Lower Urinary Tract Infection
advertisement
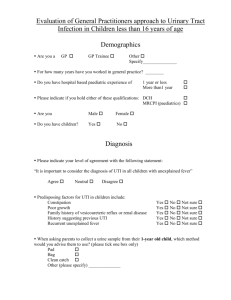
Lower Urinary Tract Infection Dr. Belal Hijji, RN, PhD April 25 & 30, 2012 Learning Outcomes At the end of this lecture, students will be able to: • Identify the risk factors for the development of urinary tract infection (UTI). • Describe the clinical manifestations of UTI. • Describe assessment and tests to diagnose UTI. • Describe the medical management of a patient with UTI • Discuss the nursing process as a framework for care of patient with UTI. 2 Introduction • Several mechanisms maintain the sterility of the bladder: the physical barrier of the urethra, urine flow, and ureterovesical junction competence. • Risk factors for UTI include: – Inability or failure to empty the bladder completely. – Obstructed urinary flow, from congenital anomalies, urethral strictures, bladder tumors, and calculi (stones) in the ureters or kidneys. – Decreased natural host defenses or immunosuppression. – Instrumentation of the urinary tract (eg, catheterization). – Inflammation of the urethral mucosa. – Contributing conditions such as diabetes mellitus (increased urinary glucose levels create an infection-prone environment in the urinary tract), pregnancy, and other altered states characterized by incomplete emptying of the bladder and urinary stasis. 3 FIGURE 1 Mechanisms of urethrovesical and ureterovesical reflux may cause urinary tract infection. Urethrovesical reflux: With coughing and straining, bladder pressure rises, which may force urine from the bladder into the urethra (A). When bladder pressure returns to normal, the urine flows back to the bladder (B), which introduces bacteria from the urethra to the bladder. Ureterovesical reflux: With failure of the ureterovesical valve, urine moves up the ureters during voiding (C) and flows into the bladder when voiding stops (D). This prevents complete emptying of the bladder. It also leads to urinary 4 stasis and contamination of the ureters with bacteria-laden urine. Clinical Manifestations • About half of all patients with bacteriuria have no symptoms. • Signs and symptoms of uncomplicated lower UTI (cystitis) include frequent pain and burning on urination, frequency, urgency, nocturia, incontinence, and suprapubic pain. Hematuria and back pain may also be present. 5 Assessment and Diagnostic Findings • UTI is diagnosed by bacteria in the urine. A colony count of at least 105 colony-forming units (CFU) per milliliter of urine on a clean-catch midstream or catheterized specimen is a major criterion for infection. However, UTI and subsequent sepsis have occurred with lower bacterial colony counts. • Hematuria (greater than 4 red blood cells [RBCs] per highpower field) is present in 50% of patients. Pyuria (greater than 4 white blood cells [WBCs] per high-power field) occurs in all patients with UTI; however, it can also be seen with kidney stones, interstitial nephritis, and renal tuberculosis. • Urine cultures remain the gold standard in documenting a UTI and can identify the specific organism present. 6 Medical Management • Management of UTIs typically involves pharmacologic therapy and patient education. The nurse is a key figure in teaching the patient about medication regimens and infection prevention measures. • Trimethoprim sulfamethoxazole and nitrofurantoin. Occasionally, ampicillin or amoxicillin are used, but E. coli organisms have developed resistance to these agents. • Ciprofloxacin. • Levofloxacin. 7 Nursing Management • Assessment: Assess, document and report the presence of pain, frequency, and urgency and changes in urine including color, concentration, and cloudiness, all of which are altered by bacteria in the urinary tract. The patient’s knowledge about prescribed antimicrobial medications and preventive health care measures is also assessed. • Nursing Diagnoses: Based on the assessment data, the nursing diagnoses may include the following: – Acute pain related to inflammation and infection of the urethra, bladder, and other urinary tract structures. – Deficient knowledge related to factors predisposing the patient to infection, detection and prevention of recurrence, and pharmacologic therapy. 8 • Planning and goals: Major goals for the patient may include relief of pain and discomfort; increased knowledge of preventive measures and treatment regimen; and absence of complications. • Nursing interventions: – Pain Relief: The pain associated with UTI is quickly relieved once effective antimicrobial therapy is initiated. Aspirin and applying heat to the perineum help relieve pain and spasm. The patient should drink liberal amounts of water to promote renal blood flow and to flush the bacteria from the urinary tract. Urinary tract irritants (eg, coffee, tea, citrus, spices, colas, alcohol) are avoided. Voiding every 2 to 3 hours is encouraged to empty the bladder completely because to significantly lower urine bacterial counts, reduce urinary stasis, and prevent reinfection. 9 – Monitoring and Managing Potential Complications: Early recognition of UTI and prompt treatment are essential to prevent recurrent infection and the possibility of complications (renal failure and sepsis). Thus, the patient must be taught to recognize early signs and symptoms, to test for bacteriuria, and to initiate treatment as prescribed. Appropriate antimicrobial therapy, liberal fluid intake, frequent voiding, and hygienic measures are commonly prescribed for managing UTI. Patients with catheterassociated UTI are at increased risk for septic shock. Indwelling catheters should be avoided if possible and removed at the earliest opportunity. If an indwelling catheter (Slide 11) is necessary, the following nursing interventions are initiated to prevent infection: • Using strict aseptic technique during insertion of the catheter (Slide 12). • Securing the catheter with tape to prevent movement. • Frequently inspecting urine color, odor, and consistency. • Performing meticulous daily perineal care with soap and water. • Maintaining a closed system. • Using the catheter’s port to obtain urine specimens. 10 Urine bag Diagram of a foley catheter 11 Urinary catheterization with a dummy 12 – Patient Education: An objective of teaching about recurrent UTIs is their prevention, through implementing careful personal hygiene, increasing fluid intake to promote voiding and dilution of urine, urinating regularly and more frequently, and adhering to the therapeutic regimen. • Hygiene: Shower rather than bathe in tub because bacteria in the bath water may enter the urethra. After each bowel movement, clean the perineum and urethral meatus from front to back. This will help reduce concentrations of pathogens at the urethral opening and, in women, the vaginal opening. • Fluid Intake: Drink liberal amounts of fluids daily to flush out bacteria. Avoid coffee, tea, colas, alcohol, and other fluids that are urinary tract irritants. • Voiding Habits: Void every 2 to 3 hours during the day and completely empty the bladder. This prevents overdistention of the bladder and compromised blood supply to its wall. Both predispose the patient to UTI. 13 • Therapy: Instruct the patient to take medication exactly as prescribed. For recurrent infection, instruct the patient to take ascorbic acid (vitamin C), 1,000 mg daily, or cranberry []التوت البري juice to acidify urine. Instruct the patient to test urine for bacteria as recommended. Finally, teach the patient to consult the health care provider regularly for follow-up, recurrence of symptoms, or infections not responsive to treatment. 14 • Evaluation: Expected patient outcomes may include: – Experiences relief of pain • Reports absence of pain, urgency, dysuria, or hesitancy on voiding • Takes analgesic and antibiotic agents as prescribed – Explains UTIs and their treatment • Demonstrates knowledge of preventive measures and prescribed treatments • Drinks 8 to 10 glasses of fluids daily • Voids every 2 to 3 hours • Voids urine that is clear and odorless – Experiences no complications • Reports no symptoms of infection (fever, dysuria, frequency) or renal failure (nausea, vomiting, fatigue, pruritus) • Has normal BUN and serum creatinine levels, negative urine and blood cultures • Exhibits normal vital signs and temperature; no signs or symptoms of sepsis • Maintains adequate urine output more than 30 mL per hour 15