidence of both DD and Candida infections. Cloth and less absorbent disposable diapers hold the moisture and irritants in contact with the skin, increasing the risk of DD. Barrier creams and ointments that contain such active ingredients as zinc oxide, dimethicone, or petrolatum should be applied to shield the skin from irritants whenever the diaper is changed. The cream should be applied to dry skin for optimal results. For most cases of primary DD, these measures alone result in resolution of the rash. For more severe or recalcitrant cases, low-potency topical steroids can be used for a short course; mid- and high-potency steroids should be avoided due to the risks of skin atrophy, tachyphylaxis, and systemic absorption with secondary adrenal suppression. Infection with C albicans commonly accompanies DD. Characteristics that should alert the physician to this possibility include involvement of the skin creases, satellite lesions, and DD that fails to respond to appropriate conservative management. Recent or frequent antibiotic exposure also increases the likelihood of yeast infection. Topical antifungal cream or ointment should be added to the treatment regimen in these cases. There is no evidence that oral antifungal therapy offers any advantage over topical treatment. 14 Bacterial skin infection, most commonly caused by Staphylococcus aureus or group A Streptococcus, should be suspected when bullae, skin erosion, or crusting is present. Topical or systemic antibiotic therapy should be added in these cases. The facial rash in the child above, who has atopic dermatitis (AD), represents secondary herpes simplex infection. Patients who have AD are prone to recurrent viral infections, perhaps because of local defects in T-cell function. Eczema herpeticum, also known as Kaposi varicelliform eruption, is a serious risk in patients who have widespread AD and may be easily misdiagnosed as bacterial superinfection. After an incubation period of 5 to 12 days, multiple pruritic vesiculopustular, disseminated lesions and painful “punched-out” superficial ulcerations appear that fail to respond to oral antibiotics. Before treatment with acyclovir is initiated, herpes infection should be documented via culture of a skin scraping or direct fluorescent antibody testing. Topical corticosteroids (clobetasol) and topical calcineurin inhibitors (TCIs) such as tacrolimus are the major pharmacologic treatments used to address acute flares and overall disease management of AD. Mild-to-moderate exacerbations are characterized by itching, erythema, excoriations, papules, and lichenification. Severe flares present with “weeping” of excoriated lesions and extensive lichenification, as described for the child in the vignette. 15 Topical mupirocin and parenteral clindamycin are useful in the management of bacterial superinfection of AD, particularly in an era when community-associated methicillinresistant Staphylococcus aureus has become frequent. Clues to secondary bacterial infection include honey-colored crusting, folliculitis, pyoderma, and cellulitis (Fig. 2). Recurrent furuncles should lead to concern for deficiency in humoral immunity such as hyper-immunoglobulin E syndrome. Figure 2 Excellent skin care is the mainstay of AD management. Emollients and moisturizers that are free of dyes and fragrances should be applied at least twice daily after any topical pharmacologic therapy. Avoidance of known triggers and judicious use of antipruritic agents such as hydroxyzine and diphenhydramine may be useful to improve sleep in patients who have flare-ups. The timing and frequency of bathing is controversial. Bathing promotes skin hydration, cleansing of the skin, and penetration of topical agents. The potential drawbacks are drying of the skin and disruption of the stratum corneum barrier. This can be minimized by the “soak and seal” strategy, which involves bathing for several minutes in lukewarm water, patting excess moisture from the skin, and promptly applying liberal quantities of emollients before the skin dries completely. Topical steroids may be used once or twice daily for treatment of acute AD flare. Some clinicians begin with a high- to mid-potency agent to induce a remission, followed by a rapid taper of preparation potency as AD improves. TCIs are second-line agents for shortterm treatment and noncontinuous chronic treatment of moderate-to-severe AD in immunocompetent patients 2 years of age and older who have failed to respond adequately to first-line agents. Such therapy is designed to limit long-term exposure to corticosteroids. 16 A complete blood count (CBC), including platelet count, should be obtained for all children presenting with diffuse purpuric rashes. Other laboratory studies that may be useful, depending on the patient's presentation, include a prothrombin time (PT), partial thromboplastin time (PTT), fibrinogen, fibrin degradation products, blood gas analysis for acidemia, C–reactive protein (CRP), lactate, electrolytes, blood urea nitrogen, creatinine, lactate dehydrogenase, uric acid, and urinalysis. CRP values have been shown to be elevated in patients who have meningococcemia, including those in whom this diagnosis was not suspected at initial evaluation. The number of studies often can be minimized in well-appearing children, such as the girl in the vignette. If such children have normal vital signs, they can be reassessed and observed closely while results are pending, and antibiotic administration can be held until the results become available. For this child, a CBC and urinalysis are indicated, as are coagulation studies (PT and PTT) because her rash is widespread. Corticosteroids should not be administered until the underlying cause becomes more apparent because of potential complications. For example, if thrombocytopenia is due to leukemia or another malignancy, corticosteroids may interfere with appropriate diagnosis and initial treatment. Fibrinogen and fibrin degradation products help in the diagnosis of disseminated intravascular coagulation, but this condition is unlikely in a child who looks so well. The nature and distribution of this child's rash in addition to her well appearance suggest a diagnosis of infantile HSP (acute hemorrhagic edema of infancy). In infants, HSP often presents with facial purpura and edema but relative sparing of other sites (eg, kidney and gastrointestinal sites). For this patient, a normal platelet count, PT, and PTT would be expected and reassuring. In addition, if a CRP were obtained, it would be expected to yield normal or minimally elevated results. Although renal involvement is less common in infants who have HSP, it still should be excluded. Treatment involves symptomatic care and good follow–up. The rash beginning with a round papulosquamous solitary lesion (herald patch) on the arm and progressing to a secondary eruption of similar but smaller lesions on the face and neck described for the boy in the vignette is characteristic of the inverse variant of pityriasis rosea (PR). PR is a common, generally benign, inflammatory skin disorder that typically is seen in adolescents but can occur in young children and adults. The name comes from the Greek word pityriasis (meaning scaly) and the Latin word rosea (meaning pink). PR is most common in the spring, but it can be seen in any season. Usually PR occurs in previously asymptomatic patients, although a mild prodrome of low-grade fever and malaise is present in about 5% of cases. The prodromal illness, seasonal variation, and clustering of cases has led to the impression that PR has a viral etiology. Human herpesviruses 6 and 7 have been implicated as causative, but agreement is not yet definitive. A PR-like rash may result from the use of various medications, including metronidazole, barbiturates, beta blockers, and clonidine. In 50% to 85% of cases, the rash of PR begins with a single oval papulosquamous lesion called a herald patch (because it heralds the beginning of the illness). The herald patch usually appears on the trunk or lower abdomen, but it may occur on the extremities (as in the boy in the vignette) or elsewhere on the body. Multiple herald patches are seen in about 5% of 17 patients. About 1 to 3 weeks after the appearance of the herald patch, a secondary eruption of smaller oval papulosquamous lesions appears in crops over 1 to 2 weeks. These lesions usually are present on the child's back and occur in a “Christmas tree” distribution, such that the long axis of the oval lesion lies along the skin cleavage lines (Langer's lines). As with the primary lesion, the scales of the secondary lesions characteristically have the free edges pointed inward toward the center of the lesion. The rash of PR typically lasts 6 to 8 weeks and resolves spontaneously. Although the classic presentation of PR involves a rash on the trunk, sparing the face and hands, there are important variations to this distribution. About 25% of cases of PR are atypical, and such cases are more common in children. The boy in the vignette has “inverse” PR, the most common variant, in which areas typically spared in the classic presentation (face, arms, axillae, inguinal region) are involved. Thus, the skin distribution is opposite, or inverse, to the classic presentation. The presentation of PR in African Americans often differs substantially from that in light-skinned children, consisting primarily of papules (follicular PR) and few, if any, macules, as previously described. The diagnosis of PR is based on the clinical symptoms. Because no clear etiologic agent has been identified, management is aimed at symptomatic relief of skin dryness and pruritus. The use of moisturizers and oral antihistamines often is beneficial, and a mild steroid cream (eg, 1% hydrocortisone) may be applied topically to the lesions. More severe cases may respond to a course of oral steroid treatment. Some reports suggest improvement of PR with ultraviolet B phototherapy or natural ultraviolet light. Erythema multiforme is a hypersensitivity reaction to medications or infectious agents. The associated rash usually has the characteristic “target lesions” in addition to erythematous macules and papules. Scabies is an intensely pruritic rash consisting of erythematous papules and vesicles usually appearing as burrows in the web spaces of the fingers or feet or along the waistline or axilla. In infants, the rash of scabies may present as an eczematous eruption but usually is widespread and involves primarily the trunk. The rash of secondary syphilis consists of reddish-brown papulosquamous lesions on the palms of the hands and the soles of the feet. Although secondary syphilis always should be considered in an adolescent who has PR because the lesions are similar in appearance, the distribution of the rash, the presence of pruritus, and the age of the child in the vignette makes syphilis unlikely. The herald patch of PR often is confused for tinea corporis because both diseases present with oval or circular papulosquamous lesions. However, the rash of tinea typically has elevated borders, unlike the lesions seen in PR. Tinea, like other fungal infections, may cause an inflammatory reaction distant from the site of the initial infection. This so-called dermatophytid (or “id”) reaction is generally vesicular, papular, or urticarial, which is not consistent with the rash described in the vignette. 18 Tinea incognito, a dermatophyte infection that has been modified and even exacerbated by the long-term use of topical corticosteroids. The immunosuppressive effect of topical corticosteroids that can alleviate the initial erythema and pruritus likely is responsible for the atypical transformation and spread of the dermatophyte infection. The characteristic circular, well-defined, scaling edge of tinea corporis can assume a variety of appearances: psoriasislike, eczemalike, or licheniform, with follicular, pustular, or papular characteristics. In general, most infectious dermatologic conditions are aggravated by topical corticosteroid use. Varicella zoster is an unusual condition in a young immunocompetent child. Pain precedes the appearance of the dermatomal rash, which starts as erythematous papules and progresses to vesicles and confluent blisters, eventually crusting over. 19 In contrast, topical corticosteroids are common therapies for several dermatologic conditions. Inflammatory-mediated rashes and conditions that feature a significant inflammatory component benefit from topical corticosteroid use. Such conditions tend to be noninfectious and include allergic contact dermatitis, atopic dermatitis/eczema, psoriasis, and seborrheic dermatitis. Allergic contact dermatitis (eg, exposure to poison ivy) is a type IV hypersensitivity reaction that is characterized by erythema and edema, usually about 48 hours after exposure to the offending agent. The development of exudative vesicular or bullous lesions may follow. The hallmark of atopic dermatitis is unremitting pruritus, which leads to the excoriation, lichenification, and crusting of lesions. Xerosis, scaling, and erythema are also common. Topical or oral steroid is particularly beneficial for type IV hypersensitivity reactions. Other dermatologic conditions that can improve with topical corticosteroid use but are somewhat less responsive are: discoid lupus erythematosus, pemphigus, vitiligo, pityriasis rosea, and granuloma annulare. The rash of erythema multiforme minor tends to be symmetrically distributed, is initially maculopapular, and eventually develops into the characteristic “target lesions.” Mild cases do not require any treatment. 20 The ill appearance and mucocutaneous rash described for the boy in the vignette are suggestive of Stevens-Johnson Syndrome (SJS) triggered by ibuprofen. SJS is a potentially life-threatening, acute, inflammatory, mucocutaneous disorder affecting the skin and at least two or more mucous membrane surfaces such as eyes, lips, or oral mucosa. Management of SJS includes immediate withdrawal of the offending agent, if known (ibuprofen for this boy), and supportive care. The illness should be managed like a “burn,” with aggressive fluid resuscitation, infection control measures, and nutrition support. SJS can be caused by chemical exposures or infections. Among the medications commonly implicated are sulfonamides, antiepileptic drugs such as phenytoin, and nonsteroidal anti-inflammatory drugs such as ibuprofen. The estimated mortality ranges from 5% to 15%. SJS belongs to same disease spectrum as toxic epidermal necrolysis (TEN). In these conditions, lateral pressure to erythematous areas can result in epidermal detachment (Nikolsky sign). Generally, mucous membrane involvement is preceded by a 21 few days of fever and influenza-like symptoms, followed by development of skin lesions. SJS may evolve to become TEN. The primary difference between the two is the extent of body surface involved: less than 10% for SJS and more than 30% for TEN. Lifethreatening complications (eg, sepsis and fluid loss) are related to sloughing of the skin and the resultant loss of the protective cutaneous barrier. There is no universally accepted clinical algorithm for diagnosis of SJS. Up to 85% of cases have conjunctival involvement that can range from hyperemia to pseudomembrane formation and frequently is associated with burning and pain. Photophobia, impaired alimentation, and painful micturition corresponding to involvement of mucous membranes also may be noted. Alternative causes of the symptoms should be excluded, particularly infections that have similar presentations, such as group A streptococcal or staphylococcal toxic shock syndrome, leptospirosis, measles, Kawasaki disease, and staphylococcal scalded skin syndrome. The primary differential diagnosis of SJS is erythema multiforme (EM) major, which formerly was considered to be a limited form of the same disease. More recent literature distinguishes EM major from SJS and places SJS and TEN in the same spectrum. The classic lesions of EM (both minor and major) are discrete, macular or papular, concentric erythematous rings (targetlike appearance) (Fig. 2). EM major involves at least one mucous membrane. Most cases of EM (60%) are associated with herpes simplex infection. Others have been associated with viral or mycoplasma infections. Lip involvement can make it difficult to distinguish from SJS. 22 23 Intertrigo in an infant has a wide differential diagnosis. Common causes are seborrheic dermatitis (SD), candidiasis, and atopic dermatitis. Topical steroids and antifungal agents are first-line agents that typically are used to treat SD and Candida infections, respectively. Atopic dermatitis characteristically spares the diaper area. Severe and recalcitrant intertriginous dermatitis may be a symptom of a more serious condition such as Langerhans cell histiocytosis (LCH), acrodermatitis enteropathica (AD), or underlying congenital or acquired immune deficiency. The rash in this infant below appears to be well-demarcated, with scaly macules, papules, and plaques and some purpuric areas. In addition, discrete reddish-brown papules, petechiae, and erosions may be seen in LCH. This presentation, in conjunction with hepatomegaly, is very suggestive of LCH. Infantile LCH (formerly called Letterer Siwe disease) is an aggressive form of multifocal disease that involves skin and internal organs such as the bone marrow, liver, spleen, and bones. Hepatosplenomegaly, anemia, and thrombocytopenia frequently are noted, making a complete blood count helpful for the infant in the vignette. Definitive diagnosis is established with a skin biopsy—see picture below: 24 A serum zinc assessment would assist in the diagnosis of AD. Zinc deficiency (<50 mcg/dL [7.7 mcmol/L]) usually is associated with periorificial involvement, chronic diarrhea, alopecia, irritability, and malnutrition. Bacterial (streptococcal) intertrigo characteristically causes well-demarcated, beefy red, macerated, moist lesions with scant bleeding and without satellite lesions. The infant usually experiences pain and discomfort during diaper changes. The rash often has a very distinct malodor. Conversely, satellite lesions are common with Candida intertrigo. These two organisms may coexist in diaper dermatitis. SD has a bimodal peak that presents between 1 and 6 months of age and during teenage years. The skin lesions typically are salmon-pink scaling patches on the face and scalp, external ear, and intertriginous body folds, areas that are rich in sebaceous glands. Pruritus is not a dominant feature, unlike with atopic dermatitis. The pathogenesis of SD is postulated to be the cutaneous fungus Malassezia furfur. Hence, topical agents such as 2% ketoconazole shampoo are effective. Other therapeutic agents that are helpful in severe cases include 1% to 2.5% hydrocortisone cream, 1% pimecrolimus, and 0.03% to 0.1% tacrolimus ointment. The natural course of both infantile and adolescent SD is disappearance with age. 25 The differential diagnosis of SD includes atopic dermatitis, candidiasis, LCH, AD, streptococcal intertrigo, congenital and acquired immune deficiencies, and psoriasis vulgaris. Childhood psoriasis typically has an onset between 6 and 18 months and is characterized by well-defined, scaly plaques. There is usually a positive family history. 26