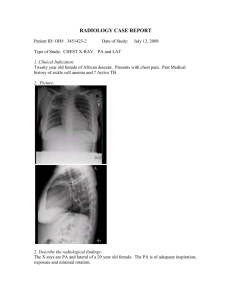
Pneumonia TB
advertisement

Pneumonia Dr Ibrahim Bashayreh, RN, PhD. 28/10/2009 1 Pneumonia Acute inflammation of lung (lower respiratory tract) caused by microorganism, comes with fever, focal chest symptoms, shadowing on CXR Leading cause of death until 1936 Discovery of sulfa drugs and penicillin 28/10/2009 2 Classification 28/10/2009 Community Acquired Pneumonia Occur within 48 hrs of admission or in patient’s who haven’t been hospitalized in the last 2 wks Strep pneumonia, mycoplasma pneumonia, influenza A, Haemophilus influenza, and Legionella are more common pathogens Patients with chronic diseases are more prone to Klebsiella and other gram negative organisms Highest incidence in winter Smoking important risk factor 3 Types of Pneumonia Hospital-acquired pneumonia (HAP) (Nasocomial Infection) 28/10/2009 Develops 2 or more days after admission Gram negative bacilli (Klebsiella, Pseudomonas, E coli, Proteus) or Staphylococcus are more common pathogens Aspiration around an ETT/reduced consciousness or difficulty swallowing allows pathogens in the oropharynx to colonize the lungs Ventilator-associated pneumonia (VAP): in patients on ventilators Aspiation: follows aspiration of gastric contents Immunosuppression: chemotherapy/bone marrow transplant/HIV patients susceptible to fungi and viral infections as well as other pathogen Highest mortality rate of nosocomial infections 4 Causes of HAP Pseudomonas Enterobacter S. aureus S. pneumoniae Immunosuppressive therapy General debility Endotracheal intubation 28/10/2009 5 Aging, 65 years or older Male Children under 2 Having HIV or AIDS Increased frequency of gram- negative bacilli (leukemia, diabetes, alcoholism) Smoking Being around certain chemicals Living in certain parts of the country Being hospitalized in ICU & having ETT Pollution Malnutrition 28/10/2009 6 Acquisition of Organisms Aspiration from nasopharynx, oropharynx Inhalation of microbes Hematogenous spread from primary infection elsewhere 28/10/2009 7 Signs & Symptoms Symptoms Dyspnea Pleurisy Cough Discolored sputum Signs Cyanosis Tachycardia Tachypnea Dull percussion Crepitus Bronchial breath sounds Pleural rub Sweating, cold clammy skin Non-respiratory features Confusion, fatigue Diarrhea, N&V. 28/10/2009 8 Clinical Manifestations CAP symptoms Sudden onset of fever Chills Cough productive of purulent sputum Pleuritic chest pain 28/10/2009 9 Pathophysiology: Pneumococcal Pneumonia Congestion from outpouring of fluid into alveoli Microorganisms multiply and spread infection, interfering with lung function 28/10/2009 10 Pathophysiology: Pneumococcal Pneumonia Red hepatization Massive dilation of capillaries Alveoli fill with organisms, neutrophils, RBCs, and fibrin Causes lungs to appear red and granular, similar to liver 28/10/2009 11 Complications Pleurisy (pain with breathing) Pleural effusion Usually is sterile and reabsorbed in 1-2 weeks or requires thoracentesis Atelectasis Usually clears with cough and deep breathing 28/10/2009 12 Complications Delayed resolution Persistent infection seen on x-ray as residual consolidation Lung abscess (pus-containing lesions) Empyema (purulent exudate in pleural cavity) Requires antibiotics and drainage of exudate 28/10/2009 13 Complications Pericarditis From spread of microorganism Arthritis Systemic spread of organism Exudate can be aspirated Meningitis Patient who is disoriented, confused, or somnolent should have lumbar puncture to evaluate meningitis 28/10/2009 14 Complications Endocarditis Microorganisms attack endocardium and heart valves Manifestations similar to bacterial endocarditis 28/10/2009 15 Diagnostic Tests History Physical exam Chest x-ray Gram stain of sputum Sputum culture and sensitivity Pulse oximetry or ABGs CBC, differential, chems Blood cultures 28/10/2009 16 Collaborative Care Antibiotic therapy Oxygen for hypoxemia Analgesics for chest pain Antipyretics Influenza drugs Influenza vaccine Fluid intake at least 3 L per day Caloric intake at least 1500 per day 28/10/2009 17 Collaborative Care Pneumococcal vaccine Indicated for those at risk Chronic illness such as heart and lung disease, diabetes mellitus Recovering from severe illness 65 or older In long-term care facility 28/10/2009 18 Nursing Assessment History of Predisposing/Risk Factors Lung cancer COPD Diabetes mellitus Debilitating disease Malnutrition 28/10/2009 19 Nursing Assessment History of Predisposing/Risk Factors AIDS Use of antibiotics, corticosteroids, chemotherapy, immunosuppressants Recent abdominal or thoracic surgery Smoking, alcoholism, respiratory infections Prolonged bed rest 28/10/2009 20 Nursing Assessment Clinical Manifestations Dyspnea Nasal congestion Pain with breathing Sore throat Muscle aches Fever 28/10/2009 21 Nursing Assessment Clinical Manifestations Restlessness or lethargy Splinting affected area Tachypnea Asymmetric chest movements Use of accessory muscles Crackles Green or yellow sputum 28/10/2009 22 Nursing Assessment Clinical Manifestations Tachycardia Changes in mental status Leukocytosis Abnormal ABGs Pleural effusion Pneumothorax on CXR 28/10/2009 23 Nursing Diagnoses Ineffective breathing pattern Ineffective airway clearance Acute pain Imbalanced nutrition: less than body requirements Activity intolerance 28/10/2009 24 Planning Goals: Patient will have Clear breath sounds Normal breathing patterns No signs of hypoxia Normal chest x-ray No complications related to pneumonia 28/10/2009 25 Nursing Implementation Teach nutrition, hygiene, rest, regular exercise to maintain natural resistance Prompt treatment of URIs 28/10/2009 26 Nursing Implementation Encourage those at risk to obtain influenza and pneumococcal vaccinations Reposition patient q2h Assist patients at risk for aspiration with eating, drinking, and taking meds 28/10/2009 27 Nursing Implementation Assist immobile patients with turning and deep breathing Strict asepsis Emphasize need to take course of medication(s) Teach drug-drug interactions 28/10/2009 28 Evaluation Dyspnea not present SpO2 > 95 Free of adventitious breath sounds Clears sputum from airway 28/10/2009 29 Evaluation Reports pain controlled Verbalizes causal factors Adequate fluid and caloric intake Performs ADLs 28/10/2009 30 Tuberculosis Famous people who have had TB Fredric Chopin* Eleanor Roosevelt* Nelson Mandela Ringo Starr Tom Jones Tina Turner *Died of TB 28/10/2009 31 What is tuberculosis (TB)? Disease caused by bacteria called Mycobacterium tuberculosis Chronic bacterial infection Was once the leading cause of death in US The number of cases declined in the 1940’s when drugs were developed to treat TB TB is still a problem worldwide 8 million people develop TB yearly 3 million die 28/10/2009 32 Tuberculosis 5-10% become active Only contagious when active Primarily affect lungs but… Kidneys Liver Brain Bone 28/10/2009 33 How is TB spread? Through the air from person to person by coughing Usually attacks lungs Two stages Latent TB asymptomatic and not contagious can take medication to prevent development of disease Active TB Disease May spread to others May have abnormal chest x-ray Usually have positive skin test 28/10/2009 34 Symptoms of TB Chills Fever Weakness or fatigue Sweating while sleeping, Night sweats Cough that lasts longer than 2 weeks Pain in chest Coughing up blood or sputum 28/10/2009 35 Risk Factors Close contact with someone who is infected with TB Traveling to a country where TB is common Foreign-born individuals and minorities have a higher incidence of developing TB 2002: 50% of US cases were in foreignborn individuals. 2002: 80% of all US TB cases were in ethnic and racial minorities. 28/10/2009 36 Risk Factors Immunocompromise Substance abuse Indigent (POVERTY) Living in overcrowded, substandard housing Health care workers performing high risk activities 28/10/2009 37 Multi-drug resistant TB (MDR TB) Bacteria become resistant to antibiotics Arose from improper use of antibiotics in the treatment of TB Treatment of one case can cost up to $1.3 million 45 states and Washington, DC have confirmed cases of MDR TB Treatment is difficult and costly Can develop from not taking proper course of antibiotics for TB MDR TB can be spread by an infected person 28/10/2009 38 How to protect yourself BCG vaccine for TB is given in many countries Not recommended for healthcare workers unless a high percentage of patients are infected with MDR TB PPD test if exposure is suspected USE proper PPE when in contact with patients who may have TB 28/10/2009 39 PPD Skin Test Procedure Intradermal administration of PPD L forearm Must be “read” between 48 and 72 hours To accurately “read” Visual inspection for erythema Tactile inspection to monitor size of induration 10 mm or > area of induration 28/10/2009 Consider positive and must be referred 40 Tuberculosis Diagnostic exams PPD Mantoux skin test > 10mm in diameter induration Indicates: Latent TB Read 48-72 after Intradermal: 15-degrees Do not rub 28/10/2009 41 Confirmation of Disease Positive reaction does not necessarily mean active disease. May indicate exposure to TB Diagnosis confirmed by: Positive smear for AFB and Sputum culture of Mycobacterium tuberculosis 28/10/2009 42 Interventions Combination drug therapy Isoniazid Rifampicin Pyrazinamide Ethambutol or streptomycin Education Must follow exact drug regimen Proper nutrition Reverse weight loss and lethargy About 28/10/2009 disease 43 Tuberculosis Treatment INH Isonicotinyl Hydrazine Isoniazid Toxic to the liver Rifampicin Turns urine red Streptomycin Causes 8th cranial nerve damage Acoustic nerve 28/10/2009 44 CLASSIFICATION Class 0—no exposure Class 1—exposure, no infection Class 2—latent infection; no disease (positive PPD but no evidence of active TB Class 3—disease; clinically active Class 4—disease; not clinically active Class 5—suspected disease; diagnosis pending 28/10/2009 45 MEDICAL MANAGEMENT Treated with chemotherapeutic agents for 612 months Resistance increasing. May be primary, secondary, or multidrug resistant. Primary—resistance to one of first line drugs in those who have not had prior treatment Secondary—resistance to one or more antiTB drugs in patients undergoing tx Multidrug resistance—resistance to two agents, INH and Rifampicin. 28/10/2009 46 Tuberculosis Complications Pleurisy Pericarditis Meningitis Bone infections Malnutrition Drug-toxicity 28/10/2009 47 Tuberculosis Nursing Dx Impaired gas exchange Ineffective airway clearance Anxiety Knowledge deficit Alt. nutrition 28/10/2009 48 Tuberculosis Preventative measures Clean well ventilated living areas Resp. isolation Vaccine? BCG Does not prevent TB Causes a + PPD If exposed take INH 28/10/2009 49 Tuberculosis Summary Chronic bacterial infection spread through the air Fever, chills, sweating while sleeping, persistent cough, coughing up blood or sputum Multi-drug-resistant tuberculosis MDR TB Use proper PPE and get PPD test if exposed 28/10/2009 50