Key Strategies for Managing
Neuropathic Pain
Copyright © 2005 Thomson Professional Postgraduate Services®. All rights reserved.
IASP Definition of Pain
“Pain is an unpleasant sensory
and emotional experience
associated with actual or potential
tissue damage or described in
terms of such damage.”
2
Acute vs Chronic Pain
Characteristic
3
Acute Pain
Chronic Pain
Cause
Generally known
Often unknown
Duration of pain
Short,
well-characterized
Persists after healing,
3 months
Treatment
approach
Resolution of
underlying cause,
usually self-limited
Underlying cause and pain
disorder; outcome is often
pain control, not cure
Domains of Chronic Pain
4
Quality of Life
• Physical functioning
• Ability to perform
activities of daily living
• Work
• Recreation
Psychological Morbidity
• Depression
• Anxiety, anger
• Sleep disturbances
• Loss of self-esteem
Social Consequences
• Marital/family
relations
• Intimacy/sexual activity
• Social isolation
Socioeconomic
Consequences
• Healthcare costs
• Disability
• Lost workdays
Nociceptive vs Neuropathic Pain
Nociceptive
Pain
Mixed Type
Caused by activity in
neural pathways in
response to potentially
tissue-damaging stimuli
Caused by a
combination of both
primary injury and
secondary effects
Neuropathic
Pain
Initiated or caused by
primary lesion or
dysfunction in the
nervous system
CRPS*
Postoperative
pain
Arthritis
Mechanical
low back pain
Sickle cell
crisis
Sports/exercise
injuries
5
*Complex regional pain syndrome
Postherpetic
neuralgia
Trigeminal
neuralgia
Neuropathic
low back pain
Central poststroke pain
Distal
polyneuropathy
(eg, diabetic, HIV)
Possible Descriptions
of Neuropathic Pain
• Sensations
–
–
–
–
–
–
–
–
–
–
6
numbness
tingling
burning
paresthetic
paroxysmal
lancinating
electriclike
raw skin
shooting
deep, dull, bonelike ache
• Signs/Symptoms
– allodynia: pain from a
stimulus that does not
normally evoke pain
• thermal
• mechanical
– hyperalgesia: exaggerated
response to a normally
painful stimulus
Physiology of Pain Perception
• Transduction
Injury
Brain
• Transmission
• Modulation
• Perception
• Interpretation
Descending
Pathway
• Behavior
Peripheral
Nerve
Dorsal
Root
Ganglion
Ascending
Pathways
C-Fiber
A-beta Fiber
A-delta Fiber
7
Dorsal
Horn
Spinal Cord
Adapted with permission from WebMD Scientific American® Medicine.
Pathophysiology of
Neuropathic Pain
•
•
•
•
•
•
•
Chemical excitation of nonnociceptors
Recruitment of nerves outside of site of injury
Excitotoxicity
Sodium channels
Ectopic discharge
Deafferentation
Central sensitization
– maintained by peripheral input
• Sympathetic involvement
• Antidromic neurogenic inflammation
8
Multiple Pathophysiologies May
Be Involved in Neuropathic Pain
• More than one mechanism of action likely involved
• Neuropathic pain may result from abnormal peripheral
nerve function and neural processing of impulses due
to abnormal neuronal receptor and mediator activity
• Combination of medications may be needed to
manage pain: topicals, anticonvulsants, tricyclic
antidepressants, serotonin-norepinephrine reuptake
inhibitors, and opioids
• In the future, ability to determine the relationship
between the pathophysiology and symptoms/signs
may help target therapy
9
Percentages of Herpes Zoster
Patients With Persistent Pain
80
70
1 month
1 year
% of patients
60
50
40
30
20
10
0
0
19
29
39
49
59
69
70
Age (y)
10
Adapted from DeMorgas JM, Kierland RR. Arch Dermatol. 1957;75:193-196.
What Are the Goals of
Clinical Assessment?
•
•
•
•
•
•
•
•
11
Achieve diagnosis of pain
Identify underlying causes of neuropathy
Identify comorbid conditions
Evaluate psychosocial factors
Evaluate functional status (activity levels)
Set goals
Develop targeted treatment plan
Determine when to refer to specialist or
multidisciplinary team (pain clinic)
Assessing the Patient With Pain
•
•
•
•
•
•
•
Onset and duration
Location/distribution
Quality
Intensity
Aggravating/relieving factors
Associated features or secondary signs/symptoms
Associated factors
– mood/emotional distress
– functional activities
• Treatment response
12
Pain Treatment Continuum
Most
invasive
Least
invasive
Continuum not related to efficacy
Psychological/physical approaches
Topical medications
Systemic medications*
Interventional techniques*
13
*Consider referral if previous treatments were unsuccessful.
Nonpharmacologic Options
•
•
•
•
Biofeedback
Relaxation therapy
Physical and occupational therapy
Cognitive/behavioral strategies
– meditation; guided imagery
• Acupuncture
• Transcutaneous electrical nerve stimulation
14
Pharmacologic Treatment
Options
• Classes of agents with efficacy demonstrated
in multiple, randomized, controlled trials for
neuropathic pain
– topical analgesics (capsaicin, lidocaine patch 5%)
– anticonvulsants (gabapentin, lamotrigine,
pregabalin)
– antidepressants (nortriptyline, desipramine)
– opioids (oxycodone, tramadol)
• Consider safety and tolerability when initiating
treatment
15
FDA-Approved Treatments for
Neuropathic Pain
• Carbamazepine
– trigeminal neuralgia
• Duloxetine
– peripheral diabetic neuropathy
• Gabapentin
– postherpetic neuralgia
• Lidocaine Patch 5%
– postherpetic neuralgia
• Pregabalin*
– peripheral diabetic neuropathy
– postherpetic neuralgia
16
*Availability pending based upon controlled substance scheduling by the DEA.
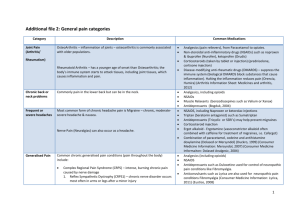
Pharmacologic Agents
Affect Pain Differently
BRAIN
CNS
PNS
Peripheral
Sensitization
17
Descending Modulation
Spinal
Cord
Dorsal
Horn
Local Anesthetics
Topical Analgesics
Anticonvulsants
Tricyclic Antidepressants
Opioids
Anticonvulsants
Opioids
Tricyclic/SNRI Antidepressants
Central Sensitization
Anticonvulsants
Opioids
NMDA-Receptor Antagonists
Tricyclic/SNRI Antidepressants
Topical vs Transdermal
Drug Delivery Systems
18
Topical
(lidocaine patch 5%)
Transdermal
(fentanyl patch)
Peripheral tissue activity
Applied directly over painful site
Insignificant serum levels
Systemic side effects unlikely
Systemic activity
Applied away from painful site
Serum levels necessary
Systemic side effects
Lidocaine Patch 5%
• Lidocaine 5% in pliable patch
• Up to 3 patches applied once daily directly over
painful site
– 12 h on, 12 h off (FDA-approved label)
– recently published data indicate 4 patches (18–24 h) safe
• Efficacy demonstrated in 3 randomized controlled trials on
postherpetic neuralgia
• Drug interactions and systemic side effects unlikely
– most common side effect: application-site sensitivity
• Clinically insignificant serum lidocaine levels
• Mechanical barrier decreases allodynia
19
Anticonvulsant Drugs for
Neuropathic Pain Disorders
• Postherpetic neuralgia
– gabapentin*
– pregabalin *
• Diabetic neuropathy
–
–
–
–
–
20
carbamazepine
phenytoin
gabapentin
lamotrigine
pregabalin *
*Approved by FDA for this use.
HIV = human immunodeficiency virus.
• HIV-associated neuropathy
– lamotrigine
• Trigeminal neuralgia
– carbamazepine*
– lamotrigine
– oxcarbazepine
• Central poststroke pain
– lamotrigine
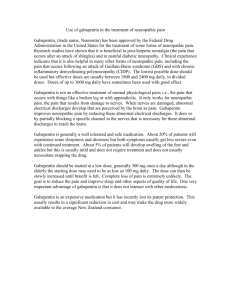
Gabapentin in Neuropathic
Pain Disorders
•
•
•
•
FDA approved for postherpetic neuralgia
Anticonvulsant: uncertain mechanism
Limited intestinal absorption
Usually well tolerated; serious adverse effects rare
– dizziness and sedation can occur
• No significant drug interactions
• Peak time: 2 to 3 h; elimination half-life: 5 to 7 h
• Usual dosage range for neuropathic pain up to
3,600 mg/d (tid–qid)*
21
*Not approved by FDA for this use.
Antidepressants in
Neuropathic Pain Disorders*
• Multiple mechanisms of action
• Randomized controlled trials and meta-analyses
demonstrate benefit of tricyclic antidepressants
(especially amitriptyline, nortriptyline, desipramine)
for postherpetic neuralgia and diabetic neuropathy
• Onset of analgesia variable
– analgesic effects independent of antidepressant activity
• Improvements in insomnia, anxiety, depression
• Desipramine and nortriptyline have fewer adverse
effects
22
*Not approved by FDA for this use.
Tricyclic Antidepressants:
Adverse Effects
• Commonly reported AEs
(generally anticholinergic):
–
–
–
–
–
–
–
–
–
23
blurred vision
cognitive changes
constipation
dry mouth
orthostatic hypotension
sedation
sexual dysfunction
tachycardia
urinary retention
AEs = adverse effects.
Fewest
AEs
• Desipramine
• Nortriptyline
• Imipramine
• Doxepin
• Amitriptyline
Most
AEs
Principles of Opioid Therapy
for Neuropathic Pain
• Opioids should be titrated for therapeutic efficacy
versus AEs
• Fixed-dose regimens generally preferred over prn regimens
• Document treatment plan and outcomes
• Consider use of opioid written care agreement
• Opioids can be effective in neuropathic pain
• Most opioid AEs controlled with appropriate specific
management (eg, prophylactic bowel regimen, use of
stimulants)
• Understand distinction between addiction, tolerance,
physical dependence, and pseudoaddiction
24
Distinguishing Dependence,
Tolerance, and Addiction
• Physical dependence: withdrawal syndrome arises
if drug discontinued, dose substantially reduced,
or antagonist administered
• Tolerance: greater amount of drug needed to
maintain therapeutic effect, or loss of effect over time
• Pseudoaddiction: behavior suggestive of addiction;
caused by undertreatment of pain
• Addiction (psychological dependence): psychiatric
disorder characterized by continued compulsive use
of substance despite harm
25
Interventional Treatments
for Neuropathic Pain
• Neural blockade
– sympathetic blocks for CRPS-I and II
(reflex sympathetic dystrophy and causalgia)
• Neurolytic techniques
– alcohol or phenol neurolysis
– pulse radio frequency
• Stimulatory techniques
– spinal cord stimulation
– peripheral nerve stimulation
• Medication pumps
26
CRPS = complex regional pain syndrome.
Summary of Advances in
Treatments for Neuropathic Pain*
• Botulinum toxin: low back pain
• Lidocaine patch 5%: low back pain, osteoarthritis,
diabetic and HIV-related neuropathy, with gabapentin
• CR oxycodone: diabetic neuropathy
• Gabapentin: HIV-related neuropathy, diabetic peripheral
neuropathy, others
• Levetiracetam: neuropathic pain and migraine
• Oxcarbazepine: neuropathic pain; diabetic neuropathy
• Bupropion: neuropathic pain
• Transdermal fentanyl: low back pain
27
*Applications not approved by FDA.
Summary
• Chronic neuropathic pain is a disease, not a symptom
• “Rational” polypharmacy is often necessary
– combining peripheral and central nervous system
agents enhances pain relief
• Treatment goals include:
– balancing efficacy, safety, and tolerability
– reducing baseline pain and pain exacerbations
– improving function and QOL
• New agents and new uses for existing agents offer
additional treatment options
28