PGS_PedScore - North East Sleep Society
advertisement

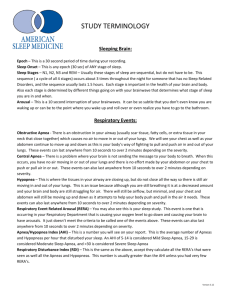
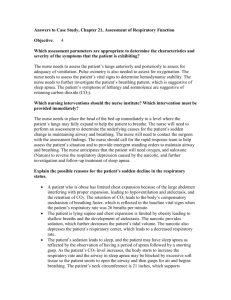
Pediatric Sleep Scoring Issues Patrick Sorenson, MA, RPSGT Infant & Pediatric Scoring April, 2011 NESS Newport, RI Staging Section Newborn: Sleep-Wake Cycles Ultradian A newborn spends approx. 70% of every 24 hrs in sleep. Cycles last about 40-60 minutes Feedings occur about every 3-4 hours-use demand not schedules. Quiet sleep Active Sleep Awake REM/NREM Developmental Distributions 90% 80% 70% 60% 50% REM NREM 40% 30% 20% 10% 0% Premies Infants Toddlers Teens Adults Quiet Sleep (QS, Stage N) Quiet sleep is analogous to NREM sleep • EEG - characterized by high amplitude (14 to 35 µV), slow wave (0.5-5 Hz) patterns. • Trace’ Alternant patterns consist of 2 to 6 second bursts of high amplitude slow waves separated by 4 to 8 seconds of low-voltage mixed activity. TA appears by about 28 weeks GA, becomes associated with QS by ~32 weeks. TA appears in its mature form by ~36 weeks. Quiet Sleep-EEG findings, cont. • Sleep spindles appear by ~4 weeks and develop rapidly through 8 weeks of age and clearly characterize NREM sleep by 3 months of age. – Coincidental with the social smile. • K-complexes first appear at ~4-6 months and are fully developed by about 2 years of age. Quiet SleepPhysiological Findings • Slower cardiac rhythm as compared to Active Sleep • Slower respiratory rates • Resting levels of muscle tone Active Sleep (AS, Stage R) Active Sleep is analogous to REM sleep • EEG is characterized by low-voltage fast desynchronous activity w/bilaterally synchronous REM’s. • Variable frequency ranges from 14-35 µV (usually in the 20-30 µV range). Active Sleep (Stage R) Physiological Findings • Increased or variable cardiac rate • Increased or variable respiratory rate; primarily costal in nature • Out-of-phase chest and abdominal effort channels. Inhibition of muscle tone in infant’s chest wall musculature. • Frequent brief movements, grimaces, peeking, vocalizations, grunts, sucking, tremors & squirming are all common in AS. Esophageal pH • Ability to interface pH equipment with polygraph and slow-chart writer • Examine the relationship between GER and apnea • GER is most commonly seen during fussy wakefulness • Document all feeds, meds and GER episodes 2007 AASM Rules for Staging Children • Pediatric sleep scoring rules start at 2 months postterm • Same terminology as adults with addition of NREM (N) as depending upon features seen. • N = Ø K’s, spindles or high amp slow-wave (0.5-2 Hz) • N2 = presence of K’s and spindles • Once N2 & N3 features are present, begin scoring as older child/adult – N1, N2, N3 & R. • Usually 5-6 months PT, but sometimes as young as 4-4.5 months. 2007 AASM Rules for Staging Children – Dominant Posterior Rhythm (DPR) • DPR changes with age – 3.5-4.5 Hz 3-4 months PT – 5-6 Hz by 5-6 months PT – 7.5-9.5 Hz by 3 years. • Amplitude also changes • Still score sleep onset if DPR ≤ 50% of the epoch • Eye movements are key! Incidence of sleep terrors • Confusional arousals seen in about 510% of all children, though regular nighttime awakenings are seen in 5070% of children 2-10 years old. • Occur in about 3% of prepubertal children and less than 1% of adults. • Onset of symptoms is about 2-4 years. Can occur at any age. • General sleep architecture w/vulnerable transition periods. W 1 ? REM 2 3 4 1 2 3 4 Hour 5 6 7 8 Begin Respiratory Section The “How to” • Sensor used to detect absence of airflow for identification of an apnea is an oronasal thermal sensor • Sensor for detection of airflow for identification of a hypopnea is a nasal air pressure transducer without the square root transformation of the signal • Acceptable sensors for detection of respiratory effort are either esophageal manometry, or calibrated or uncalibrated inductance plethysmography • Sensor for detection of blood oxygen is pulse oximetry with a maximum acceptable signal averaging time of 3 seconds • Acceptable methods for assessing alveolar hypoventilation are either transcutaneous or end-tidal CO2 monitoring Sleep Foundations 27 Oxygenation Sensors • Pulse oximetry • < 3 seconds averaging time • Pulsewave = plethysmograph Nasal pressure in children • Need: – More than one airflow measure. – Way of simultaneously measuring PCO2. Dual PN / CO2 system (commercial) Age Criteria • Criteria for respiratory events during sleep for infants and children can be used for children <18 years, but an individual sleep specialist can choose to score children ≥ 13 years using adult criteria. Sleep Foundations 31 Normative data ages 1-17 y 6 5 4 N 3 2 1 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Age (y) Marcus, Am Rev Respir Dis 1992; 146:1235 Results • Obstructive AI = 0.1 + 0.5 / hr • Obstructive AHI = 0.2 + 0.6 / hr* *Witmans, AJRCCM 2003; 168:1540 Normative data ages 1-15 y Uliel, Chest 2004; 125:872 Results • Mean obstructive AI = 0 / hr • Mean obstructive AHI = 0 / hr The Rules Score a respiratory event as an obstructive apnea if it meets all of the following criteria: • Event lasts for at least 2 breaths (or the duration of 2 breaths as determined by baseline breathing pattern) • Event is associated with a >90% fall in the signal amplitude for ≥ 90% of the entire respiratory event compared to the pre-event baseline amplitude • Event is associated with continued or increased inspiratory effort throughout the entire period of decreased airflow • Duration of the apnea is measured from the end of the of the last normal breath to the beginning of the first breath that achieves the preevent baseline inspiratory excursion Sleep Foundations 36 Obstructive apnea Definition MEETS ALL OF THE FOLLOWING: • > 2 missed breaths • > 90% fall in flow amplitude • No arousal / SaO2 criteria Mixed Events? Score a respiratory event as a mixed apnea if it meets both duration and flow amplitude criteria, and it is associated with absent inspiratory effort in the initial portion of the event, followed by resumption of inspiratory effort before the end of the event Sleep Foundations 39 Central Events Score a respiratory event as a central apnea if it is associated with absent inspiratory effort throughout the entire duration of the event and one of the following is met: • • Event lasts 20 seconds or longer Event lasts at least 2 missed breaths (or the duration of 2 breaths as determined by baseline breathing pattern) and is associated with an arousal, an awakening or a ≥ 3% desaturation Sleep Foundations 40 Central Event Central Apnea > 20 sec (Infants) Duration of apnea (sec) 40 36 32 28 24 20 16 0 2 4 6 8 10 12 14 16 Age (weeks) Hunt, Pediatr Res 1996; 39:216 18 20 Infant CA, cont. • Apnea of Prematurity: Slowed or retarded maturation of the Arcuate Nucleus and Carotid Chemoreceptors can inhibit natural respiratory drive mechanisms • Central Apnea commonly follow sighs as the drive to breathe is temporarily inhibited • Periodic Breathing consists of central pauses of 3 or more seconds followed by normal breathing for up to 20 seconds Infant CA, cont. • Periodic Breathing is most prevalent in premature infants and is usually separated by bursts of 2-4 quick breaths between complete respiratory drive inhibition • By 3 months, normal PB consists of < 3% of total sleep time • Respiratory drive seems to be reset at birth Apnea of Prematurity Can worsen with: • Anemia-below normal reduction of erythrocytes in the quantity of hemoglobin. • Septicemia-pathogenic microorganisms or their toxins are present in the blood. • Hypoxia-reduced O2 supply to tissue. • GER-Gastroesophageal Reflux. • Seizures-electrical disturbance of the CNS. Pediatric Hypopnea Rules Score a respiratory event as a Hypopnea if it meets all of the following criteria: • Event is associated with a ≥ 50% fall in the amplitude of a nasal pressure or alternative signal compared to the pre-event baseline excursion • Event lasts at least 2 missed breaths (or the duration of 2 breaths as determined by baseline breathing pattern) from the end of the last normal breathing amplitude • The fall in the nasal pressure signal amplitude must last for ≥ 90% of the entire respiratory event compared to the signal amplitude preceding the event • Event is associated with an arousal, awakening or ≥ 3% desaturation Sleep Foundations 46 Hypopnea Definition • MEETS ALL OF THE FOLLOWING: • > 2 missed breaths • > 50% fall in amplitude • Arousal / awakening / > 3% desaturation RERA’s Score Respiratory Effort Related Arousal (RERA) if conditions below are met: • When using a nasal pressure sensor all of the following must be met: – Discernable fall in the amplitude of signal from a nasal pressure sensor, but it is less than 50% in comparison to the baseline level – Flattening of the nasal pressure waveform – Event accompanied by snoring, noisy breathing, elevation in the endtidal PCO2, transcutaneous PCO2, or visual evidence of increased work of breathing – Duration of event is at least 2 breath cycles (or the duration of 2 breaths as determined by baseline) Sleep Foundations 48 RERA definition (PN) • • • • • MEETS ALL OF THE FOLLOWING: < 50% fall in amplitude Flattened waveform > 2 breaths Snoring, WOB, CO2 Use of Pes for RERA When using an Esophageal Pressure Sensor (Pes) all of the following must be met: • There is a progressive increase in inspiratory effort during the event • Event is accompanied by snoring, noisy breathing, elevation in the end-tidal PCO2, transcutaneous PCO2 or visual evidence of increased work of breathing • Duration of the event is at least 2 breath cycles (or the duration of 2 breaths as determined by baseline breathing pattern) Sleep Foundations 50 RERA definition (Pes) MEETS ALL OF THE FOLLOWING: • Progressive increase in inspiratory effort • > 2 breaths • Snoring, WOB, CO2 Child with UARS Flow Chest Abdo Pes * * * Hypoventilation Rule Score the presence of sleeprelated hypoventilation when >25% of the total sleep time as measured by either the transcutaneous PCO2 and/or tidal CO2 sensor(s) is spent with a CO2 >50 mm Hg. Sleep Foundations 53 Noninvasive CO2 measurements • Moderate to high correlations between transcutaneous / end-tidal and arterial CO2. • Largest discrepancies occur in hypercapnic subjects or subjects with respiratory disease. • End-tidal CO2 tends to underestimate arterial CO2. • Transcutaneous CO2 tends to have a smaller bias then end-tidal PCO2, with a tendency for overestimating CO2. ETCO2 Waveform •1. Inspiratory baseline •2. Expiratory upstroke •3. Expiratory plateau •4. Inspiratory downstroke ETCO2 is range-based. Individual values are of little use. Torr & mm/Hg mean the same thing The capnograph trace End-tidal measurements • Breath-by-breath changes • Need good waveform with plateau • Uncomfortable • Poor signal: – Mouth-breathing – Secretions – Tachypnea, small lung volumes Transcutaneous measurements • Slow response rate • Well tolerated • Problems: – Burns – Required repositioning every 4 hours – Poor perfusion – Skin lesions Periodic Breathing Rule Score Periodic Breathing if there are: >3 episodes of central apnea lasting > 3 seconds separated by no more than 20 seconds of normal breathing Sleep Foundations 61 Sudden Infant Death Syndrome (SIDS) The sudden and unexpected death of an infant for which sufficient cause cannot be found by a death scene investigation, review of the history, and a postmortem examination. Respiratory Drive Chart 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Birth-FT 1 week 2 weeks 3 weeks 1 month Thermoregulation Chemoreception This graph shows the rate per 1,000 live births for infant deaths during the neonatal period (between the ages of birth through 27 days) in the United States. PSG night-to-night variability (sleep architecture) 100 80 60 Night 1 Night 2 40 20 0 Sleep Efficiency REM (% TST) Arousal Index (N/hr) (%) Katz, J Pediatr 2002; 140:589 PSG variability (respiratory) 100 80 60 Night 1 Night 2 40 20 0 AHI (N/hr) SaO2 Nadir (%) Hypoventilation (% TST) Katz, J Pediatr 2002; 140:589 Reliability of infant respiratory scoring • Scoring of apnea • Based on RIP • k = 0.65 • After training: k = 0.85 Corwin, Pediatr Res 1998; 44:682 Summary • Most scoring is similar to former ATS pediatric criteria. • Established the 1st criteria for pediatric hypopnea scoring. Major differences between pediatric and adult scoring • CA scoring: > 20 seconds OR associated abnormalities. • Obstructive events: > 2 breaths. • CO2 usually measured. Time for questions? • Please use microphone if available.