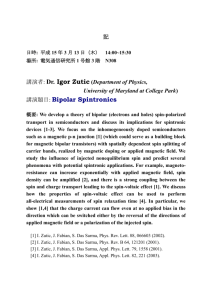
IHD Dx. Rx. by Dr Sarma
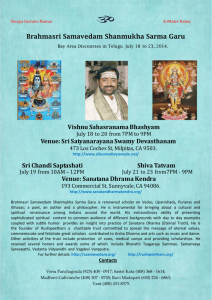
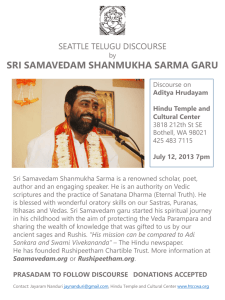
advertisement

Dr. R.V.S.N.Sarma, M.D., M.Sc (Canada) Consultant Physician and Chest Specialist 1, Jayanagar, Tiruvallur, Chennai -602 001 (04116) – 260593, 263665 Mobile 098940 60593 palmsprings@eth.net Dr.Sarma@works Ischemic Heart Disease Diagnosis & Management We’ve come a long way in the treatment of MI “ There’s too much confusion, Never, I can’t get neither no relief ” Jimi Hendrix, Purple Haze, 1968 “In this world, nothing can be said to be certain except death and taxes.” Benjamin Franklin 13 November 1789 (letter) Lysis or Life-flight ? Comorbidity of Atherosclerotic Disease a major health burden • Atherothrombosis • major complications of atherosclerosis are thrombosis, with local occlusion or distal embolization CAD CVA PAD Aronow WS, Ahn C. Am J Cardiol. 1994;74:64–65. Atherosclerosis Time-line Foam Cells Fatty Streak Intermediate Lesion Atheroma Fibrous Plaque Complicated Lesion/ Rupture Endothelial Dysfunction From First Decade From Third Decade Adapted from Pepine CJ. Am J Cardiol. 1998;82(suppl 104). From Fourth Decade Left Coronary Artery Right Coronary Artery Overview of CAD Presentation • • • • • Assessment of CAD likelihood Risk stratification based on findings Anti-ischemic drug therapy Anti-platelet/ anti thrombotic therapy Invasive versus conservative strategy – Primary PTCA versus Thrombolytic Rx. • Secondary prevention and risk factor modification Dr.Sarma@works Clinical Assessment The two critical questions 1. What is the likelihood that the signs and symptoms represent ACS secondary to obstructive CAD ? 2. What is the likelihood of an adverse clinical outcome? like risk of death and nonfatal cardiac ischemic events (new or recurrent MI, recurrent UA, disabling angina that requires hospitalization, and/or urgent coronary revascularization) Dr.Sarma@works History - Likelihood of ischemia The 5 most important factors, ranked in the order of importance, are 1. Nature of the anginal symptoms 2. Prior history of CAD 3. Sex 4. Age 5. Number of traditional risk factors present Dr.Sarma@works Classical Angina Angina is characterized as a deep, poorly localized chest or arm discomfort that is reproducibly associated with physical exertion or emotional stress and is relieved promptly (in less than 5 min) with rest and/or the use of sublingual nitroglycerin (NTG) Dr.Sarma@works Clinical Classification of Chest Pain Typical angina (definite) 1) substernal chest discomfort with a characteristic quality and duration that is ... 2) provoked by exertion or emotional stress and 3) relieved by rest or nitroglycerin Atypical angina (probable) meets 2 of the of characteristics Noncardiac chest pain meets 1 of the typical angina characteristics Dr.Sarma@works J Am Coll Cardiol. 1983;1:574, Letter Differential Diagnosis of Prolonged Chest Pain • • • • AMI Aortic dissection Pericarditis Atypical angina pain associate with hypertrophic cardiomyopathy • Esophageal, other upper gastrointestinal, or biliary tract disease • Pulmonary disease – pneumothorax – embolus with or without infarction – pleurisy: infectious, malignant, or immune disease-related • Hyperventilation syndrome • Chest wall – skeletal – neuropathic • Psychogenic Dr.Sarma@works Chest Pain Checklist YES • • • • • • • • • NO • • • • • • • Ongoing chest discomfort ( 20 min and < 12 hours) Oriented, can cooperate Age > 35 y (> 40 if female) ECG done High-risk profile * Heart rate 100 bpm Blood pressure 100 mm Hg Pulmonary edema (rales > 1/2 way up) Shock History of stroke or TIA Known bleeding disorder Active internal bleeding in past two weeks Surgery or trauma in past two weeks Terminal illness Jaundice, hepatitis, kidney failure Use of anticoagulants • Systolic/diastolic blood pressure Right arm ____/____ Left arm ____/____ • 1. Pain began 2. Arrival time 3. Begin transport 4. Hospital arrival ____ AM/PM ____ AM/PM ____ AM/PM ____ AM/PM Check each finding. If all [YES] boxes are checked and ECG indicates ST elevation or new BBB, reperfusion therapy with fibrinolysis or primary PTCA may be indicated. Fibrinolysis is generally not indicated unless all [NO] boxes are checked and BP 180/110 mm Hg. * Transport to a facility capable of angiography and revascularization if needed Adapted from the Seattle/King County EMS Medical Record Dr.Sarma@works Acute Coronary Syndrome Ischemic Discomfort Unstable Symptoms No ST-segment elevation Unstable Angina History Physical Exam ST-segment elevation NSTEMI (Non-Q MI) STEMI (Q-wave MI) (positive cardiac biomarker) Dr.Sarma@works ECG (10 min) Cardiac Biomarkers ACC/AHA Classifications Expert Opinion and Recommendations I IIa IIb III Intervention is useful and effective Evidence conflicts/opinions differ but leans towards efficacy Evidence conflicts/opinions differ but leans against efficacy Intervention is not useful/effective and may be harmful Dr.Sarma@works JACC 1999; Vol 33, No 7:2092-197 12 Lead Resting ECG • should be recorded in all patients with symptoms suggestive of angina pectoris • normal in 50% of patients • a normal ECG does not exclude severe CAD; however, it does imply normal LV function with favorable prognosis Dr.Sarma@works Tools for Risk Stratification • The 12-lead ECG lies at the center of the decision pathway for the evaluation and management of patients with ischemic discomfort. A recording made during an episode of presenting symptoms is particularly valuable. Importantly, transient ST-segment changes (> 0.05 mV) that develop during a symptomatic episode at rest and that resolve when the patient becomes asymptomatic strongly suggest acute ischemia and a very high likelihood of underlying severe CAD Dr.Sarma@works Risk Stratification: abnormal rest ECG • Evidence of >1 prior MI (Q waves or R wave in lead V1 for posterior infarction) • A "QRS score" to indicate the extent of old or new MI • persistent ST-T wave inversions, particularly in leads V1 to V3 of the rest ECG, is associated with an increased likelihood of future acute coronary events and a poor prognosis • LV hypertrophy by ECG criteria in a patient with angina pectoris is also associated with increased morbidity and mortality • A decreased prognosis is also likely when the ECG shows left bundle-branch block, bifascicular block (often left anterior fascicular block plus right bundle-branch block), second- or thirddegree atrioventricular block, atrial fibrillation or ventricular tachyarrhythmias Dr.Sarma@works Am J Cardiol 1982;49:1604-14 Risk stratification: Chest X-Ray • often normal in patient with stable angina pectoris • usefulness as a routine test is not well established • findings associated with poorer long-term prognosis – cardiomegaly – LV aneurysm – pulmonary venous congestion Dr.Sarma@works – left atrial enlargement Cardiac Troponins • Advantages – powerful tool for risk stratification – greater sensitivity and specificity than CK-MB – detection of recent MI up to 2 weeks after onset • Disadvantages – low sensitivity in very early phase of MI (< 6 h after symptom onset) – limited ability to detect late minor reinfarction • Clinical recommendations – useful as a single test to efficiently diagnose NSTEMI (including minor myocardial damage), with serial measurements Dr.Sarma@works CK-MB • Advantages – rapid, cost-efficient, accurate assays – ability to detect early reinfarction • Disadvantages – loss of specificity in setting of skeletal muscle disease or injury, including surgery – low sensitivity during very early MI (< 6 h after symptom onset) or later after symptom onset (> 36 h) and for minor myocardial damage (detectable by troponins) • Clinical recommendations – prior standard and still acceptable diagnostic test in most clinical circumstances Dr.Sarma@works Myoglobin • Advantages – – – – high sensitivity useful in early detection of MI detection of reperfusion most useful in ruling out MI • Disadvantages – very low specificity in setting of skeletal muscle injury or disease – rapid return to normal range limits sensitivity for later presentations • Clinical recommendations – should not be used as only diagnostic marker because of lack of cardiac specificity Dr.Sarma@works Tools for Risk Stratification • Biomarkers are of critical importance in the evaluation of patients with UA/NSTEMI. The troponins offer great diagnostic sensitivity because of your ability to identify patients with lesser amounts of myocardial damage. Nevertheless, these lesser amounts of damage are associated with high-risk patients with ACSs because they are thought to represent microinfarctions that result from microemboli from an unstable plaque. Dr.Sarma@works Serum Cardiac Markers • CK-MB subfomes for Dx within 6 hrs of MI onset • cTnI and cTnT efficient for late Dx of MI • CK-MB subform plus cardiac-specific troponin best combination • Do not rely solely on troponins because they remain elevated for 7-14 days and compromise ability to diagnose recurrent infarction Dr.Sarma@works Myocardial Markers MARKER 1st SEEN REL. DURATION SENS. (median) (x Nl) (hrs) MI SENS. U.A. MYOGLOBIN 2-3 hr 12 18-24 85-90 ? TROPONIN I 4-6 50 > 144 100 30 TROPONIN T 3-4 50 > 240 100 40 MB MASS 4-6 12 24-36 100 25 CK TOTAL 6-8 8 36-48 80-85 ? CK ISOFORM 2-3 N/A 6-12 100 10? Dr.Sarma@works Size of Myocardial Infarction (grams) 100 10 1 0.1 0.01 0.001 EKG Dr.Sarma@works ECHO CK, CK- TROPONIN AST MB Enzymatic Criteria for Diagnosis of Myocardial Infarction • Serial increase, then decrease of plasma CK-MB, with a change > 25% between any two values • CK-MB > 10-13 U/L or > 5% total CK activity • increasing MB-CK activity > 50% between any two samples, separated by at least 4 hrs • if only a single sample available, CK-MB elevation > twofold • beyond 72 hrs, an elevation of troponin T or I or LDH-1 > LDH-2 Dr.Sarma@works The Progressive Development of Cardiovascular Disease Risk Factors Endothelial Dysfunction Atherosclerosis CAD Myocardial Ischemia Coronary Thrombosis Myocardial Infarction Arrhythmia & Loss of Muscle Remodeling Ventricular Dilation Congestive Heart Failure Dr.Sarma@works Endstage Heart Disease Atherosclerosis: the Pathologic Process Atherosclerotic Plaque Plaque Fissure/ Cracking/ Rupture Thrombus Formation Stabilized Plaque Chronic Ischemia Dr.Sarma@works Thrombus Incorporated into Atheroma Embolism Occlusion Acute Event Cardiac Enzyme bio-markers RELATIVECONCENTRATION M y o g l o b i n T r o p o n i n C K ,A S T L D H N o r m a l 0 6 1 2 1 8 2 4 2 3 4 5 6 7 8 9 1 0 H o u r s D a y s T I M E A F T E R I N F A R C T Dr.Sarma@works MYOFIBER STRUCTURE TnI TnC Actin Dr.Sarma@works TnT Tropomyosin Inferior MI changes fully evolved Dr.Sarma@works Posterior MI Dr.Sarma@works ST ↓ - Ischemia Lateral wall Dr.Sarma@works ST segment ↑– Acute evolving MI Dr.Sarma@works ST segment ↑– Inferio-lateral MI Dr.Sarma@works Evolution of Acute MI Dr.Sarma@works Acute MI Anterior wall Dr.Sarma@works Anterio-septal MI with RBBB Dr.Sarma@works Extensive Anterio-lateral MI Dr.Sarma@works Fully Evolved MI Anterioseptal Dr.Sarma@works MI inferio-posterior Dr.Sarma@works Inferio-posterior MI with RV MI Dr.Sarma@works Risk Factors for Atherosclerotic Disease Non-modifiable Age Family history Sex Modifiable Dr.Sarma@works Cigarette smoking Diabetes mellitus Hyperlipidemia Hypertension Obesity Physical inactivity Hoeg JM. JAMA. 1997;277:1387–1390. Vascular Endothelium • Endothelium as an organ – 1 to 6 x 1013 cells monolayer – weighs 1 kg – covers 6 tennis courts • Modulator of vascular tone – nitric oxide (NO) – prostaglandin I2 (PGI2, prostacycline) • Regulator of hemostasis – antithrombotic Dr.Sarma@works – prothrombotic Anticoagulant: •GAGs/AT III •TFPI •Thrombomodulin Procoagulant: •Tissue factor •Binding sites for coagulation factors and fibrin Profibrinolytic: •t-PA •u-PA •Binding sites for plasminogen •PA receptors Antifibrinolytic: •PAI •TAFI Platelet inhibitory: •PGI2 (prostacycline) •Nitric oxide •ADPase •Carbon monoxide Platelet activating: •vWF •PAF •Fibronectin •Endothelin-1 •TXA2 Antithrombotic Vasodilation Prothrombotic Vasoconstriction ACUTE CORONARY SYNDROME No ST Elevation ST Elevation NSTEMI Unstable Angina NQMI QwMI Myocardial Infarction Dr.Sarma@works ACUTE CORONARY SYNDROMES (ACS) Dr.Sarma@works CAUSES OF UA/NSTEMI Thrombosis Mechanical Obstruction . MVO2 Dynamic Obstruction Inflammation/ Infection Thrombosis Mechanical Obstruction . MVO2 Dynamic Obstruction Braunwald, Circulation 98:2219, 1998 Dr.Sarma@works Inflammation/ Infection ED MANAGEMENT OF UA/NSTEMI ST ? NO Nondiagnostic ECG Normal serum cardiac markers Observe Follow-up at 4-8 hours: ECG, cardiac markers No recurrent pain; Neg follow-up studies Stress study to provoke ischemia prior to discharge or as outpatient Neg: nonischemic discomfort;low-risk UA/NSTEMI Outpatient follow-up Dr.Sarma@works YES ST and/or T wave changes Ongoing pain + cardiac markers Hemodynamic abnormalities Recurrent ischemic pain or + UA/NSTEMI follow-up studies Diagnosis of UA/NSTEMI confirmed + UA/NSTEMI confirmed ADMIT Evaluate for Reperfusion INITIATION OF ATHEROCLEROSIS Dr.Sarma@works TYPES OF PLAQUES Fibrous Cap Media Lumen “Vulnerable” Plaque Lumen - T-Lymphocyte - Macrophage - Foam cell - Activated intimal SMC Lipid Core “Stable” Dr.Sarma@works Plaque Dr.Sarma@works PATHOGENESIS Molecular Basis • Normally a fine balance exists between production of collagen by smooth muscle cell & break down • Impaired gene expression disturbs this balance Dr.Sarma@works PATHOGENESIS OF ACS Dr.Sarma@works TRIGGERS OF PLAQUE RUPTURE Vulnerable Plaque Inflammatory infiltrate Plaque Thin fibrous cap Lum en Large lipid core Spontaneou s or triggered rupture Non occlusive Dr.Sarma@works thrombus Occlusive thrombus Non occlusive thrombus Occlusive thrombus Factors limiting thrombosis • Minor plaque disruption • Silent • High flow • Unstable angina • fibrinolyti • Non-Qwave MI c activity • Sudden Dr.Sarma@works death Factors favoring thrombosis • Q-wave MI • Sudden death • Major plaque disruption • Vasospasm low flow • fibrinolytic activity • Procoagulant state, such as fibrinogen, ACUTE CORONARY SYNDROME Triggering activities of patients Acute Risk Factors of an Arterial Pressure surge or Vasoconstriction lead to Plaque Disruption Minor Plaque Disruptio n NonVulnerable Vulnerable Atherosclero Atherosclero tic Plaque tic Plaque Dr.Sarma@works Major Plaque Disruptio n Acute Risk Factors of a coagulability Increase or Vasoconstriction lead to occlusion by Non-complete Occlusive Occlusive Thrombus Thrombu Thrombus s Asymptomat ic Unstable Angina or Non-Q-MI Occlusive Thrombu s Myocardia l Infarction or Sudden Cardiac Death UNSTABLE PLAQUE Dr.Sarma@works LARGE NON OCCLUDING THROMBUS DUE TO ENDOTHELIAL EROSION Dr.Sarma@works NON OCCLUDING THROMBUS DUE TO PLAQUE RUPTURE Dr.Sarma@works OCCLUSIVE THROMBUS DUE TO PLAQUE RUPTURE Dr.Sarma@works HEALED PLAQUE Dr.Sarma@works PLATELET PLUG FORMATION ADP Epinephri ne Adhesion Thrombin Collagen Arachidonic Acid release Aspiri n Thromboxane A2 Release of ADP, serotonin Ticlopidine / GP IIb/IIIa Clopidogrel exposure GP IIb/IIIa receptor blockers Dr.Sarma@works Platelet aggregation GP IIb/IIIa (quiescent) Resting Platelet Dr.Sarma@works GP IIb/IIIa (activated) Activated Platelet GP IIb/IIIa (activated) Fibrinogen Platelet Dr.Sarma@works R.G.D. Sequence vWF Competitive Antagonist (Integrilin, Aggrastat) Activated Platelet Dr.Sarma@works Thrombotic Process — Pathophysiology Plaque Characteristics & Disruption Thrombus Lumen Fibrous Cap Lipid-Rich Core Dr.Sarma@works Thinning Fibrous Cap Disruption Production of LMWH by depolymerization of unfractionated heparin Native heparin Pentasaccharide sequence Dr.Sarma@works Depolymerisation process LMWH Semin Thromb. Hemost. 1993; 19 suppl. 1: 1-11 MODE OF ACTION OF HEPARIN AND LMWH Dr.Sarma@works Dr.Sarma@works Dr.Sarma@works MODE OF ACTION OF ANTIPLATELET AGENTS Vessel Wall Injury Cyclooxygenase Arachidon ic Acid PGH2 TXA2 ADP ASPIRI N IIB Fibrinog en Platelet III a GP IIb, IIIa ADP Receptor EC Vessel wall Dr.Sarma@works TXA CLOPIDOGREL 2 ADP Lumen Platelet ANTI-PLATELET THERAPY Dr.Sarma@works Antiplatelet Agents GP IIb/IIIa Inhibitors GP IIb/IIIa Receptor Fibrinogen GP IIb/IIIa Inhibitors Dr.Sarma@works Oral Antiplatelet Agents Mechanism of Action ADP clopidogrel bisulfate ticlopidine HCl dipyridamole ADP phosphodiesterase ADP Gp IIb/IIIa (Fibrinogen Receptor) Activation Collagen Thrombin TXA2 COX TXA2 aspirin ADP = adenosine diphosphate, TXA2 = thromboxane A2, COX = Dr.Sarma@works cyclooxygenase. Schafer AI. Am J Med. 1996;101:199–209. Anticoagulants Direct Thrombin Inhibitors Hirudin-Thrombin Binding Mechanisms of Thrombin Inhibition Fibrin Binding Site Thrombin Catalytic Site Substrate Recognition Site Dr.Sarma@works Thrombin Hirudin Thrombin ATIII/ Heparin The Management of Patients with Acute Myocardial Infarction Initial Assessment and Evaluation Dr.Sarma@works Algorithm for Initial Assessment and Evaluation of the Patient with Acute Chest Pain Chest pain consistent with coronary ischemia Within 10 minutes • Initial evaluatioon • 12 lead ECG • Establish IV • Aspirin 160-325 mg - chewed • Establish continuous ECG monitoring • Blood for baseline serum cardiac markers Therapeutic/Diagnostic tracking according 12-lead ECG Nondiagnostic / normal ECG Dr.Sarma@works ECG suggestive of ischemia T wave inversion or ST depression ST segment elevation or new bundle branch block Emergency Department Algorithms/Protocol for Patients with Symptoms and Signs of AMI Onset of symptoms Ambulance presents patient to ED lobby Patient presents to ED lobby ED triage or charge nurse triages patient • AMI symptoms and signs • 12-lead ECG • Brief, targeted history Emergency nurse initiates emergency nursing care in acute care area of ED • Cardiac monitor • Blood studies • Oxygen therapy • Nitroglycerin • IV D5W • Aspirin Emergency Physician evaluates patient • History • Physical exam • Interpret ECG AMI patient? Dr.Sarma@works Emergency Department Algorithms/Protocol for Patients with Symptoms and Signs of AMI Yes AMI patient? No Uncertain Yes Fibrinolytic therapy Candidate for fibrinolytic therapy Evaluate further Trans Mural Consult Conduct education and follow-up instruction No Other indicated treatment: • Other drugs for AMI (beta-blockers, heparin, aspirin, nitrates) • Transfer to cath lab for PTCA or surgery for CABG Dr.Sarma@works Admit Release Patient with Acute Chest Pain with non-diagnostic and normal ECG Non-diagnostic / normal ECG • Continue evaluation/monitoring in Emergency Department or Chest Pain Unit • Serial serum cardiac marker levels - CKMB, Trop • Serial ECGs • Consider noninvasive evaluation of ischemia • Consider alternative diagnoses No Evidence of MI or ischemia MI or demonstrable ischemia Discharge with follow-up as appropriate (Goal: 12-24 hours) Admit to unit of appropriate intensity Dr.Sarma@works Patient with Acute Chest Pain with T-wave inversion or ST depression ECG suggestive of ischemia T wave inversion or ST depression • Anti-ischemia Therapy • Analgesia Admit to unit of appropriate intensity Admission blood work • CBC • Electrolytes, BUN, creatinine • Lipid profile Dr.Sarma@works Differential diagnosis • • • • • • • • • • ischemia acute posterior MI ventricular hypertrophy digoxin effect pericarditis pulmonary embolus LBBB hyperventilation anxiety normal variants Management of Patients with Non-ST Elevation MI ST depression/T-wave inversion: Suspected AMI Heparin + Aspirin Nitrates for recurrent angina Antithrombins: LMWH - high-risk patients Anti-Platelets: GpIIb/IIIa inhibitor Patients without prior beta-blocker therapy or who are inadequately treated on current dose of beta-blocker Establish adequate beta-blockade Dr.Sarma@works Persistnet symptoms in patients with prior beta-blocker therapy or who cannot tolerate beta-blockers Add calcium antagonist Assess Clinical Status High-risk patient: 1. Recurrent ischemia 2. Depressed LV function 3. Widespread ECG changes 4. Prior MI Clinical stability Catheterization: Anatomy suitable for revascularization Yes No PCI CABG Medical Therapy Modified from Antman EM. Atlas of Heart Disease, VIII; 1996 Continued observation in hospital Consideration of stress testing Patient with Acute Chest Pain with ST elevation or new bundle branch block ST segment elevation or new bundle branch block Assess suitability for reperfusion • ? Contraindications for fibrinolysis • Availability and appropriateness of primary angioplasty Initiate anti-ischemia therapy • Beta-blocker • Nitroglycerine Analgesia Admission blood work Initiate fibrinolysis if indicated Goal: 30 minutes from entry to ED Primary PTCA if available and suitable Goal: PTCA within 90 30 minutes Admit - CCU Dr.Sarma@works The Management of Patients with Acute Myocardial Infarction Initial Management Dr.Sarma@works Management of Patients with ST Elevation ST elevation Aspirin Beta-blocker 12 h Eligible for fibrinolytic therapy Fibrinolytic therapy contraindicated Fibrinolytic therapy Primary PTCA or CABG > 12 h Not a candidate for reperfusion therapy Persistent symptoms ? No Other medical therapy: ACE inhibitors ? Nitrates Anticoagulants Dr.Sarma@works Modified from Antman EM. Atlas of Heart Disease, VIII; 1996 Yes Consider Reperfusion Therapy Comparison of Approved Fibrinolytic Agents Streptokinase Anistreplase Alteplase Reteplase Dose 10U x 2 over 30 min Bolus administration Antigenic Allergic reactions (mostly hypotension) Systemic fibrinogen depletion 90-min patency rate TIMI-3 flow Mortality rate Dr.Sarma@works Cost /dose (US) 1.5 MU 30 mg 100 mg in 30-60 min in 5 min in 90 min NO Yes Yes Yes Yes Marked ~50% 32% 7.3% $294 Yes No No Marked ~65% 43% 10.5% $2116 No Yes No No Mild Moderate ~75% ~75% 54% 60% 7.2% 7.5% $2196 $2196 ContraindicatIons and Cautions for Fibrinolytic Used in Myocardial Infarction Absolute Contraindications: • Previous hemorrhagic stroke at any time: other strokes or cerebrovascular events within one year • Known intracranial neoplasm • Active internal bleeding (does not include menses) • Suspect aortic dissection Dr.Sarma@works ContraindicatIons and Cautions for Fibrinolytic Used in Myocardial Infarction Cautions / Relative Contraindications • Severe uncontrolled HTN on presentation (BP >180/110 mmHg) • History of prior CVA or known intra-cerebral pathology not covered in contraindications • Current use of anticoagulants in therapeutic doses (INR 2-3); no bleeding diathesis • Recent trauma (within 2-4 weeks) including head trauma Dr.Sarma@works • Noncompressible vascular punctures • Recent (within 2-4 weeks) internal bleeding • For streptokinase/anistreplase: prior exposure (especially within 5d-2 yrs) or prior allergic reaction • Pregnancy • Active peptic ulcer • History of chronic hypertension Primary Percutaneous Transluminal Coronary Angioplasty Recommendations Class I Recommendations 1. As an alternative to fibrinolytic therapy if: – – – – – ST segment elevation or new or presumed new LBBB Within 12 hrs of symptoms or > 12 hrs of persistent pain In a timely fashion (90 30 min) By experienced operators In appropriate environment 2. In cardiogenic shock patients < 75 yrs or within 36 hrs of AMI and revascularization can be performed within 18 hrs of onset of shock Class IIa Recommendations 1. As reperfusion strategy in candidates for reperfusion who have contraindications to fibrinolytic therapy Dr.Sarma@works Primary Percutaneous Transluminal Coronary Angioplasty Recommendations Class IIb Recommendations 1. In patients with AMI who do not present with ST elevation but who have reduced (< TIMI grade 2) flow of the infarct-related artery and when angioplasty can be performed within 12 hrs of onset of symptoms Class III Recommendations 1. This classification applies to patients with AMI who: • undergo elective angioplasty in the non-infarct-related artery at the time of AMI • are beyound 12 hrs after the onset of symptoms and have no evidence of myocardial ischemia • have received fibrinolytic therapy and have no symptoms of myocardial ischemia • are fibrinolytic-eligible and are undergoing primary angioplasty by and Dr.Sarma@works unskilled operator in a laboratory that does not have surgical capability Advantages of Fibrinolytic Therapy • More universal access • Shorter time to treatment • Greater clinical trial evidence of: – reduction in infarct size – improvement of LV function • Results less dependent on physician experience • Lower system costs Dr.Sarma@works Advantages of Primary PTCA • • • • • • Higher initial reperfusion rates Lower recurrence rates of ischemia / infarction Less residual stenosis Less intracranial bleeding Defines coronary anatomy and LV function Utility when fibrinolysis contraindicated Dr.Sarma@works Pharmacologic Management of Patients with MI Heparin Recommendations Class I Recommendations 1. In patients undergoing percutaneous or surgical revascularization Class IIa Recommendations 1. Intravenously in patients undergoing reperfusion therapy with alteplase/reteplase (note change in recommendations) 1999 1996 Bolus Dose 60 U/kg 70 U/kg Maintenance ~12 U/kg/hr ~15 U/kg/hr Maximum 4000 U bolus None 1000 U/h if >70kg aPTT 1.5-2.0 x control 1.5-2.0 x control (50-70 sec) for 48 hrs (50-70 sec) for 48 hrs Dr.Sarma@works Pharmacologic Management of Patients with MI Heparin Recommendations Class IIa Recommendations (continued) 2. Intravenous unfractionated heparin (UFH) or low molecular weight heparin (LMWH) subcutaneously for patients with non-ST elevation MI 3. Subcutaneous UFH (eg, 7,500 U b.I.d.) or low molecular weight heparin (eg, enoxaparin 1 mg/kg b.I.d.) in all patients not treated with fibrinolytic therapy who do not have a contraindication to heparin. In patients who are at high risk for systemic emboli (large or anterior MI, AF, previous embolus, or known LV thrombus), intravenous heparin is prefered 4. Intravenously in patients treated with nonselective fibrinolytic agents (streptokinase, anistrplase, urokinase) who are at high risk for systemic emboli (large or anterior MI, AF, previous embolus, or known LV Dr.Sarma@works thrombus) Pharmacologic Management of Patients with MI Heparin Recommendations Class IIb Recommendations 1. In patients treated with nonselective fibrinolytic agents, not at high risk, subcutaneous heparin, 7,500 U to 12,500 U twice a day until completely ambulatory Class III Recommendations 1. Routine intravenous heparin within 6 hrs to patients receiving a nonselective fibrinolytic agent (streptokinase, anistrplase, urokinase) who are not at high risk for systemic embolism Dr.Sarma@works Pharmacologic Management of Patients with MI GP IIb/IIIa Inhibitors - New Recommendations Class IIa Recommendations 1. For use in patients experiencing an MI without ST segment elevation who have some high-risk features and/or refractory ischemia, provided they do not have a contraindication due to a bleeding risk Dr.Sarma@works Classification of Inotropic Agents Agent Mechanism Inotrpic Vascular Effect Isoproterenol -1 receptor tobradycardia; ++ Major Use Dilatation Hypotension due Dobutamine -1 receptor mm Hg Dopamine Low dose: <90 mm Hg (dopaminergic) value Medium dose: (-1 receptor) High dose: (-receptor) Norepinephrine - receptor ++ Mild dilatation no pacing available Low output with SBP >90 ++ Renovascular dilatation Hypoperfusion with SBP ++ Intense constriction Intense constriction Amrinone failure of ++ Dilatation PDE inhibitor or 30 mm Hg below usual Constriction Extreme hypotension despite dopamine use Second-tier agent after dopamine / dobutamine Milrinone PDE inhibitor Digitalis Inhibts Na+-K+ dysfunction Dr.Sarma@works ++ + Dilatation Variable Established systolic LV The Management of Patients with Acute Myocardial Infarction Hospital Management Dr.Sarma@works Sample Admitting Orders Condition IV Vital signs Activity Diet Medications Dr.Sarma@works Serious NS or D5W to keep vein open q 1/2 hr until stable, the q 4 hrs and p.r.n. Notify if HR <60 or >110; BP <90 or >150; RR <8 or >22. Pulse oximetry x 24 hrs Bed rest with bedside commode and progress as tolerated after approximately 12 hrs NPO until pain free, then clear liquids. Progress to a heart - healthy diet Nasal O2 2 L/min x 3 hrs Enteric-coated aspirin daily (165 mg) Stool softener daily Beta-adrenoreceptor blockers Consider need for analgesics, nitroglycerin, anxiolytic Heart-Healthy Diet • complex carbohydrates = 50-55% of kilocalories • unsaturated fats ( 30% of kilocalories) • foods high in: – potassium (eg. fruits, vegetables, whole grains, dairy products) – magnesium ( eg. green leafy vegetables, whole grains, beans, seafood) – fiber (eg. fresh fruits and vegetables, whole-grain breads, cereals) Dr.Sarma@works Treatment Strategy for Right Ventricular Ischemia/Infarction • Maintain right ventricular preload – Volume loading (IV normal saline) – Avoid use of nitrates and diuretics – Maintain AV synchrony (AV sequential pacing for symptomatic high-degree heart block unresponsive to atropine) – Prompt cardioversion for hemodynamically significant SVT • Inotropic support – Dobutamine (if cardiac output fails to increase after volume loading) Dr.Sarma@works Treatment Strategy for Right Ventricular Ischemia/Infarction • Reduced right ventricular afterload with LV dysfunction – Intra-aortic balloon pump – Arterial vasodilators (sodium nitroprusside, hydralazine) – ACE inhibitors • Reperfusion – Fibrinolytic agents – Primary PTCA – CABG (in selected patients with multivessel disease) Dr.Sarma@works Clinical Profile of Mechanical Complications of Myocardial Infarction Variable Muscle Ventricular Free Wall Paillary Septal Defect Rupture Rupture Age (mean, years) 63 69 65 Days post MI 3-5 3-6 3-5 Anterior MI 66% 50% 25% New Murmur 90% 25% 50% Palpable thrill Yes No Rare Previous MI 25% 25% 30% Echo: 2-D Visualize defect May have PE Flail or prolapsing leaflet Doppler Detect shunt Regurgitating jet in LA PA catheterization Oxygen step up Equalization of Prominent Vwave in Hi RV diastolic pressure PCW tracing Dr.Sarma@works Modified from Labovitz AJ, et al. Cardiovasc Rev Rep. 1984; 5-948 Mortality: Medical 90% 90% 90% Surgical 50% Case report 40-90% The Management of Patients with Acute Myocardial Infarction MI Management Summary Dr.Sarma@works Initial Management in ED • Initial evaluation with 12-lead ECG in < 10 minutes – targeted history (for AMI inclusion, thrombolysis exclusion) – vital signs, focused examination • Continual ECG, automated BP, HR monitoring • IV access • Draw blood for serum cardiac markers, electrolytes, magnesium, hematology, lipid profile panel Dr.Sarma@works Initial Management in ED • Aspirin165-325 mg (chew and swallow) • Sublingual NTG unless SBP <90 or HR <50 or >100: test for prinzmetal’s angina, reversible spasm, antiischemic, antihypertensive effects • O2 by nasal prolongs, first 2-3 h in all; continue if PaO2 <90% • Analgesia: small doses of morphine (2-4 mg) as needed • Fibrinolysis or PCI if ST elevation > 1mV or LBBB (Goal: door-needle < 30 min or door-dilatation < 60-90 min) Dr.Sarma@works MI Management in 1st 24 Hours • Limited activity for 12 hours, monitor 24 hours • No prophylactic antiarrhythmics • IV heparin if: a) large anterior MI; b) PTCA; c) LV thrombus; or d) alteplase/reteplase use (for ~48 hours) • SQ heparin for all other MI (7,500 u b.I.d.) • Aspirin indefinitely • IV NTG for 24-48 hrs if no / HR or BP • IV beta-blocker if no contraindications • ACE inhibitor in all MI if no hypotension Dr.Sarma@works In-Hospital Management • • • • • • • Aspirin indefinitely Beta-blocker indifinitely ACE inhibitor (DC at ~6 wks if no LV dysfunction) If spontaneous or provoked ischemia - elective cath Suspected pericarditis - ASA 650 mg q 4-6 hrs CHF - ACE inhibitor and diuretic as needed Shock - consider intra-aortic balloon pump + cath with PCI or CABG • RV MI - fluids (NS) + inotropics if hypotensive Dr.Sarma@works Predictors of 30 day Mortality in Fibrinolysis Patients GUSTO Trial - 41,021 patients Heart rate 12% AMI Location 6% Other 10% (DM, smoking, BP; Height/Weight, Prior CVD; Time to Rx; Choice of fibrinolytic therapy; US hospital) Killip class 15% Systolic BP 24% Age 32% Dr.Sarma@works Circulation 1995; 91:1659-1668 Clinical Indications of High Risk At Predischarge Present Absent Absent Strategy I Strategy II Strategy III Symptom-Limited Exercise Test at 14-21 Days Submaximal Exercise Test at 5-7 Days Markedly Abnormal Mildly Abnormal Markedly Abnormal Mildly Abnormal Negative Negative Exercise Imaging Study Exercise Imaging Study Reversible Ischemia Reversible Ischemia No Reversible Ischemia Medical Treatment Strenuous Leisure Activity or Occupation Symptom-Limited Exercise Test at 3-6 Weeks Markedly Abnormal Cardiac Catheterization Mildly Abnormal Negative Exercise Imaging Study Reversible Ischemia Dr.Sarma@works No Reversible Ischemia No Reversible Ischemia Medical Treatment Recommendations for Hormone Replacement Therapy (HRT) After Acute MI Class IIa Recommendations 1. HRT with estrogen and progestin for secondary prevention of coronary events should not be given de novo to postmenopausal women after AMI 2. Postmenopausal women who are already taking HRT with estrogen plus progestin at the time of AMI can continue their therapy Dr.Sarma@works HERS Study: JAMA 1998;280:605-13 Initial Treatment • A = Aspirin and Antianginal therapy • B = Beta-blocker and Blood pressure • C = Cigarette smoking and Cholesterol • D = Diet and Diabetes • E = Education and Exercise Dr.Sarma@works Algorithm for the Evaluation and Management of Patients Suspected of Having an ACS. Noncardiac Diagnosis Chronic Stable Angina Treatment as indicated by alternative diagnosis See ACC/AHA/ACP Guidelines for Chronic Stable Angina No recurrent pain; Negative follow-up studies Symptoms Suggestive of ACS Possible ACS Definite ACS No ST elevation Nondiagnostic ECG Normal Initial serum cardiac markers ST and/or T wave changes Ongoing pain Positive cardiac markers Hemodynamic abnormalities Observe Stress study to provoke ischemia Follow-up at 4-8 hours; Consider evaluation of LV function if ischemia present (Test may be performed prior to discharge or as outpatient) ECG, cardiac markers Negative: Potential diagnoses: nonischemic discomfort low-risk ACS Arrangement for outpatientfollow-up Dr.Sarma@works Positive: Diagnosis of ACS confirmed ST elevation Evaluation for reperfusion therapy Recurrent ischemic pain or positive follow-up studies Diagnosis of ACS confirmed See ACC/AHA Guidelines for Acute MI Admit to hospital Manage via acute ischemia pathway III. Hospital Care A. Anti-ischemic Therapy B. Antiplatelet and Anticoagulation Therapy C. Risk Stratification D. Early Conservative vs. Invasive Strategies Dr.Sarma@works Acute Ischemic Pathway Aspirin Beta-blockers Nitrates Antithrombin regimen GP IIb/IIIa inhibitor Monitoring (rhythm and ischemia) Early Invasive strategy Immediate angiography 12-24 hour angiography Recurrent Ischemia and/or ST segment shift, or Deep T-wave Inversion, or Positive cardiac markers Early Conservative strategy Patient stabilizes Recurrent symptoms/ischemia Heart failure Serious arrhythmia Evaluate LV function EF < .40 Stress Test EF .40 Low risk Not low risk Follow on Medical Rx Dr.Sarma@works A. Anti-Ischemic Therapy Class I - Recommendations 1. Bed rest with continuous ECG monitoring for ischemia and arrhythmia detection in patients with ongoing rest pain 2. Sublingual follow by intravenous nitroglycerin (NTG) for immediate relief of ischemia and associated symptoms 3. Morphine sulfate intravenously when symptoms are not immediately relieved with NTG or when acute pulmonary congestion is present 4. A beta-blocker, with the first dose administered intravenously if there is ongoing chest pain, followed by oral administration, in the absence of contraindications Dr.Sarma@works A. Anti-Ischemic Therapy Class I - Recommendations 1. Bed rest with continuous ECG monitoring for ischemia and arrhythmia detection in patients with ongoing rest pain 2. Sublingual follow by intravenous nitroglycerin (NTG) for immediate relief of ischemia and associated symptoms 3. Morphine sulfate intravenously when symptoms are not immediately relieved with NTG or when acute pulmonary congestion is present 4. A beta-blocker, with the first dose administered intravenously if there is ongoing chest pain, followed by oral administration, in the absence of contraindications Dr.Sarma@works A. Anti-Ischemic Therapy Class I - Recommendations 1. Bed rest with continuous ECG monitoring for ischemia and arrhythmia detection in patients with ongoing rest pain 2. Sublingual follow by intravenous nitroglycerin (NTG) for immediate relief of ischemia and associated symptoms 3. Morphine sulfate intravenously when symptoms are not immediately relieved with NTG or when acute pulmonary congestion is present 4. A beta-blocker, with the first dose administered intravenously if there is ongoing chest pain, followed by oral administration, in the absence of contraindications Dr.Sarma@works B. Antiplatelet and Anticoagulation Therapy • When platelets are activated, the GP IIb-IIIa receptor undergoes a change in configuration that results in binding of fibrinogen to platelet receptors, resulting in platelet aggregation. The efficacy of GP IIb-IIIa antagonists in prevention of the complications associated with percutaneous coronary intervention (PCI) has been documented in numerous trials, many of which were composed entirely or in large part of patients with UA. Dr.Sarma@works B. Antiplatelet and Anticoagulation Therapy Class III Recommendations Intravenous Thrombolytic Therapy in Non-ST Elevation MI Dr.Sarma@works D. Early Conservative Versus Invasive Strategies Class I - Recommendations 1. An early invasive strategy is recommended in patients with UA/NSTEMI and any of the following high-risk indicators: a. Recurrent angina/ischemia at rest or with low-level activities despite intensive anti-ischemia therapy b. Elevated TnT or TnI c. New or presumed new ST-segment depression at presentation d. Recurrent angian/ischemia with CHF symptoms, an S3 gallop, pulmonary edema, worsening rales, or new or worsening mitral regurgitation. Dr.Sarma@works D. Early Conservative Versus Invasive Strategies Class I - Recommendations e. f. High-risk findings on noninvasive stress testing Depressed LV systolic function (eg.ejection fraction [EF] <0.40 on noninvasive study). g. Hemodynamic instability or angina at rest accompanied by hypotension. h. Sustained ventricular tachycardia. i. PCI within 6 months. j. Prior CABG Dr.Sarma@works IV. Coronary Revascularization Recommendations for Revascularization with PCI and CABG in Patients with UA/NSTEMI Dr.Sarma@works Recommendations for Revascularization Class I - Recommendations 1. CABG for patients with significant left main CAD 2. CABG for patients with 3-vessel CAD; the survival benefit is greatest in patients with abnormal LV function (EF <0.50) 3. CABG for patients with 2-vessel CAD with significant proximal left anterior descending CAD and wither abnormal LV function (EF <0.50) or demonstrable ischemia on noninvasive testing Dr.Sarma@works Recommendations for Revascularization Class I - Recommendations 4. PCI or CABG for patients with 1- or 2- vessel CAD without significant proximal left anterior descending CAD but with a large area of viable myocaridum and high-risk criteria on noninvasive testing 5. PCI for patients with multivessel CAD with suitable coronary anatomy, with normal LV function, and without diabetes Dr.Sarma@works Recommendations for Revascularization Class I - Recommendations 6. CABG with the internal mammary artery for patients with multivessel CAD and treated diabetes mellitus 7. Intravenous platelet GP IIb/IIIa inhibitor in UA/NSTEMI patients undergoing PCI Dr.Sarma@works Unstable Angina - Definition • angina at rest (> 20 minutes) • new-onset (< 2 months) exertional angina (at least CCSC III in severity) • recent (< 2 months) acceleration of angina (increase in severity of at least one CCSC class to at least CCSC class III) Canadian Cardiovascular Society Classification Dr.Sarma@works Agency for Health Care Policy Research - 1994 Unstable Angina pathogenesis • Plaque disruption • Acute thrombosis • Vasoconstriction Dr.Sarma@works Unstable Angina pathogenesis • Plaque disruption – Passive plaque disruption soft plaque with high concentration of cholesteryl esters and a thin fibrous cap – Active plaque disruption macrophage-rich area with enzymes that may degrade and weaken the fibrous cap; predisposing it to rupture Dr.Sarma@works Unstable Angina pathogenesis • Acute Thrombosis – Vulnerable plaque • disrupted plaque with ulceration • occurring in 2/3 of unstable patients • the exposed lipid-rich core abundant in cholesteryl ester is highly thrombogenic – Systemic Hypercoagulable State • disrupted plaque with erosion • occurring in 1/3 of unstable patients Dr.Sarma@works Unstable Angina pathogenesis • Vasoconstriction – the culprit lesion in response to deep arterial damage or plaque disruption – area of dysfunctional endothelium near the culprit lesion – platelet-dependent and thrombin-dependent vasoconstriction, mediated by serotonin and thromboxane A2 Dr.Sarma@works Acute Coronary Syndrome • Process of resolution – spontaneous thrombolysis – vasoconstriction resolution – presence of collateral circulation • Delayed or absence of resolution may lead to non-Q-wave or Q-wave myocardial infarction Dr.Sarma@works Non-Q-Wave MI clues to diagnosis • Prolonged chest pain • Associated symptoms from the autonomic nervous system – nausea, vomiting, diaphoresis • Persistent ST-segment depression after resolution of chest pain Dr.Sarma@works Prinzmetal’s Angina clues to diagnosis • Transient ST-segment elevation during chest pain • Intermittent chest pain – – – – often repetitive usually at rest typically in the early morning hours rapidly relieved by nitroglycerine • Syncope (rare), Raynaud’s, migraine Dr.Sarma@works Unstable Angina Anti-thrombotic Therapy • Thrombolytics are not indicated • “lytic agents may stimulate the thrombogenic process and result in paradoxical aggravation of ischemia and myocardial infarction” Dr.Sarma@works TIMI IIIB Investigators Circulation 1994; 89:1545-1556 Recommendations for Revascularization Class I - Recommendations • Discharge prescription details Dr.Sarma@works Fiban incidence of intracranial bleeding Study Compound Treatment (%) Placebo Active RESTORE EPIC Tirofiban Abciximab 0.3 0.3 EPILOG IMPACT II Dr.Sarma@works Abciximab Integrelin 0.0 0.07 The EXCITE Trial Investigators 0.1 0.1 0.4 0.1 0.07 0.15 Heparin Bolus Bolus + Infusion Low dose High dose Unstable Angina Anti-platelet Therapy • Summary The question is no longer “Is there a reason to use GP IIb/IIIa inhibitors?” but “Is there a reason not to use them?” Eric Topol, MD Dr.Sarma@works Unstable Angina Anti-coagulant Therapy • Heparin – recommendation is based on documented efficacy in many trials of moderate size – meta-analyses (1,2) of six trials showed a 33% risk reduction in MI and death, but with a two fold increase in major bleeding – titrate PTT to 2x the upper limits of normal Dr.Sarma@works 1. Circulation 1994;89:81-88 2. JAMA 1996;276:811-815 Unstable Angina Anti-coagulant Therapy • Low-molecular-weight heparin advantages over heparin: – better bio-availability – higher ratio (3:1) of anti-Xa to anti-IIa activity – longer anti-Xa activity, avoid rebound – induces less platelet activation – ease of use (subcutaneous - qd or bid) – no need for monitoring Dr.Sarma@works Unstable Angina Anti-coagulant Therapy • Low-molecular-weight heparin – ESSENCE Trial (Efficacy and Safety of Subcutaneous Enoxaparin in non-Q-Wave Coronary Events Study) – at 30days, there was a relative risk reduction of 15% -16% in the rate of death, MI, or refractory ischemia as compared to standard heparin Dr.Sarma@works N Eng J Med 1997;337:447-452 MITI: Mortality, Infarct Size, and Time P<0.001 P=0.04 12.0 11.2 10.0 Tx >70 minutes from onset 8.7 Percent 8.0 6.0 4.9 4.0 2.0 1.2 0.0 Mortality Adapted from Weaver WD, et al. JAMA. 1993;270:1211-1216. Dr.Sarma@works Tx <70 minutes from onset Infarct Size Importance of Door-to-Balloon Time: 30-Day Mortality in the GUSTOP=0.00 IIb Cohort 1 25 14.1 Mortality (%) 20 15 6.4 10 3.7 5 4.0 1.0 0 < 60 61-75 76-90 > 91 Door-to-Balloon Time (minutes) Berger PB, et al. Circulation. 1999;100:14-20. Dr.Sarma@works PTCA not performed Patency and Mode of Reperfusion 100 Patency Rate (%) Fibrinolysis 80 60 90-minute patency 40 PTCA at 75 minutes 20 PTCA at 120 minutes 0 0 30 ED Drug arrival administration 45 60 75 Time (minutes) Adapted from Gibson CM. Ann Intern Med. 1999;130:841-847. 90 120 150 The Four Ds ED Time Point 4: DRUG ED Time Point 3: DECISION ED Time Point 2: DATA ED Time Point 1: DOOR Time Interval III Decision to drug Time Interval II ECG to decision to treat Time Interval I Door to ECG Time of Onset NHAAP Recommendations. U.S. Department of Health NIH Publication: 1997:97-3787. Dr.Sarma@works ACC/AHA Guidelines for the Management of Patients With AMI ST-segment elevation Aspirin, beta-blocker, antithrombin 12 h Eligible for fibrinolytic therapy Fibrinolytic therapy Fibrinolytic therapy contraindicated >12 h Not a candidate for reperfusion therapy Persistent symptoms? No Primary PTCA or CABG Other medical therapy: ACE inhibitors? Nitrates Yes Consider reperfusion therapy PTCA, percutaneous transluminal coronary angioplasty; CABG, coronary artery bypass graft; ACE, angiotensin-converting enzyme. Adapted from Ryan TJ, et al. ACC/AHA 1999 Update. Dr.Sarma@works Available at http://www.acc.org/clinical/guidelines and http://www.americanheart.org. Accessed February 2000. Summary: Importance of Early Treatment • Prompt reperfusion limits myocardial necrosis, preserves left ventricular function, and reduces mortality • Achievement of early, complete reperfusion may be more feasible with fibrinolytic therapy than with primary PTCA • Maximal benefits of fibrinolytic therapy are attained within the first hour of symptom onset, although benefits extend out to 12 hours • Continued efforts are needed to minimize doorDr.Sarma@works to-drug time Myocardial Infarction Overview • Estimated 200-300,000 sudden (out-of-hospital) deaths per year in U.S. • Approximately 1 million hospitalizations per year in U.S. • Absolute number of MI events and fatality rates declining • Remains principal cause of death in Western world Acute MI Impact of Modern Critical Care on Mortality 40 30 Short-Term Mortality (%) 30 20 15 10 0 Defibrillation Hemodynamic Monitoring -Blockers Pre-CCU Era CCU Era Aspirin Thrombolysis PTCA 6.5 Reperfusion Era Adapted from Antman, Braunwald In:Braunwald ed. Heart Disease p 1184. Management of Acute MI Diagnosis Risk Stratification Acute Therapy Reperfusion Adjunctive Complications Pre-Discharge Management Diagnosis of Acute MI History • Classic symptoms: intense, oppressive chest pressure radiating to left arm • Other symptoms: chest heaviness, burning radiation to jaw, neck, shoulder, back, arms nausea, vomiting diaphoresis dyspnea lightheadedness • Symptoms may be mild or subtle Diagnosis of Acute MI Physical Examination • Tachycardia or bradycardia • Extrasystoles • S3 or S4, mitral regurgitation murmur • Lung rales • Hypertension or hypotension • Pallor, distress Diagnosis of Acute MI Electrocardiogram Defines location, extent, and prognosis of infarction • ST elevation diagnostic of coronary occlusion • Q-waves do NOT signify completed infarction • ST depression or T inversion: unlikely total coronary occlusion • ST elevation in RV4 for RV infarction • Observe up to 24 hrs for non-diagnostic ECG • Differentiate from early repolarization in V1-2 Acute MI Myocardial Enzymes CPK Troponin 20 100 % of Patients TnT >0.1 ng/ml 80 15 TNT <0.1 ng/ml 60 10 12.3 11.6 40 Occl -Reperf 20 Occl +Reperf 5 4.1 Subtot Occl 0 8-11 12-15 >16 4-7 <4 Time to Peak CK Activity (hrs) Gore et al. AJC 1987;59:1234. 0 2.3 CK-MB>7 CK-MB<7 Ohman et al. NEJM 1996;335:1333. Diagnosis of Acute MI Echocardiography • Not diagnostic, but supportive • Identify regional wall motion abnormalities • Absence of contralateral wall hyperkinesia suggests multivessel disease or IRA recanalization • Assess LV function, prior infarcts • More sensitive than ECG for RV infarction Diagnosis of Acute MI Differential Diagnosis Ischemic Heart Disease • angina, aortic stenosis, hypertrophic CMP Nonischemic Cardiovascular Disease • pericarditis, aortic dissection Gastrointestinal • esophageal spasm, gastritis, PUD, pancreatitis, cholecystitis Pulmonary • pulmonary embolism, pneumothorax, pleurisy Diagnosis of Acute MI Coronary Angiography • May be necessary for equivocal symptoms and ECG e.g. patients with prior CABG, previous MI, myocarditis with diffuse ECG D’s, noncharacteristic D’s on ECG • Finding of acutely-occluded vessel diagnostic • Allows mechanical reperfusion Acute MI Coronary Angiography • Incorporated in primary, rescue PTCA strategies • If ischemia, spontaneous or exerciseinduced or complicated (CHF, arrhythmia) • Controversial if uncomplicated MI • Delineates anatomy but may potentiate unneeded revascularization • Very low risk but appreciable cost • Key prognostic indicator Management of Acute MI Diagnosis Risk Stratification Acute Therapy Reperfusion Adjunctive Complications Pre-Discharge Management Acute MI - Risk Stratification The GUSTO Pyramid - 30 Day Mortality Model HX CV Disease (0.4%) HTN (0.6%) Prior CABG (0.8%) Accel t-PA (0.8%) Smoker (0.8%)Weight (0.8%) Diabetes (1%)Time-to-Rx (1%) Age x Killip (1.3%) Height (1.1%) MI Location (6%) Prior MI (3%) Heart Rate (12%) Killip Class (15%) Systolic Blood Pressure (24%) Age (31%) Lee et al. Circulation 1995;91:1659-1668 Acute MI - Risk Stratification ECG Classification - GUSTO I Outcome Category Occlusion Site ECG 1-Year Mortality 1. Prox LAD before septal ST V1-6, I, aVL 25.6% fasicular or BBB 2. Mid LAD before diagonal ST V1-6, I, aVL 12.4% 3. Distal LAD Diagonal beyond diagonal in diagonal ST V1-4 or 10.2% ST I, aVL, V5-6 4. Moderate-to- proximal RCA large inferior or LCX (post, lat, RV) ST II, III, aVF and 8.4% V1, V3R, V4R or V5-6 or R > S V1-2 5. Small inferior ST II, III, aVF only6.7% distal RCA or LCX branch Acute MI - Risk Stratification Ejection Fraction 50% Mortality (2-Year) 40% 30% 20% 10% 0 20 30 40 50 60 Ejection Fraction (%) Gottlieb et al. Am J Cardiol 1992;69:977-984 70 Acute MI - Risk Stratification Hemodynamic Subgroups - Killip Class GISSI-1 (%) Killip Definition Incidence Control I No CHF 71 7.3 5.9 II S3 gallop or basilar rales 23 19.9 16.1 III Pulmonary edema (rales >1/2 up) 4 39.0 33.0 IV Cardiogenic shock 2 70.1 69.9 Class tality Lytic MortalityMor Management of Acute MI Diagnosis Risk Stratification Acute Therapy Reperfusion Adjunctive Complications Pre-Discharge Management Aspirin in Acute MI ISIS-2 20 35 Day Mortality (%) 15 13.2 10 10.7 10.4 8 5 0 4300 4295 4300 4292 Placebo ASA SK SK + ASA ISIS-2 Collaborative Group, Lancet 1988;2:349. Aspirin in Acute MI Recommendations • Indicated in ALL patients with acute MI, except for true aspirin allergy (not intolerance) • Initiate orally with chewable compound, at least 160 mg stat some data suggest first dose should be 650 mg to achieve full antiplatelet effect Heparin for Acute MI? Death HeparinAllocated ControlAllocated Odds Ratio & 95% C.I. t-PA (4.3%) 17/476 (3.6%) 20/468 SK/APSAC (7.2%) 28/402 (7.0%) 28/389 Aspirin (4.8%) 30/622 (4.8%) 29/609 0.36 No Aspirin 15/256 (5.9%) 20/248 114/476 (23.9%) 83/468 0.43 (8.1%) Any Bleeding t-PA (17.7%) SK/APSAC (14.4%) 0.5 85/402 (21.1%) 56/389 1.0 1.5 2.0 2.5 Heparin Better Control Better Mahaffey, et al. AJC 77:551–6, 1996 T-PA and Heparin 100 80 Patency (%) Heparin 79 79 No Heparin 83 82 75 71 60 80 80 52 40 44 20 0 Angio TAMI-3 90 min +ASA HART 18 hrs +ASA Bleich 40 hrs +ASA ECSG-6 NHF 80 hrs 7 days +ASA +ASA Topol EJ, Textbook Intervent Cardiol, 2nd Ed, 1993, p. 83. Acute MI Heparin • Intravenous heparin recommended with tPA (intial bolus 5000 U, infusion 1000 U/hr, adjust for weight < 50 kg) • No clear data for benefit with streptokinase and increased bleeding • Discontinue after 24 hrs, except for: atrial fibrillation recurrent ischemia anteroapical MI for CVA prophylaxis Acute MI IV Heparin • Optimal aPTT appears to be 50 to 70 seconds • Not indicated with streptokinase GISSI-2/Int’l and ISIS-3 SK+ASA=SK+ASA+SQ hep GUSTO-I SK+IV hep = SK+SQ hep • Risk (at higher levels) of ICB GUSTO-II Adjunctive Therapy for Acute MI Beta Blockers (Prior to Thrombolytic Era) Pooled Analysis - 7 Day Outcome 5 4 3 % of Patients p<0.02 4.2 3.6 > 29,000 Patients (26 Trials) Beta Blocker p<0.02 3.4 2.8 2 1 0 Placebo p<0.05 2.2 2.6 -13% -20% -15% Death Reinfarction Arrest (VF) Held et al, in Topol: Text Int Cardiol 2nd Ed 1993, p.47. TIMI 2 Immediate vs Deferred Metoprolol 30 % of Patients % of Patients 2 Immediate 20 1.5 Delayed p<0.01 21 15 10 p<0.02 2 0 4 Reinfarction Recurrent Ischemia 1.4 1 p<0.03 0.5 0 0.28 IC Hemorrhage 48% of patients eligible for randomization to beta blocker 10% discontinued due to hypotension or bradycardia TIMI Study Group. N Engl J Med 1989;320:618. Beta Blockers in Acute MI Pooled Analysis of Randomized Trials Mortality Odds Ratio & 95% CI Study Agent ISIS-1 Atenolol 16,027 During MI MIAMI Metoprolol5,778 TIMI IIB Post MI Metoprolol1,434 Norwegian Timolol BHAT N 1,884 3,837 Propranolol 0 Rx Better Hennekens et al. NEJM 1996;335:1660. 1 Control Better 2 Beta Blockers in Acute MI Recommendations • IV to oral beta blocker therapy in patients without contraindications in first 24 hours • Avoid early therapy in patients with bradycardia, hypotension, inferior MI, CHF, impaired LV function, AV block, asthma • Continue treatment for at least 2-3 years Adjunctive Therapy for Acute MI ACE Inhibitors Outcome in “Megatrials” 15 % Mortality (4-6 Weeks) ACE-I 10 0 Mortality Reduction = 5 lives/1000 Rx’d p=0.57 Control p=0.02 5 Total 85,064 Patients 6.87 7.33 p=0.03 6.33 9.39 9.72 7.11 27,442 27,382 9435 9460 5666 5679 ISIS-4 GISSI-3 Chinese ACE Inhibitors in Acute MI Pooled Analysis of Randomized Trials Study Agent ISIS-4 Captopril 58,050 Mortality Odds Ratio & 95% CI N During GISSI-3 Lisinopril 19,394 MI CONSEN II Enalaprilat6,090 Post MI SAVE Captopril 2,231 AIRE Ramipril TRACE 1,749 Trandolapril 2,006 0 Rx Better Hennekens et al. NEJM 1996;335:1660. 1 Control Better 2 Adjunctive Therapy for Acute MI Magnesium LIMIT-2 ISIS-4 % Mortality (28 Day) 15 % Mortality (35 Day) 15 p < 0.05 10 p = NS 10.20 10 7.80 5 5 0 0 Mg Placebo Woods et al. Lancet 1992;339:1553. 7.28 6.92 Mg Placebo ISIS-4 Collab Group Lancet 1995;345:669. Magnesium in Acute MI Summary • Mortality benefit of empiric Rx - conflicting results of randomized trials possibly due to late administration and low mortality in the ISIS-4 trial • Correct low serum [Mg+2] • Magnesium 1-2 gm bolus over 5 minutes may be definitive Rx for Torsade de Pointes or polymorphic ventricular tachycardia Adjunctive Therapy for Acute MI Calcium Channel Antagonists Agent N Odds Ratio & 95% CI Nifedipine 1358 Verapamil 1775 Diltiazem 2466 Verapamil/ 4241 Diltiazem Pooled Ca+2Ant Control 5599 0 Less Mortality 1 More Mortality 15.0% 13.0% 10.8% 13.3% 13.5% 13.5% 12.4% 13.4% 13.0% 13.3% 2 Held et al, in Topol: Text Int Cardiol 2nd Ed 1993, p.52. Management of Acute MI Diagnosis Risk Stratification Acute Therapy Reperfusion Adjunctive Complications Pre-Discharge Management Complications of Acute MI Extension / Ischemia Expansion / Aneurysm Mechanical Arrhythmia Pericarditis Acute MI Heart Failure RV Infarct Mural Thrombus Management of Acute MI Intra-Aortic Balloon Pump Counterpulsation Decreases systemic afterload Increases diastolic aortic pressure Reduces myocardial oxygen demand Improves systemic / end-organ perfusion Variable effects on coronary perfusion IABP in Acute MI Indications Cardiogenic shock not quickly reversed (indication less firm for hemodynamic instability without shock) Acute MR or VSD Refractory myocardial ischemia Refractory ventricular arrhythmias Useful as a bridge to revascularization and for support during recovery of extensive “stunned myocardium” Management of Acute MI Indications for Invasive Hemodynamic Monitoring Right Heart Catheterization (Swan-Ganz Catheter) Severe or progressive CHF or pulmonary edema VSD or papillary muscle rupture Cardiogenic shock or progressive hypotension Hypotension unresponsive to fluid Rx Need for inotropic or IABP support RV infarction Refractory VT Acute MI - Recurrent Infarction / Ischemia Pathophysiology • In distribution of infarct vessel: IRA reperfusion, then reocclusion thrombus propogation, branch occlusion distal embolization reduced coronary perfusion pressure with severe residual IRA stenosis reduced collateral flow from stenosed artery • At a distance: reduced collateral flow from IRA new coronary thrombus (hypercoagulable state) reduced systemic perfusion pressure increased myocardial oxygen consumption Acute MI - Complications Recurrent Ischemia / Infarction • Prevention: Aspirin Beta blockers ACE inhibitors with low LVEF ? heparin with fibrin-specific lytics (reocclusion) • Treatment: Pharmacologic (beta blockers, nitrates) IABP Urgent revascularization Repeat lytics (antibodies to SK) Acute MI - CHF and Shock Pathophysiology • Extensive (or multiple) LV infarction(s) - systolic dysfunction • Impaired relaxation, compliance due to infarction or ischemia - diastolic dysfunction • Extensive RV infarction or ischemia • VSD or acute severe MR • Tamponade (w/ or w/o free wall rupture) • Others e.g. critical valve stenosis or regurgitation, toxicmetabolic, sepsis, beta- or Ca+2-blocker overdose, pulmonary embolism, bowel ischemia Acute MI - CHF and Shock Hemodynamic Subsets Subset PCWP CI (mm Hg) (l/min) Clinical Setting 1 < 18 > 2.2 asymptomatic 2 congestion > 18 > 2.2 pulmonary 3 < 18 < 2.2 4 > 18 < 2.2 RV failure, hypovolemia, or profound venodilation severe LV dysfxn cardiogenic shock Forrester JS et al. NEJM 1976;295:1356 and 1404. Acute MI - Cardiogenic Shock Outcome with PTCA Pooled Analysis of 22 Retrospective Studies 100 Mortality (%) 80 81 • Historical control mortality ~ 80% • Total 646 pts • PTCA success rate = 76% 60 40 45 33 20 0 Total Successful Unsuccessful PTCA PTCA Hochman, Gersh in Topol, Text Cardiovasc Med 1998, p. 461. Acute MI - Mechanical Complications Free Wall Rupture • Less frequent (1-3.4%), but earlier, with thrombolysis • Uncontained sudden EMD or asystole • Pseudoaneurysm transient hypotension, EMD, bradycardia, repetitive emesis, restlessness • Echocardiogram usually diagnostic • Surgical repair - may require pericardiocentesis for uncontained rupture Acute MI - Mechanical Complications Interventricular Septal Rupture • Incidence 1-3% of transmural MIs • Acute shock, pulmonary edema, right heart failure, new loud pan-systolic murmur (thrill in 50%) • Diagnose with echocardiogram or O2 saturation step-up • Medical stabilization and IABP for CHF, shock • Early surgical repair for decompensated pts; mortality highest in pts with inferior MI and complex ruptures involving RV (~70%), lowest for apical ruptures (~30%) Acute MI - Complications Infarct Expansion • Potential consequences: LV aneurysm +/- mural thrombus +/embolization adverse LV remodeling and CHF ventricular rupture ventricular arrhythmias • Prevention: ACE inhibitors ? nitrates the “open artery” Acute MI The “Late Open Artery” n Patent Up Time to FollowOccluded Angio (days) (months) IRA IRA Mortality Mortal ity Cigarroa 179 1-150 47 0% 18% Gohike 102 < 365 51 13% 17% Galvani 172 10 43 1% 17% White 305 28 39 5% 10% Lamas 946 4 42 14% 24% Welty Hochman, Gersh in Topol, Text Cardiovasc Med 1998, p. 445. 479 < 90 34 4% 17% Acute MI - Mechanical Complications Acute Mitral Regurgitation • Transient MR common in early MI (20-40%) • Associated with advanced age, prior MI, infarct extension, recurrent chest pain, CHF, female gender • Persistent MR, even mild, associated with increased long-term mortality post-MI • May be due to papillary muscle or chordal rupture or to geometric changes (dilation) of ventricle and annulus • Most common with inferior MI (single blood supply to posteromedial papillary muscle) - MI often small Acute Mitral Regurgitation Diagnosis and Management harsh, short systolic murmur - may be muffled sudden CHF +/- hypotension or shock 2-7 days post MI echocardiography (surface or TEE) usually diagnostic - mobile papillary muscle head or flail MV leaflet LV function often normal or hyperkinetic sudden hemodynamic deterioration common stabilize medically, IABP, then surgical repair surgical mortality high if shock is present Acute MI - Complications Right Ventricular Infarction • Associated with occlusion of proximal RCA • Classic triad by hypotension, JVP, clear lungs specific but insensitive • Kussmaul’s sign, JVP > 8 cm H2O sensitive and specific • EKG: ST in RV4 • Echo: RV dilation and hypokinesia • PA catheter: RA >10 mm, RA/PCWP ratio > 0.8 Acute MI - RV Infarction Management • Extensive irreversible infarction is unusual transient ischemic dysfunction with long-term recovery common • Marked by sensitivity to preload reduction (nitrates, diuretics, morphine), bradycardia, AV block • Fluid volume infusion for hypotension and low cardiac output • PCWP elevation may occur due to septal shift • Dobutamine if fluids RA and PCWP without Acute MI - Arrhythmias Prophylactic Lidocaine • Prophylactic use for suppression of VT or VF controversial • Overview of randomized trials: 33% reduction in primary ventricular arrhythmias trend toward 38% increased mortality (asystole) • Potential benefit in reperfusion era - GUSTO I (but not a randomized comparison) • Should likely avoid unless VT / VF or non-sustained VT occurs Acute MI - Antiarrhythmic Agents Pooled Analysis of Randomized Trials Study Agent CAST Enc / Flec 1,498 Class CAST II I Moricizine 1,325 EMIAT Amiodarone1,486 CAMIAT 1,202 Amiodarone Class III SWORD Mortality Odds Ratio & 95% CI N d-Sotalol 3,121 Julian et al l-Sotalol 1,456 0.1 Rx Better 1 Control Better NEJM 1996;335:1660. Lancet 1997;349:667 and 675. 10 Acute MI - Arrhythmias Ventricular Tachycardia or Fibrillation • Prognosis of VT or VF in first 48 hours controversial MILIS - no increased in-hospital mortality GISSI - increased in-hospital mortality No increased mortality after hospital discharge • VT or VF after first 48 hours associated with poorer long-term prognosis • Acute management - K+ replacement, antiarrhythmic therapy (lidocaine, procainamide, or amiodarone) if stable, electrical shock if unstable Acute MI - Arrhythmias Atrial Fibrillation • Incidence reduced with thrombolysis (<5%) • Associated with large MI (especially if sustained) • Prognostic of adverse events over following year • Rate control with digoxin, or (without CHF) beta blockers, verapamil, or diltiazem • Consider IV amiodarone • Electrical cardioversion for hemodynamic compromise or ischemia Acute MI - Arrhythmias Indications for Temporary Pacing asystole complete (third-degree) AV block second-degree Mobitz II AV block second-degree Mobitz I AV block with hypotension new bifascicular block, esp with first-degree AV block symptomatic bradycardia, unresponsive to atropine Acute MI - Arrhythmias Indications for Permanent Pacing persistent complete (third-degree) AV block persistent sinus node dysfunction symptomatic bradycardia intermittent second-degree Mobitz II or thirddegree AV block second-degree Mobitz II or third-degree AV block with new bundle branch block Management of Acute MI Diagnosis Risk Stratification Acute Therapy Reperfusion Adjunctive Complications Pre-Discharge Management Acute MI Pre-Discharge Management • Risk stratification • Catheterization and revascularization strategy • Electrophysiologic evaluation for VT or VF • Lifestyle modification: diet, exercise, tobacco • Pharmacologic therapy Acute MI - Risk Stratification Post-MI Revascularization Strategy Low Risk High Risk* LVSF Nl LVSF Stress Imaging LVSF Nl LVSF Stress Imaging or Catheterization Normal Angiography ± Revascularization Direct Cath * (Re) MI or CP, VT, CHF, Prior MI, Prior Revascularization Acute MI Management Pharmacologic Therapy on Hospital Discharge Aspirin indefinitely (ticlopidine or clopidogrel for aspirin allergy or intolerance) Beta blockers for at least 2-3 years ACE inhibitors for CHF, LVEF<40%, or large infarction (even with preserved LVEF) Lipid lowering agents Coumadin for mural thrombus, extensive anterior infarct, DVT, atrial fibrillation Thrombolysis in Acute MI Relative Contraindications Uncontrolled HTN (BP > 180/110) on presentation History prior CVA beyond 1 yr Anticoagulant Rx with INR > 2-3; bleeding diathesis Recent trauma (within 2-4 wks) Noncompressible vascular punctures Recent internal bleeding (within 2-4 wks) Pregnancy Active peptic ulcer Prior exposure (5 day - 2 yr) for SK or APSAC Thrombolysis in Acute MI Absolute Contraindications Previous hemorrhagic stroke CVA within previous yr Intracranial neoplasia or AVM Active internal bleeding (not menses) Suspected aortic dissection Myocardial Reperfusion The Original Paradigm Re-establish Infarct Vessel Patency Limit Infarct Size Mortality GUSTO 8 Mortality Trial Angiographic Trial 41,021 Patients 30-day Outcome 2,431 Patients TIMI 3 flow % Mortality 60 50 6 4 2 0 % of Patients 54 40 SK (IV) SK (SubQ) t-PA +SK Accel.t-PA 0 2 4 6 8 1012141618202224262830 Days from Randomization 30 20 29 33 38 10 0 SK+SQ SK+IV Accel. t-PA+ Hep Hep t-PA SK Thrombolytic: Placebo-Control Meta-Analysis Agent Ratio s.d.) Streptokinase Trial Name Reduction Deaths/Patients Active 495/4865 GISSI 23% ± 6 ISAM 50/842 16% ± 18 ISIS-2 471/5350 30% ± 5 Control 623/4878 Odds Odds (& 95% Cl) (± 61/868 648/5360 APSAC AIMS 50% ± 16 32/502 61/502 t-PA ASSET 28% ± 9 182/2516 245/2495 0.0 0.5 1.0 1.5 2.0 Lytic better Lytic worse Overall: any thrombolytic 1230/14075 1623/14103 Thrombolysis for Acute MI Time to Therapy and Mortality Reduction Pooled Analysis of Randomized Trials Absolute Mortality Reduction per 1000 Patients 40 30 20 10 0 0 6 12 18 24 Time from Symptom Onset to Randomization (h) Fibrinolytic Therapy Trialists. Lancet 1994;343:311. New Fibrinolytics ASSENT II 8 30 Day Outcom e (%) 8 7 t-PA 6 TNK 6.15 6.17 INTIME II 6 5 4 4 3 3 2 2 1 1 0 Mortality ICH t-PA 7 5 0.94 0.93 30 Day Outcom e (%) 0 6.6 6.77 TNK p=0.003 1.13 Mortality 0.62 ICH Thrombolysis for Acute MI Electrocardiographic Criteria for Therapy Pooled Analysis of Randomized Trials EKG Odds Ratio & 95% CI Placebo Lysis BBB 23.6% 18.7% ST Anterior 16.9% 13.2% 8.4% 7.5% 13.4% 10.6% 13.8% 15.2% 5.8% 5.2% 2.3% 3.0% ST Inferior ST Other ST Other Abnorm Normal 0.33 Lysis Better 1 Placebo Better 3 Fibrinolytic Therapy Trialists. Lancet 1994;343:311. Thrombolysis and Age 40 GISSI -1 and ISIS -2 GUSTO 1 N = 28,896 Patients N = 41,021 Patients % Mortality Placebo 30 20 10 Streptokinase 14% RR D = 2.4% 26% RR D = 1.2% 7.7 0 14% RR D = 3.9% 28.8 40 SK 30 Accel t-PA 6% RR D =1.3% 24.9 20 17.6 15.2 10 21.5 20.2 17% RR D = 1.0% 6.0 5.5 <65 % Death or Disabling Stroke 65-74 Age (yrs) 75+ 0 5.0 <=75 >75 Age (yrs) Acute MI PTCA vs Lysis Death + MI (%) 20 Thrombolysis PTCA 15 10 5 p<0.0001 0 0 11 RCTs (2725 patients) 4 2 Months from Randomization 6 PCAT Collaborative Group, 2001 Primary Angioplasty in Acute MI Pooled Analysis of Randomized Trials Trial SK Trials t-PA Trials Accel t-PA Trials N Odds Ratio & 95% CI Zijlstra 389 Ribeiro 100 Grinfeld 112 DeWood 90 395 PAMI Gibbons 103 Ribichini 83 Elizaga 189 GUSTO II1138 Pooled 2599 0.1 PTCA Lysis Pooled 32% RR PTCA Better 1 Lysis Better 2.0% 7.4% 6.0% 2.0% 9.3% 10.3% 6.5% 4.5% 2.6% 6.5% 4.3% 3.6% 0.0% 2.4% 3.2% 10.6% 5.7% 7.0% 4.4% 6.5% 10 Topol, Van de Werf. Textbook Cardiovasc Med 1998;p416 Acute MI: 1995 RESCUE 156 pts < 8 hours chest pain, ant. MI with occluded LAD PTCA successful in 92% of patients Outcomes at 30 Days 20 % of Patients 50 Control 16 40 16.6 Rescue 12 8 4 0 % 39 38 40 43 30 9.6 20 7.0 5.1 Death 6.4 1.3 Severe CHF Death or CHF 10 0 Rest EF Exercise EF Pathophysiology of Combination Therapy in AMI Combination Therapy Thrombus % Stenosis Minimum Diameter Epicardial Flow Reduces Reinfarction* Myocardial Blush ST Resolution Facilitates PCI *Gibson et al. J Am Coll Cardiol. 1995;25:582-589. Gibson et al. Circulation. 2001;103:2550-2554. Myocardial Flow Recent Clinical Trials Trial GUSTO-V Lytic GP IIb/IIIa Receptor Inhibitor Anticoagulant 100% r-PA 50% r-PA None Abciximab Standard-dose heparin Low-dose heparin ASSENT-3 100% TNK-tPA 50% TNK-tPA 100% TNK-tPA None Abciximab None ACC/AHA heparin dose Low-dose heparin Enoxaparin ENTIRE Abciximab Abciximab None None Unfractionated heparin Enoxaparin Unfractionated heparin Enoxaparin 50% TNK-tPA 50% TNK-tPA 100% TNK-tPA 100% TNK-tPA Clinical Trials: Ongoing Trial Lytic GP IIb/IIIa Receptor Inhibitor Anticoagulant FASTER 50% TNK-tPA 75% TNK-tPA 100% TNK-tPA Tirofiban Tirofiban Tirofiban Low-dose heparin Low-dose heparin Low-dose heparin INTEGRITI 50% TNK-tPA 75% TNK-tPA 100% TNK-tPA Eptifibatide Eptifibatide Eptifibatide Low-dose heparin Low-dose heparin Low-dose heparin GUSTO-I: A 20% Increase in TIMI Grade 3 Flow is Needed to Yield a 1% Mortality Reduction % TIMI Grade 3 Flow 60 54% 50 t-PA 6.3% 40 32% 30 20 SK 7.4% 10 0 t-PA SK 5 6 The GUSTO Angiographic Investigators. N Engl J Med. 1993;329:1615-1622. 7 8 % Patients With TIMI Grade 3 Flow TIMI Grade 3 Flow – Pooled Data From Dose Confirmation Phases of Recent Trials 100 Lytic alone Combination 78 80 73 70 73 64 60 54 56 54 56 47 40 40 20 0 292 GUSTO-I 90 min 63 58 87 88 T14 t-PA 90 min T14 r-PA 90 min 98 100 81 75 329 321 SPEED INTRO-AMI Pooled 60-90 min 60 min 60-90 min SPEED: Results of Dose-Confirmation Phase 100 TIMI-2 TIMI-3 Patency (%) 80 28.7 21.6 60 54.9 40 47.5 20 n=109 n=115 r-PA 10+10 U r-PA 5+5 U + Abx 0 The SPEED Study Group. Circulation. 2000;101:2788-2794. • There was a 7.4% improvement in the rate of TIMI Grade 3 flow • If a 20% improvement is required to improve mortality by 1%, then a 7.4% improvement would be predicted to improve mortality by 0.3% GUSTO-V: Study Design ST , lytic eligible, < 6 h (n=16,588) ASA No Abciximab Abciximab 2 x 10 U bolus (30’) Full-dose r-PA 2 x 5 U bolus (30’) Half-dose r-PA Standard Heparin: Low-dose Heparin: 5000 U bolus followed by 800 U/h (< 80 kg) or 1000 U/h ( 80 kg) infusion 60 U/kg bolus followed by 7 U/kg/h infusion 1º end point: mortality at 30 days 2º end point: clinical and safety events at 30 days The GUSTO-V Investigators. Lancet. 2001;357:1905-1914. Primary End Point: 30-Day Mortality % Mortality 6 5.9% 5.6% 4 P=.43 for superiority Non-Inferiority RR 0.95 (95% CI, 0.84-1.08) 2 Std. Reteplase (n = 8260) Abx + Dose Reteplase (n = 8328) 0 0 5 10 15 20 Days The GUSTO-V Investigators. Lancet. 2001;357:1905-1914. 25 30 GUSTO-V: Noninferiority Analysis Upper Boundary of 95% CI for Noninferiority 1.11 OR and 95% CI Non-Inferiority RR 0.95 (95% CI, 0.84-1.08) 0.0 1.0 Abciximab + Half-dose r-PA superior Full-dose r-PA superior Adapted with permission from the GUSTO-V Investigators. Lancet. 2001;357:1905-1914. 2.0 A Comparison of the Outcomes With r-PA Monotherapy in GUSTO-III vs GUSTO-V Trials 8 P<.001 7.4% 50 1.0 48% 0.9 7 5.9% 6 40 37% 0.91% 0.8 0.7 5 30 0.59% 0.6 4 0.5 20 3 0.4 0.3 2 10 0.2 1 0 P=.015 0.1 10,138 8,260 GUSTO III GUSTO V Death 0 10,138 8,260 GUSTO III GUSTO V Anterior MI The GUSTO-III Investigators. N Engl J Med. 1997;337:1118-1123. The GUSTO-V Investigators. Lancet. 2001;357:1905-1914. 0 10,138 8,260 GUSTO III GUSTO V ICH GUSTO-V: Causes of Reinfarction Myocardial Infarction (%) 4 P<.0001 3.5 r-PA r-PA + Abx 3 2.7 2.3 2 1.7 1.6 1.2 1 0.5 0.2 0 Any Q-wave *Unblinded, unadjudicated The GUSTO-V Investigators. Lancet. 2001;357:1905-1914. Enzymatic Ischemic ST Change* Non-Intracranial Bleeding Through Discharge/Day 7 30 % of Patients 25 24.6 r-PA r-PA + Abx 20.0 20 15 13.7 11.4 10 5.7 10 4.0 3.5 0.5 1.1 1.8 0 Severe Bleeding Moderate Bleeding Mild Bleeding The GUSTO-V Investigators. Lancet. 2001;357:1905-1914. Any Bleeding Receiving Transfusions ICH by Age Group % of Patients 3 r-PA (n=8260) r-PA + Abx (n=8328) P=.069* 2.1 2 P=.53 1.5 1.2 1 P=.27* P=.66 0.4 0 1.1 0.5 0.3 0.4 24/6230 21/6193 25/2030 31/2135 37/7172 28/7179 12/1088 24/1149 70 yrs > 70 yrs 75 yrs > 75 yrs *Significant treatment interaction for the age 75 dichotomy; P=.033. The GUSTO-V Investigators. Lancet. 2001;357:1905-1914. GUSTO-V: PCI Within 6 Hours (Urgent) and Through Day 7 * 27.9 30 * 25.4 25 PCI (%) 20 Urgent Through Day 7 15 10 * 8.6 * 5.6 5 0 r-PA r-PA + Abx *P<.0001. The GUSTO-V Investigators. Lancet. 2001;357:1905-1914. GUSTO-V: Event Rates in Those Requiring Urgent PCI Myocardial Infarction (%) 12 10 r-PA r-PA + Abx n=1173 9.6 9.0 8 6.7 6 5.4 4.8 4 2.8 2 0 Death Repeat MI Death Plus Repeat MI Heartwire News. September 2, 2001. GUSTO-V: Combination half-dose fibrinolytic plus IIb/IIIa blocker. An Alternative approach to MI? GUSTO-V: Conclusions • Compared with r-PA monotherapy, combination therapy with r-PA and abciximab resulted in – A mortality rate that was not inferior to r-PA monotherapy – Fewer nonfatal reinfarctions (primarily a reduced incidence of recurrent ST elevation) – A lower rate of urgent revascularization – More noncerebral bleeding complications, transfusions, and thrombocytopenia – A higher rate of ICH in elderly patients over the age of ASSENT-3: Rationale for Use of Enoxaparin • TNK-tPA plus enoxaparin – Favorable effects of LMWHs in recent small-scale thrombolysis trials – Higher late patency: HART-2 ASSENT-Plus AMI-SK – Less reocclusion: HART-2 – Fewer reinfarctions: ASSENT-Plus AMI-SK Wilson, et al. • ASSENT-3 is the first large-scale trial to test LMWH ASSENT-3: Study Design ST-Segment Elevation AMI (n=6095 patients) 150 to 325 mg ASA (daily) Randomized Full-dose TNK-tPA Plus Enoxaparin Half-dose TNK-tPA Full-dose TNK-tPA Plus Abciximab Plus WeightPlus Low-dose Heparin adjusted UFH The ASSENT-3 Investigators. Lancet. 2001;358:605-613. ASSENT-3: Primary End Points • Primary Efficacy End Point: Composite of 30-day mortality or in-hospital reinfarction or in-hospital refractory ischemia. • Primary Efficacy Plus Safety End Point: Composite of 30day mortality or in-hospital reinfarction or in-hospital refractory ischemia plus in-hospital intracranial haemorrhage or in-hospital major bleeding other than intracranial. % Risk of 30-Day D/MI/Ref Isch ASSENT-3: 30-Day Mortality, Recurrent MI, Refractory Ischemia 3-way P=.0001 20 P=.0009* P=.0002* 15.4 15 11.4 11.1 TNK-tPA + Enox TNK-tPA + Abx 10 5 0 TNK-tPA + UFH *P-values are the Bonferroni P-values after correcting for multiple comparisons. The uncorrected P-values were P=.0002 for the enox vs UFH comparison, and P<.0001 for the abx vs UFH comparison. ASSENT-3: 30-Day Mortality, Recurrent MI, Refractory Ischemia, Major Bleeding and ICH 3-way P=.0062 % Risk of 30-Day D/MI/ Ref Isch/Maj Bleed/ICH 20 P=.0146* P=.0057* 15 13.8 14.2 TNK-tPA + Enox TNK-tPA + Abx 17.0 10 5 0 TNK-tPA + UFH *P-values are the Bonferroni P-values after correcting for multiple comparisons. The uncorrected P-values were P=.0037 for the enox vs UFH comparison, and P=.0142 for the abx vs UFH comparison. Kaplan-Meier Curves Primary Efficacy End Point 20 18 18 14 Enox* 12 Abx* 10 UFH 16 Probability (%) Probability (%) 20 UFH 16 Primary Efficacy Plus Safety End Point 8 6 4 Abx 14 Enox* 12 10 8 6 4 log-rank P=.0001 *vs UFH 2 0 log-rank P=.0062 *vs UFH + Abx 2 0 0 5 10 15 20 25 Days to death, reinfarction, or refractory ischemia 30 0 5 10 15 20 25 30 Days to death, reinfarction, refractory ischemia, ICH, or major bleeding Reprinted with permission from the ASSENT-3 Investigators. Lancet. 2001;358:605-613. ASSENT-3: Primary Efficacy and Safety End Point of Death, Reinfarction or Refractory Ischemia, ICH or Major Bleeding in Patients >75 Years of Age % Risk of 30-Day Efficacy and Safety End Point 45 P=.001* 40 36.9 35 30 28.0 25.5 25 20 15 10 5 0 TNK-tPA + Enox TNK-tPA + Abx TNK-tPA + UFH *There was a statistically significant interaction between treatment with abciximab and age such that patients over the age of 75 had poorer outcomes with abciximab (P=.001). ASSENT-3: Primary Efficacy and Safety End Point of Death, Reinfarction or Refractory Ischemia, ICH or Major Bleeding in Patients with Diabetes % Risk of 30-Day Efficacy and Safety End Point 30 P=.007* 25 22.3 20 16.5 15 13.9 10 5 0 TNK-tPA + Enox TNK-tPA + Abx TNK-tPA + UFH *There was a statistically significant interaction between treatment with abciximab and diabetes, such that diabetics had poorer outcomes with abciximab therapy (P=.0007). ASSENT-3: 30-Day Mortality % Risk of 30-Day Mortality 10 3-way P=.25 8 6.6 6 6.0 5.4 4 2 0 TNK-tPA + Enox TNK-tPA + Abx TNK-tPA + UFH ASSENT-3: 30-Day Death or MI % Risk of 30-Day Death or MI 10 3-way P=.0198 8 6.8 9.1 7.3 6 4 2 0 TNK-tPA + Enox TNK-tPA + Abx TNK-tPA + UFH ASSENT-3: In-Hospital Recurrent MI 5 3-way P=.0009 % Risk of In-Hospital Recurrent MI 4.2 4 3 2.7 2.2 2 1 0 TNK-tPA + Enox TNK-tPA + Abx TNK-tPA + UFH ASSENT-3: In-Hospital Refractory Ischemia % Risk of 30-Day Refractory Ischemia 10 3-way P<.0001 8 6.5 6 4.6 4 3.2 2 0 TNK-tPA + Enox TNK-tPA + Abx TNK-tPA + UFH ASSENT-3: Incidence of In-Hospital Thrombocytopenia and Noncerebral Bleeding Complications Enox (n=2040) Any thrombocytopenia Thrombocytopenia <20,000 cells/µL 20,000 to 50,000 cells/µL 50,000 to <100,000 cells/µL Abx (n=2017) 1.2 3.2 UFH (n=2038) 1.3 P-Value 3-way <.0001 <.0001 0.1 0.2 0.9 0.5 0.6 2.0 0.2 0.2 1.0 Bleeding episodes Total Major Minor 25.6* 3.0* 22.6* 39.7 4.3 35.4 21.1 2.2 18.8 <.0001 .0005 <.0001 Blood transfusion 3.4* 4.2 2.3 .0032 *While 3-way P-value is significant, Enox vs UFH comparison P=NS ASSENT-3: In-Hospital Stroke Rates Enox Abx UFH (n=2040) (n=2017) (n=2038) P-Value Total strokes 1.62 1.49 1.52 0.94 Intracranial hemorrhage 0.88 0.94 0.93 0.98 Ischemic stroke* 0.64 0.40 0.54 0.57 Hemorrhagic conversion 0.07 0.07 0.00 0.77 Unclassified 0.15 0.05 0.59 *Including hemorrhagic conversion 0.15 Patients Undergoing PCI: Mortality 8 ASSENT-3: In-Hospital PCI GUSTO-V: Urgent PCI 7 6.7 Mortality (%) 6 5.4 5 4 3 3.7 2.7 2.5 2 1 0 TNK-tPA + Enox TNK-tPA + Abx TNK-tPA + UFH r-PA + UFH r-PA + Abx How Does Actual Weight Compare to Estimated Weight? Correlation Between Estimated and Actual Patient Weight in TIMI 10B Actual Patient Weight (kg) 188.5 R2=0.93, P<.0001 40.5 36.4 Estimated Patient Weight (kg) Reprinted with permission from Cannon CP, et al. J Am Coll Cardiol. 2001;37:323A. 181 Weight-Based Dosing of Thrombolysis: How Well Do We Estimate Weight? How Often Would This Translate Into Errors With Administration of Thrombolytic Drugs and Adverse Outcomes? 1. Errors in estimating weight are uncommon, especially those that would lead to a dose change (1.3% or 49/3730 for TNK-tPA and 4.5% or 13/290 for t-PA). 2. No adverse outcomes were seen among patients who received an incorrect dose, suggesting a broad safety profile for the new single-bolus agent TNK-tPA. Cannon CP, et al. J Am Coll Cardiol. 2001;37:323A. ASSENT-3: Study Group Conclusions Regarding TNK-tPA + Abciximab Therapy • “The results obtained with half-dose tenecteplase plus abciximab are very similar to those with half-dose reteplase and abciximab seen in GUSTO-V.” • “In both trials, these benefits are obtained at the cost of a higher rate of major bleeding complications and blood transfusions.” • “No benefit and perhaps even harm was observed in patients above 75 years and in diabetics.” • “Taken together they suggest that caution should be exercised regarding the use of conjunctive therapy with abciximab in elderly patients with an acute myocardial infarction treated with a fibrinolytic agent.” The ASSENT-3 Investigators. Lancet. 2001;358:605-613. ASSENT-3: Study Group Conclusions Regarding Enoxaparin “In view of the present data and the ease of administration, enoxaparin might be considered an attractive alternative anticoagulant treatment when given in combination with tenecteplase.” The ASSENT-3 Investigators. Lancet. 2001;358:605-613. ENTIRE TIMI-23: Study Design ST MI <6h (n=461) ASA Standard Reperfusion: Combination Reperfusion: Full-dose TNK-tPA (0.53 mg/kg) Half-dose TNK-tPA + Abx (0.27 mg/kg) UFH ENOX UFH ENOX 60 U/kg bolus 12 U/kg/h infusion 36 h varying doses +/- IV bolus Index Hosp ( 8 d) 40 U/kg bolus 7 U/kg/h infusion 36 h varying doses +/- IV bolus Index Hosp ( 8 d) Antman E, et al. Eur Heart J. 2001;22:15. Abstract 145. Outstanding Issues • Should enoxaparin replace UFH as the optimal antithrombin agent for AMI? • Will similar improvements in efficacy and safety occur if enoxaparin is combined with a less fibrin-specific agent such as r-PA? • Will physicians accept the use of enoxaparin in selected patients with ST-elevation MI who may require rescue PCI? • Will trials of TNK-tPA plus the small molecule GP IIb/IIIa receptor inhibitors produce results similar to ASSENT-3? • What is the optimal strategy for facilitated PCI? Future Trials: Potential Downstream Targets • Large embolii: Filters • Small embolii (thrombii): Filters & GP IIb/IIIa inhibitors, p-selectin inhibitors • Vasoconstrictor release: GP IIb/IIIa inhibitors • Spasm: Adenosine, Ca channel blockers, alpha blockers, avoid over sizing with PCI, high pressure inflations, serotonin inhibitors, endothelin inhibitors • Endothelial & Myocardial swelling: Myocardial cooling, Ca channel blockers, DHEA, Na / H pump inhibitors, anti-inflammatory approaches Conclusions (cont.) Antiplatelet Agents — ASA & GP IIb/IIIa Blockers • ASA in treating ACS reduces relative risks of CVD/MI by 35%-50% • GP IIb/IIIa blockers offer benefits in… – CVD/MI/emergency revascularization: RRR up to 50% – CVD/MI: RRR 10% to 27% • Patients undergoing PTCA also have benefited from GP IIb/IIIa inhibitors • Patients with acute MI may benefit from GP IIb/IIIa inhibition + thrombolysis Conclusions (cont.) Anticoagulants — Indirect Antithrombins — UFH & LMWH • Antithrombin therapy treats acute exacerbation via short-term treatment • UFH+ASA better than placebo or ASA alone in reducing CVD/MI/RA • LMWH has clinical advantages over UFH, and is a useful agent early in treatment Conclusions (cont.) Anticoagulants — Direct Antithrombin - Hirudin • Studied internationally in 29,000+ patients • Neutralizes clot-bound and soluble fibrin; no allergic reactions (lack of HIT) • In acute MI, hirudin and UFH have equivalent effects as adjunctive therapy to thrombolysis • In PTCA, hirudin is associated with fewer cardiac events compared to UFH • In ACS, hirudin is superior to UFH: – CVD/MI RRR 14% — 24% – CVD/MI/RA RRR 19% — 22% Conclusions (cont.) Summary • Direct thrombin inhibition offers benefits over indirect thrombin inhibition for ACS • Hirudin appears to be a safe, superior alternative to UFH • Longer treatment durations need to be assessed for possible long-term benefits • Combining a thrombin-specific inhibitor (eg, hirudin) with a GP IIb/IIIa blocker may be an even more effective antithrombotic therapy for ACS Comparative Advantages of Stress Echocardiography and Stress Radionuclide Perfusion Imaging in Diagnosis of CAD • Advantages of Stress Echocardiography 1. Higher specificity 2. Versatility - more extensive evaluation of cardiac anatomy and function 3. Greater convenience / efficacy / availability 4. Lower cost • Advantages of Stress Perfusion Imaging 1. Higher technical success rate 2. Higher sensitivity - especially for single vessel coronary disease involving the left circumflex 3. Better accuracy in evaluating possible ischemia when multiple resting LV wall motion abnormalities are present 4. More extensive published data base - especially in evaluation of prognosis Prognostic Markers in Exercise Testing The Duke Treadmill Score (risk calculation) The Duke treadmill score = – exercise time in minutes on Bruce Protocol – minus 5x the ST-segment deviation (during or after exercise, in millimeters) – 4x the angina index (“0” if there is no angina, “1” if angina occurs, and "2" if angina is the reason for stopping the test). • works well for both inpatients and outpatients, and equally well for men and women N Engl J Med 1991;325:849-53 Survival According to Risk Groups Based on Duke Treadmill Score 4 -Year Annual Risk Group (Score) Total Survival Low ( +5) 62% Moderate (-10 to +4) High (< -10) 34% Mortality 99% 95% 4% N Engl J Med 1991;325:849-53 0.25% 1.25% 79% 5.00% Risk Stratification With Coronary Angiography • the extent and severity of coronary disease and LV dysfunction are the most powerful clinical predictors of long-term outcome – proximal coronary stenoses – severe left main coronary artery stenosis • CASS registry of medically treated patients, the 12-year survival rate Coronary arteries Ejection fraction normal coronary arteries 91% one-vessel disease two-vessel disease three-vessel disease 50% to 100% 74% 35% to 49% 59% <35% 40% Circulation 1994;90:2645-57 73% 54% 21% Risk Factors for Coronary Artery Disease • Age: > 45 y/o male; > 55 y/o female; or post-menopausal female without estrogen therapy • Male gender • Hypertension • Diabetes mellitus • Hypercholesterolemia/Hypertriglyceridemia • Smoking • Family history of early CAD female age < 65; male age < 55 • Past personal history of PVD or CVA Risk Factors for Coronary Artery Disease (con’t) • Left ventricular Hypertrophy • Cocaine/Ethanol Abuse • Obesity • Sedentary Lifestyle • Oral contraceptives • Homocysteine elevation • Fibrinogen, C-reactive protein, Lp (a) Guidelines to Reduce Risk For Patients With Coronary Disease and other vascular disease Cessation of smoking Lipid Management Goals Primary Goal: LDL < 100 mg/dl Secondary: HDL > 35 mg/dl TG < 150 mg/dl Physical activity: 30 minutes 3-4 times per week Weight management Antiplatelet/anticoagulants:ASA 80 to 325 mg/day (or clopidogrel 75m/day) ACE inhibitors (post-MI for LVD) Beta blockers for high-risk patients post-MI Blood pressure control: goal < 130/85 mm Hg Adapted from Smith, Circulation 1995;92:3 Medical Therapy For Patients with CAD or Other Vascular Disease Risk Reduction • ASA 20-30% • Beta Blockers 20-35% • ACE inhibitors • Statins 22-25% 25-42% The four medications every atherosclerosis patient should be treated with, unless contraindications exist and are documented Adapted from the UCLA CHAMP Guidelines 1994 Protocol Design TIMI IIIA 391 Patients with Unstable Angina / NQWMI IV Heparin, (ASA), Beta-blockers, Nitrates, Ca++ blockers Baseline Angio Angio Exclusion: no CAD or LMain Randomize t-PA 0.8 mg/kg over 90 mins Primary Endpoint: Death, MI, Positive ETT 6 weeks Placebo Angio 18-36 hrs Follow-up 6 weeks Circulation 1993;87:38-52 Primary Results TIMI IIIA Effects of tPA on Coronary Lesions BASELINE ANGIORAPHY: Apparent thrombus 35% ANGIORAPHY AFTER tPA: No thrombus 35% Possible thrombus 30% Improvement in Culprit Lesion: 25% t-PA vs. 19% placebo TIMI IIIA Investigators. Circulation 1993;87:38-5 Protocol Design TIMI IIIB 1473 Patients with Unstable Angina / NQWMI ASA, IV Heparin, Beta-blockers, Nitrates, Ca++ blockers Randomize Early Invasive: Cath 18-48 h PTCA/CABG prn 2x2 Factorial: t-PA vs. Placebo 1o Endpoint Inv-Cons: Death, MI, Positive ETT - 6 weeks ETT 6 weeks Circulation 1994;89:1545-56 Follow-up 1 year Early Conservative: ST Holter, ETT Thallium Cath/PTCA if +ischemia 1o Endpoint t-PA: Death, MI, Rec Isch, + ETT, Thallium or ST Holter Primary Results TIMI IIIBtPA vs. Placebo in Non-ST Elevation ACS Composite Endpoint 80 12 70 60 Death or MI 54.2 55.5 10 0.8 40 0.7 8.8 8 50 0.6 6.2 6 30 ICH 0.55 0.5 0.4 0.3 4 20 0.2 2 10 0 0.1 0 tPA Placebo P = NS 0 0 tPA Placebo P = 0.05 tPA Placebo P = 0.05 TIMI IIIB Investigators. Circulation 1994;89:154556 Primary Results TIMI IIIB Early Invasive vs. Conservative Strategy Events at 42d No. Pts Death (%) MI (%) D/MI/+ETT (%) Rehosp Angina (%) D/MI/Rehosp (%) LOS (days) # Days rehosp Invasive Conservative p value 740 733 2.4 2.5 NS 5.1 5.7 NS 16.2 18.1 NS 7.8 15 10.2 365 14.1 22 10.9 930 <0.001 0.007 <0.001 <0.001 TIMI IIIB Investigators. Circulation 1994;89:154556 TIMI III REGISTRY Protocol Design • All consecutive patients admitted with unstable angina were screened. • Inclusion Criteria: Ischemic pain >5 mins within 96 hrs with unstable pattern: At rest, accelerating, post MI • Exclusion Criteria: Non-ischemic pain, ST elevation, admitted for revascularization procedure • Patients in specific subgroups defined by gender, race and age were randomly selected for detailed evaluation and follow-up at 6 weeks and 1 year. Risk Stratification TIMI III REGISTRY Admission ECG as a prognostic indicator _ >0.1 mV LBBB ST deviation Tw change No ECG changes 22.9 25 20 Death or MI 15 11 10 5 6.8 6.6 2.6 0.8 1.6 1.6 3.6 8.2 3.7 3.7 0 In-Hospital 6 Weeks 1 Year Stone PH, TIMI III Registry Study Group. JAMA 1996;275:11041112. TIMI IIIB Risk Stratification cTnI to Predict Risk of Mortality in ACS All Patients Enrolled 0-6 hrs No CKMB Elev P<0.001 All Patients Enrolled 6-24 hrs P <0.05 No CKMB Elev P<0.001 All Patients Enrolled 0-24 hrs P <0.05 No CKMB Elev 0 1 2 3 4 5 TnI < 0.4 ng/ml TnI > 0.4 ng/ml Mortality at 42 Days (%) Antman et al. NEJM 1996; 335:1342-9 Dr.Sarma@works