Motivational Interviewing - UCLA Integrated Substance Abuse

Using Motivational Interviewing
Albert L. Hasson, M.S.W.
Outpatient Clinical Research Center
Pacific Southwest Addiction Technology Transfer Center
UCLA Integrated Substance Abuse Programs
UCLA David Geffen School of Medicine, Dept. of Psychiatry www.psattc.org
www.uclaisap.org
Motivational
Interviewing
What are we talking about?
What does
“MOTIVATION” mean to you?
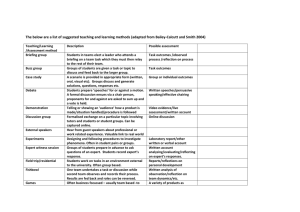
Traditional approach
Motivating for change
UNDERSTANDING HOW
PEOPLE CHANGE: MODELS
Activity
• In groups of two
• What is something about yourself that you
– Want to change
– Need to change
– Should change
– Have been thinking about changing, but you haven’t changed yet
(something you’re ambivalent about)
Activity
• Tell them how much they need to make this change
• Give them list of reasons for doing so
• Emphasize the importance of changing
• Tell them how to change
• Assure them that they can do it
• Pressure them to get on with it
Directing Style of Helping
• Tell them it’s important
• Show them how to do it
• Explain it to them, how life could be better
• Threaten them, instill fear
• Give them short term goals
• Make them a list
• Constantly remind them
• Tell them what you expect
Listen with the goal of fixing the dilemma.
• Once you understand the problem:
1. Ask as few questions as possible
2. Convince the person to change
3. Tell them why they need to change
4. Offer advice for change
5. End the session by telling them the consequences of not changing.
Roadblocks to Communication
Roadblocks to
Communication
-Ordering, directing
-Warning or threatening
-Giving advice
-Persuading, arguing, lecturing
-Moralizing, preaching, telling clients what they “should” do
-Excessive reassuring, sympathizing, consoling
-Questioning or probing excessively
-Withdrawing, distracting, humoring
-Cultural/Racial roadblocks -Disagreeing, judging, blaming
-Praising prematurely or in excess
-Shaming, ridiculing, labeling
-Organizational roadblocks
-Gender/Age roadblocks
Directing Style of Helping
Given that you are caring, compassionate, well-intended, and that your advice is sound…
…why does your directing helping style not work as well as you would hope?
Guiding Style of Helping
• Respect their decisions
• Have them to describe what is working
• Ask them about their plan
• Find out what’s important to them
• Have them talk about their health and their goals
• Ask what their goals are for treatment
Guiding Style of Helping
• Motivational Interviewing can be considered a specialized subset of a Guiding style.
• How does MI work to facilitate change?
– Reduces resistance
– Raises discrepancy
– Elicits change talk
What is Motivational
Interviewing?
Developed by William Miller (U New Mexico), Stephen Rollnick
(Cardiff University School of Medicine), and colleagues over the past three decades. Miller and Rollnick (2012, p. 29) define MI as:
“MI is designed to strengthen personal motivation for and commitment to a specific goal by eliciting and exploring the person’s own reasons for change within an atmosphere of acceptance and compassion.”
The Underlying Spirit of MI
Partnership
Compassion
MI
Spirit Acceptance
Evocation
Four Processes of MI
Focusing
Engaging
Planning
Evoking
What’s the Best Way to Facilitate Change?
• Constructive behavior change comes from connecting with something valued, cherished and important
• Intrinsic motivation for change comes out of an accepting, empowering, safe atmosphere where the painful present can be challenged
A Personal Change
Think about the most difficult change that you had to make in your life.
How much time did it take you to move from considering that change to actually taking action?
Where do I start?
• What you do depends on where the patient is in the process of changing
• The first step is to be able to identify where the patient is coming from
The Concept of Motivation
• Motivation is influenced by the clinician’s style
• Motivation can be modified
• The clinician’s task is to elicit and enhance motivation
• “Lack of motivation” is a challenge for the clinician’s therapeutic skills, not a fault for which to blame our clients
The Concept of
Ambivalence
• Ambivalence is normal
• Clients usually enter treatment with fluctuating and conflicting motivations
• They “want to change and don’t want to change”
• “Working with ambivalence is working with the heart of the problem”
MI - The Spirit (1) : Style
• Nonjudgemental and collaborative
• based on patient and clinician partnership
• gently persuasive
• more supportive than argumentative
• listens rather than tells
• communicates respect for and acceptance for patient and their feelings
MI - The Spirit (2) : Style
• Explores patient’s perceptions without labeling or correcting them
• no teaching, modeling, skill-training
• resistance is seen as an interpersonal behaviour pattern influenced by the clinician’s behavior
• resistance is met with reflection
MI - The Spirit (3) : Patient
• Responsibility for change is left with the patient
• Change arises from within rather than imposed from without
• Emphasis on patient’s personal choice for deciding future behavior
• Focus on eliciting the patient’s own concerns
MI - The Spirit (4) : Clinician
• Implies a strong sense of purpose
• Seeks to create and amplify the patient’s discrepancy in order to enhance motivation
• Elicits possible change strategies from the client
• Systematically directs patient toward motivation for change
MI Skills and Strategies
Core Skills
• O pen-Ended Questions
• A ffirmations
• R eflective Listening
• S ummarizing
Open-Ended Questions
Are difficult to answer with brief replies or simple “yes” or “no” answers.
Contain an element of surprise; you don’t really know what the patient will say.
Are conversational door-openers that encourage the patient to talk.
Is this an open-ended or closed-ended question?
Open and Closed
Questions Quiz
1. Don’t you think your drinking is part of the problem?
2. Tell me about when you were able to quit smoking?
3. How is it going with managing your pain meds?
4. Do you know you might die if you don’t stop using?
5. What do you want to do about your drinking?
6. Can you tell me about what you know about your heart condition?
O
C
O
C
C
O
Converting Closed Questions
1. Do you think your drug use is a problem?
2. Do you have any health problems related to your drinking?
3. Have you considered getting some professional help?
4. Are you worried about dying?
5. Would there be any benefits to not smoking marijuana?
Core Skills
• O pen-Ended Questions
• A ffirmations
• R eflective Listening
• S ummarizing
Affirmations
• Focused on achievements of individual
• Intended to:
– Support person’s persistence
– Encourage continued efforts
– Assist person in seeing positives
– Support individual’s proven strengths
Core Skills
• O pen-Ended Questions
• A ffirmations
• R eflective Listening
• S ummarizing
The Communication Cycle
1. What the patient says.
2. What the patient actually means.
4. What the clinician says he or she heard.
Accurate
Empathy
2 = 4
3. What the clinician hears.
Levels of Reflection
Simple
Exactly repeating one or more aspects of what is said or changing one or more of the words used in a statement (no meaning is added)
Complex
Reflecting the inferred meaning of a statement or paraphrasing that focuses on the emotional aspect of the statement (meaning is added on to what was said)
Reflective Listening
Making your best guess about what a patient means.
What does the patient mean?
I should stop using it.
Tell me about your marijuana use.
What does this patient mean?
I know I shouldn’t have.
He just came by and I couldn’t turn him away.
What made you decide to see him?
What does the patient mean?
What about it?
What difference does it make?
How are things going with the medication?
Forming Reflective
Statements
If you find it helpful, start your reflections with the following:
“It sounds like you…”
“You’re feeling…”
“It seems that you…”
“So you…”
1. Simple Reflection (repeat)
2. Amplified Reflection
(amplify/exaggerate the consumer’s point)
3. Double-Sided Reflection
(captures both sides of the ambivalence)
NIDA-SAMHSA Blending
Initiative
Reflections
Patient says:
• I’m so tired of this life.
I’ve tried to get clean so many times and it only works for a little while, then I’m out using again and it’s worse than before. I don’t know what to do.
Simple Reflection
(repeat)
• You’re so tired of using and you don’t know what to do about it.
• Every time you start using again it gets worse and you don’t know what to do .
Reflections
Patient says:
• I’m so tired of this life. I’ve tried to get clean so many times and it only works for a little while, then I’m out using again and it’s worse than before. I don’t know what to do.
Amplified Reflection
(continuing the thought)
• You’re so tired of getting high and you’re confused as to how to get out of this.
• Every time you relapse it gets worse and you don’t know if you’ll be able to stop. You’re afraid you’ll always be hooked
Reflections
Patient says:
• I’m so tired of this life.
I’ve tried to get clean so many times and it only works for a little while, then I’m out using again and it’s worse than before. I don’t know what to do.
Amplified Reflection
(emphasizes the patient’s point; add intensity; overstate)
• You’re so discouraged about staying clean, you’re not sure you should even bother anymore.
• Every time you relapse it gets worse, so why even bother trying.
Reflections
Patient says:
• I’m so tired of this life. I’ve tried to get clean so many times and it only works for a little while, then I’m out using again and it’s worse than before. I don’t know what to do.
Double-sided Reflection
(captures both sides of ambivalence)
• On the one hand you want to get clean, and on the other hand , you’re not sure if you can do it so why bother?
• It’s a real struggle for you to stay off drugs, and at the same time you know it’s important for you to keep trying.
Simple Reflections
• Stay very close to the speaker’s original words and meaning
• Patient: Everybody out there is trying to make me confused.
• Clinician: ??
• Patient: Usually when I get depressed, I just try to stay busy, and it eventually goes away.
But this time…..I can’t seem to shake it.
• Clinician: ??
Amplified Reflection: Example
• Continues the thought; takes a guess at what client really means and/or feels
• Patient: Everyone should just relax. I’m doing the best I can at dealing with these symptoms.
• Clinician: ???
• Patient: I don’t know how I’m going to come here every day. What do these people expect of me?
• Clinician: ???
Amplified Reflection: Example
• Emphasizes the patient’s point; add intensity; overstate and make it big
• Patient: I think things are fine with my life right now.
• Clinician: ???
• Patient: You know if my mom would just back off, I would not be as tense and I wouldn’t have these problems.
• Clinician: ???
Double Sided Reflections
So on the one hand you…..and on the other you want……..
Patient: I know it might not be good for me, but it is the only thing that helps me sleep.
Clinician: ??
patient: I know that it is a bad idea to keep secrets from my family. I just don’t want them to know how depressed I’ve been.
Clinician: ???
Empathic Listening & Reflections
Reflective Listening Exercise
Talk about a personal change you are making.
Listener will only respond with reflections. No
Questions.
The Listener will use as many amplified, and double-sided reflections as possible.
Types of Reflective
Statements:
1. Simple Reflection (repeat)
2.
Amplified Reflection
(continue the paragraph, amplify/exaggerate the client’s point)
4. Double-Sided Reflection
(captures both sides of the
Questions to guide you:
▫ Where are they going with this?
▫ How do they feel about this?
▫
What do they really mean?
▫ What have they said?
▫ How does this affect how they think?
▫ How does this affect how they feel about themselves ambivalence) or their world?
End —Ready for Round 2?
5 min
Types of Reflective
Statements:
1. Simple Reflection (repeat)
2.
Amplified Reflection
(continue the paragraph, amplify/exaggerate the client’s point)
4. Double-Sided Reflection
(captures both sides of the ambivalence)
End
Questions to guide you:
▫ Where are they going with this?
▫ How do they feel about this?
▫ What do they really mean?
▫ What have they said?
▫
How does this affect how they think?
▫ How does this affect how they feel about themselves or their world?
5 min
What was your experience like?
“People are better persuaded by the reasons they themselves discovered than those that come into the minds of others”
Blaise Pascal
Recognizing Change Talk
1. I don’t need to stop drinking. I need to cut down on my drinking, for sure. But I don’t need to stop.
2. I don’t want to smoke. It is just that sometimes I have such a strong urge to smoke that I can’t resist it, especially after eating.
3. I really want to be less depressed. I will not drink anymore.
4. I already take care of myself. I don’t need to see a psychiatrist. Besides, I’ve never met a psychiatrist
I’ve liked.
5. Look, I stopped smoking marijuana two weeks ago. But I’m warning you. Unless you find some other way to give me relief, I’m going to start smoking again when I leave this hospital.
Recognizing Change Talk
(cont.)
6. That program might be good at helping some people, but not me. I can change by myself.
7. I’ve had enough of drug dealing. If I don’t stay out of trouble, I’ll be dead before I know it.
8. My blood pressure is still pretty high despite all of my efforts to eat better and exercise more. I’ve been fighting the idea of taking another medication, but if I have to, then I guess I will.
9. I don’t ever want to end up in a psych ward again.
I am really sick and tired of being sick and tired.
10.Okay, I get it. If I keep shooting dope, my heart might get re-infected. So what?
5 Key MI Principles
• Reduce ambivalence & develop discrepancy
• Facilitate self-motivational statements
• Express empathy
• Avoid or “roll with” resistance
• Use counseling skills to elicit discussion about change
– Open-ended questions
– Affirmations
– Reflective listening
– Summarizing
Engaging
• The process of establishing a mutually trusting and respectful helping relationship
Developing Discrepancy
• Clarify important goals for the client
• Explore the consequences or potential consequences of the client’s current behaviours
•
Create and amplify in the client’s mind a discrepancy between their current behaviour and their life goals
Expressing Empathy through
Reflective Listening
Expressing Empathy through
Reflective Listening
•
•
•
•
Reflective listening is used to:
Check out whether you really understood the client
Highlight the client’s own motivation for change about substance use
Steer the client towards a greater recognition of her or his problems and concerns, and
Reinforce statements indicating that the client is thinking about change.
It’s not about the nail…
Building Motivation
(the microskills)
• Open-ended questioning
• Affirming
• Reflective listening
• Summarizing
The goal is to elicit and reinforce self-motivational statements (Change Talk)
Putting It All Together
• Use the microskills in all interactions
– Open ended questions
– Affirmations
– Reflections
– Summary
• Remember that your goals are the client’s goals. You may need to start very small and very slowly. The goal is forward movement.
Recognizing Resistance
Resistance is when patients :
• argue
• interrupt
• fail to link (problems to use)
• ignore problems
• fail to engage or follow through
Where does resistance start?
Rolling with Resistance
To reduce resistance:
• Shift the focus
• Reframe
• Emphasize personal choice and control
• Stop providing solutions
• Talk about something else
Steps in Motivational
Interviewing
1. Assess the client
2. Explore the behaviors.
3. Summarize and help the client make a decision (using the Decision Matrix)
4. Help set goals
Step 1: Assess the Patient
• Establish rapport
• Show empathy
• Take a drug use history (typical day)
• Provide results and feedback on the assessment
• Determine the stage of change and willingness to talk directly about changing drug use
Step 2: Explore the Behaviors
• Decisional balance (good versus not-so-good)
– Listen for change talk
• Use the readiness/confidence rulers
– Listen for change talk
THE DECISIONAL BALANCE
The good things about
______
The notso-good things about ____
• Open-ended questioning
• Affirming
The notso-good things about changing
The good things about changing
• Reflective listening
• Summarizing
Avoid questions that inspire a yes/no answer.
The Readiness Ruler
• How important is your drug use to you?
– On a scale of 1-10
– (1 = not important, 10 = very important)
• How confident are you about changing?
– On a scale of 1-10
– (1 = not confident, 10 = very confident)
• Why did you score yourself so high/low? Why wasn’t it lower?
• What would help to move you higher on the scale?
1 2 3 4 5 6 7 8 9 10
Step 3: Summarize and help the client make a decision
• Restate the dilemma or ambivalence:
– “You were saying that your were trying to decide whether to continue or cut down on _______”
– “After this discussion, are you more clear about what you would like to do?“
– “So have you made a decision about what you would like to work on?”
– (How would you change the above questions?)
Step 4: Goal Setting
• What will be your next (1 st ) step now?
• What will you do in the next 1 or 2 days (week)?
• Have you already been doing something to
• achieve this? If so, can you do more of this?
• Who will be helping you on this?
• On a scale of 1-10 how confident are you that you
• will do this next step?
NOTE:
Be sure to provide praise and support self-efficacy
Change Planning
• Clarify the change goal (reduced use, abstinence)
• Talk about treatment options and services that might be available at your hospital
• Identify what the patient will do to achieve the goal
• Ask who might help the patient and how
• Ask about potential obstacles and how the patient would address them
• Develop a Change Plan Contract
What if no commitment to change is made?
• Accept it
• Empathize that ambivalence can be difficult
• Ask if he/she can manage the consequences of not making a decision
• Ask if there is anything else that will help with the decision (i.e. having more time or information, etc.)
Remember to leave the door open…
• ‘‘In summary, it seems that at the moment you don’t want to change this behavior, but if you want to talk about it further at some stage, or if you decide that it is starting to cause you problems, please feel free to come and see me again and we can discuss this further…’
What techniques should I avoid?
Techniques to avoid when motivating clients:
• Confrontation / denial
• Closed questions
• Clinician traps
• Roadblocks to reflective listening
You Are Using MI If You:
• Talk less than your consumer does
• Offer one refection for every three questions
• Reflect with complex reflections more than half the time
• Ask mostly open-ended questions
• Avoid getting ahead of your consumer’s stage of readiness (warning, confronting, giving unwelcome advice, taking “good” side of the argument)
THANK YOU!!
Albert L. Hasson, M.S.W.
alhasson@ucla.edu
For additional information on this or other training topics, visit: www.psattc.org
www.motivationalinterview.org
www.uclaisap.org/dmhcod