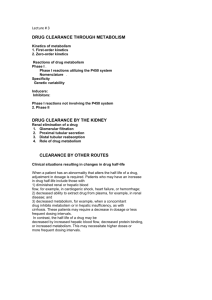
PHARMACOKINETICS
advertisement

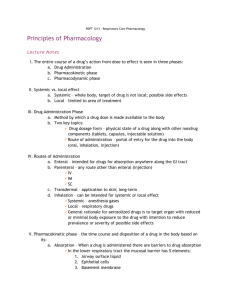
PHARMACOKINETICS WHAT THE BODY DOES TO THE DRUG XENOBIOTIC A compound to which the body is exposed that is foreign to the body. Includes drugs, industrial and environmental chemicals Pharmacodynamics – concentration – effect Graded response Quantal response Pharmacokinetics – dose - concentration Routes of drug administration Oral Inhalational Sublingual Transdermal Rectal Subcutaneous Transnasal Intramuscular Intra-tracheal Intravenous Routes of Administration PHARMACOKINETICS ABSORPTION DISTRIBUTION METABOLISM EXCRETION ABSORPTION Describes the rate and extent to which a drug leaves its site of administration Pharmacokinetics Absorption –the process by which the drug moves into the body from external source Drug Absorption Orally Rectually (drug embedded in a suppository, which is placed in the rectum) Parenterally (given in liquid form by injection with a needle and syringe) Inhaled –thru the lungs as gases, as vapors, or as particulars carried in smoke or in an aerosol Absorbed through the skin Absorbed through mucous membranes (from snorting or sniffing the drug, with the drug depositing on the oral or nasal mucosa) Drug Absorption caveats Orally Drug must be soluble and stable in stomach fluid (not destroyed by gastric acids), enter the intestine, penetrate the lining of the stomach or intestine, and pass into the blood stream. Drug Absorption disadvantages May occasionally lead to vomiting and stomach distress. How much of the drug will be absorbed into the bloodstream cannot always be accurately predicted because of the genetic differences between people and because differences in the manufacture of the drugs. The acid in the stomach destroys some drugs. Drug Absorption caveats Rectually Rarely used unless patient is vomiting, unconscious, or unable to swallow Drug Absorption disadvantages Rectually Often irregular, unpredictable, and incomplete Many drugs irritate the membranes that line the rectum. Drug Absorption Parenterally Intravenous –directly into a vein Intramuscular –directly into muscle Subcutaneous –just under the skin Drug Absorption Parenterally Often produces a more prompt response than does oral administration because absorption is faster. Permits a more accurate dose because the unpredictable processes of absorption are bypassed. Drug Absorption disadvantages Parenterally Leaves little time to respond to an unexpected drug reaction or accidental overdose. Requires the use of sterile techniques. Once a drug is administers by injection, it cannot be recalled. Drugs that cannot become completely soluble before injection, cannot be injected intravenuously. Drug Absorption Inhaled Lung tissues have a large surface area with large blood flow, allowing for rapid absorption of drugs. Relatively quick route to the brain.* *May even have a faster onset of effect than drugs administered intravenously. Drug Absorption Absorbed through the skin Provides continuous, controlled release of a drug from a reservoir through a semipermeable membrane. Potentially minimizes side effects associated with rapid rises and falls in plasma concentration of the drug contained in the patch. CHARACTERISTICS OF A DRUG FAVORING ABSORPTION Low molecular size Nonpolar Uncharged High lipid solubility MECHANISMS OF SOLUTE TRANSPORT ACROSS MEMBRANES Passive diffusion Facilitated Active diffusion transport Endocytosis Passive Diffusion Concentration gradient Lipid-water partition coefficient Area, Thickness and Permeability of the membrane Ionic, pH, charge gradient* Ionic Transport pH gradient Drug’s (pKa) acid dissociation constant pKa – pH value at which one half of the drug is present in ionic form pKa = pH + log (HA) (A-) Henderson-Hasselbalch equation Calculates the ratio of non-ionized to ionized drug at each ph pH = log [A-] + pka (Acid) [HA] or = log [B] + pKa (Base) [BH+] Ka = dissociation constant A = molar concentration of the acidic anion HA = molar concentration of the undissociated acid B = molar concentration of the basic anion HB = molar concentration of the undisscociated base Drugs and ionisation : Theory Many drugs are weak acids or weak bases • Acids =aspirin, barbiturates • Bases =propranolol, opioids The pKa of a drug is the pH at which it is 50% ionised and 50% unionised • aspirin has pKa of 3.5 : at an acid pH of 3.5 it is 50% U/I • propranolol has a pKa of 9.4 : at a basic pH of 9.4 it 50% U/I Drugs and ionisation : Theory The more acidic the pH for an acidic drug the more of it is unionised, and vice versa for a basic drug The U fraction is lipid soluble and thus crosses cell membranes more easily than the I fraction Drugs and ionisation: Which of the following statements are correct? Explain briefly 1. Ionised drugs do not easily cross lipid barriers such as the gut, placenta and blood brain 2. Acidic drugs are well absorbed in the acidic medium of the stomach, basic drugs in the alkaline medium of the small bowel Characteristics of Un-ionized and Ionized Drug Molecules Un-ionized Ionized Pharmacologic effect Solubility Cross lipid barriers Active Lipids Yes Inactive Water No Yes No No Yes (gastrointestinal tract, blood-brain barrier, placenta) Hepatic metabolism Renal excretion Drugs and ionisation: Practise Acidic drugs (such as aspirin) will be ionised in an alkaline urine and thus cannot be reabsorbed across the renal tubular membrane (alkaline diuresis) pH trap (ion trapping) is significant for some drugs, especially local anaesthetics in labor Factors Affecting DRUG ABSORPTION Biopharmaceutic Factors • - Tablet compression • - Coating and Matrix • - Excipients Interactions • - Food • - Other Drugs • - Bacteria Physiological Factors Factors Affecting GI Absorption Gastric Emptying Time Intestinal Motility Food Formulation Factors “First Pass Effect” PK Definitions Cmax: Maximum concentration – may relate to some side effects Plasma Concentration 10000 AUC: Area under the curve (filled area) = overall drug exposure 3000 1000 Cmin: minimum or trough concentrations: may relate with efficacy of HIV drugs 100 0 2 4 6 8 Time Postdose (hr) http://www.thebody.com/content/art875.html 10 12 Drug Levels & Resistance BIOAVAILABILITY Quantity of drug in systemic circulation Quantity of drug administered Bioavailability BIOAVAILABILITY is the fraction of the oral (rectal) dose reaching the systemic circulation High bioavailability means good absorption and limited liver metabolism Are these two properties compatible? Bioavailability Oral and rectally administered drugs are absorbed via the gut wall into the portal circulation The liver (and gut wall) removes drugs by ‘first pass’ metabolism and binding so only a proportion reaches the hepatic veins and the systemic circulation Bioavailability Lipid soluble drugs such as propranolol are well absorbed but have high ‘first pass’ and hepatic extraction ratio (thus low oral bioavailability) versus water soluble drugs such as digoxin 1. How do you measure bioavailability? 2. Which pharmacokinetic parameter most reliably reflects the amount of drug reaching the target tissue after oral administration? Measuring bioavailability I.v. dose Log Concentration Bioavailability = AUC I.v. AUC oral/ AUC i.v. Oral dose AUC oral time Bioavailability (f) f = dose(IV) x AUC (PO)/dose(PO) x AUC (IV) Why do we need to know the bioavailability of a drug? To determine the correct route of administration e.g. i.v. versus i.m., oral versus rectal To determine the correct dosage DISTRIBUTION Delivery of drug from systemic circulation to tissues Pharmacokinetics Distribution –the drug is distributed throughout the body (including fetus) Distribution The movement of drug from the blood to and from the tissues Drug Distribution 4 Body Membranes that Affect Drug Distribution 1. Cell membranes 2. Walls of the capillary vessels in the circulatory system 3. Brain-blood barrier 4. Placental barrier Drug Distribution 1st Body Membrane that Affects Drug Distribution Cell membranes Permeable to small lipid (fatty) molecules Drug Distribution 2nd Body Membrane that Affects Drug Distribution Walls of the capillary vessels in the circulatory system Does not depend on lipid solubility Only drugs that do not bind to plasma proteins pass through capillary pores. Drug Distribution 3rd Body Membrane that Affects Drug Distribution Brain-blood barrier The rate of passage of a drug into the brain is determined by two factors: (1) the size of the drug molecule and (2) its lipid (fat) solubility. Drug Distribution 4th Body Membrane that Affects Drug Distribution Placental barrier Oxygen and nutrients travel from the mother’s blood to that of the fetus, while carbon dioxide and other waste products travel from the blood of the fetus to the mother’s blood. Fat-soluble substances (including all psychoactive drugs) diffuse rapidly and without limitation. PATTERNS OF DRUG DISTRIBUTION Mainly in the vascular system ex. Dextran, highly bound to plasma protein apparent Vd = 3-5 L in adults (approx plasma volume) PATTERNS OF DRUG DISTRIBUTION Uniformly distributed throughout the body water ex.ethanol, sulfonamides Vd = 30-50 L corresponding to total body water PATTERNS OF DRUG DISTRIBUTION Concentrated specifically in one or more tissues that may or may not be the site of action Vd – very large values ex. Chloroquine – 1000x in the liver Tetracycline – bone and developing teeth PATTERNS OF DRUG DISTRIBUTION Non-uniform distribution in the body - highest concentrations usually in the liver, kidney and intestine - distribution varies with lipid solubility, ability to pass thru membranes Factors Affecting Drug Distribution Affecting Rate of Distribution Membrane Permeability Blood Perfusion Affecting extent of distribution Extent of plasma protein binding Regional differences in pH Lipid solubility Available transport mechanisms Intracellular Binding Membrane Permeability Capillary permeability Renal capillary permeability large pores Brain capillaries Blood Perfusion Rate Greatest blood flow – brain, kidneys, liver and muscle Highest perfusion rate – brain, kidneys, liver, heart Protein Binding Extensive plasma protein binding – lower Vd; stay in central blood compartment Slight change in the binding of highly bound drugs – significant change in clinical response Only free drug are active Plasma protein binding of drugs Acidic drugs (e.g. barbiturates) bind to albumin Basic drugs (e.g. opioids, local anaesthetics) bind to alpha 1 acid glycoprotein The process is reversible Binding sites are non-selective for similar drugs and thus one can displace another Plasma protein binding of drugs The bound drug is inactive whilst bound and this limits systemic distribution and glomerular filtration Only drugs which are highly bound (>90%) with small Vd are affected by changes in protein binding (e.g. phenytoin and warfarin) Drugs Vit. C, salicylates, sulfonamides, barbiturates, penicillins, tetracyclines, probenecid Binding sites for acidic agents Albumin Binding sites for basic agents Quinine, Streptomycin, chloram, digitoxin, coumarin Globulins, 1, 2, β1, β2 Percent Unbound for Selected drugs Drug Caffeine Digoxin Gentamicin Theophylline Phenytoin Diazepam Warfarin Phenylbutazone dicumarol % Unbound 90 77 50 85 13 4 0.8 5 3 Calculating the volume of distribution Injected dose 10 mg. ? Volume of container Sampled concentration 1 mg. l-1 Volume = injected dose/ sampled concentration = 10 litres Calculating the apparent volume of distribution Injected dose 10 mg. ? Volume of container Sampled concentration 0.1 mg. l-1 Volume = injected dose/ sampled concentration = 100 litres Why do we need to know the volume of distribution? Vd is needed to calculate the loading dose of a drug (e.g. lignocaine, aminophylline, pethidine, propofol) Loading dose = Vd * effective concentration (Ceff) required Question: What is the loading dose if Vd is 30 litres and Ceff is 10 mg.l-1 Weight consideration Vd is proportional to body weight and thus, the loading dose can be based on body weight Varies with the very young, and very old Two compartment pharmacokinetic model K12 Dose Peripheral compartment Central compartment K21 K elim Central compartment Intravascular space, highly perfused tissues Rapid uptake of drug 75% of cardiac output; 10% of body mass Apparent volume can be calculated METABOLISM Active Drug Active Drug Inactive Prodrug Unexcretable drug Inactive drug Active or toxic metabolite Active drug Excretable metabolite Pharmacokinetics Metabolism –detoxification or breakdown of the drug into metabolites that no longer exert any effect Drug Metabolism Side effects are results that are different from the primary, or therapeutic, effect, for which a drug is taken. First-pass metabolism drug-metabolizing enzymes in either the cells of the GI tract or the liver can markedly reduce the amount of drug that reaches the bloodstream. BIOTRANSFORMATION Phase I Phase II PHASE I Modify the chemical structure of a drug OXIDATION REDUCTION HYDROLYSIS Oxidative Reactions N- dealkylation – Imipramine, erythromycin O-dealkylation – Indomethacin,Codeine Aromatic hydroxylation – Phenytoin, phenobarbital N- Oxidation – chlorpheniramine, Dapsone S- oxidation - Cimetidine, Omeprazole Deamination – Amphetamine, Diazepam Liver Microsomal System Oxidative Reactions: Cytochrome P450 mediated Examples • Formation of an inactive polar metabolite • Phenobarbital • Formation of an active metabolite • By Design: Purine & pyrimidine chemotherapy prodrugs • Inadvertent: terfenadine – fexofenadine • Formation of a toxic metabolite • Acetaminophen – NAPQI (N-acetyl-p-benzoquinone imine HYDROLYSIS Ester Hydrolysis – Procaine, aspirin, Succinylcholine Amide Hydrolysis – Lidocaine, Indomethacin Epoxide Hydrolysis - Carbamazepine REDUCTION Nitro reduction – Chloramphenicol Dehalogenation – Halothane Carbonyl Reduction – Methadone, Naloxone PHASE II Conjugate a drug to large polar molecules to : Inactivate a drug Enhance drug’s solubility Enhance excretion rate CONJUGATION REACTIONS Glucoronidation – Acetaminophen, Morphine, Oxazepam Sulfation – Acetaminophen, Steroids Acetylation – Sulfonamides, INH, Clonazepam Metabolism Induction – drugs can cause an increase in liver enzyme activity thus increasing metabolic rates of some drugs ex. Phenobarbitone – induce metabolism of itself, phenytoin, warfarin Inhibition – inhibit metabolism of other drugs Drug A inhibits the production of enzymes to metabolize Drug B Induction Inhibition Liver This reduces the amount of Drug B and may lead to loss of Drug B’s effectiveness Drug A induces the body to produce more of an enzyme to metabolized Drug B This increases the amount of Drug B in the body and could lead to an overdose or toxic effects Hepatic clearance and ratio extraction Clearance = Flow X Extraction ratio IF hepatic blood flow = 1500 ml.min-1 and extraction ratio = 50% Clearance = 750 ml. min-1 Hepatic clearance and extraction ratio Extraction ratio = Ci - Co/ Ci Ci may be calculated by determining the percentage of a drug absorbed, and thus reaching the liver Co may be calculated from the bioavailability Effect on clearance when hepatic blood flow falls (e.g. hepatic disease, decreased cardiac output and hypovolaemia) Hepatic microsomal enzymes are capable of being induced and inhibited Drugs causing induction include • barbiturates (i.e.phenobarbitone) • rifampicin • nicotine and aminophylline Drugs causing inhibition include • • • • cimetidine erythromycin metronidazole disulphiram and ethyl alcohol Effects of hepatic blood flow and enzyme induction/inhibition Metabolism of high clearance (ER) drugs (e.g. opioids) is more dependent on hepatic blood flow and less dependent of enzyme induction and inhibition Effects of hepatic blood flow and enzyme induction/inhibition Metabolism of low to moderate clearance (ER) drug ( e.g. aminophylline) is more dependent on enzyme induction and inhibition and less dependent of hepatic blood flow Drug metabolism: Zero and first order kinetics Zero order kinetics: First order kinetics: • a fixed amount of the drug is metabolised in unit time (e.g. alcohol) • a fixed fraction of the drug is metabolised in unit time Drug metabolism: Zero and first order kinetics Most drugs are metabolised by a first order process Amount metabolised is proportional to the concentration of the drug Newborn hepatic metabolism of some drugs such as phenytoin becomes saturable at therapeutic concentrations The rate constant in first order kinetics and relationship to the half life The rate constant is the fractional change in concentration in unit time It is expressed as the elimination rate constant k, in units of h-1 Thus, if 10% of the drug is removed per hour, then the rate constant is 0.1h-1 T1/2 = natural logarithm of 2 (0.693)/k Thus, k of 0.1 = T1/2 of 6.93 hours Clearance First order kinetics states that a fixed fraction of the drug is metabolised in unit time Or … the amount metabolised is proportional to the concentration Or … amount metabolised = K * concentration K is the ‘clearance’ and has the unit of flow (e.g. mls.min-1 or litres.hr-1) Why do we need to know the drug clearance? For effective drug therapy you need to be able to maintain the effective concentration (Ceff) that produces the desired effect Thus, we need to calculate the maintenance dose Why do we need to know the drug clearance? Maintenance dose = clearance * effective concentration (Ceff) e.g. if clearance is 3 l.hr-1 and Ceff is 10 mg.l-1 Maintenance dose = 30 mg.hr-1 We can thus predict the effect of changes in clearance and Ceff on maintenance dose CLEARANCE CLP =___rate of elimination (mg/min)______ plasma concentration of drug (mg/ml) The elimination half life Half life is the time taken for the concentration (in the plasma) to fall by one half HALF LIFE AND PERCENT OF DRUG REMOVED (wash out) Number of Half-lives 0 1 2 3 4 5 Percent of Drug Remaining 100 50 25 12.5 6.25 3.125 Percent of Drug Removed 0 50 75 87.5 93.75 96.875 Half life and onset of action using maintenance dose and no loading dose (wash in) Number of Half-times 0 1 2 3 4 5 Percent of final steady state concentration 0 50 75 87.5 93.75 96.875 The context sensitive half life Definition: The time for the plasma concentration to fall by half following steady state infusion and constant blood levels. Usually after several hours infusion. FACTORS AFFECTING DRUG METABOLISM Genetic variation Environmental determinants Disease Factors Age Sex Cultural Metabolism Genetic –people have different amounts of enzymes that metabolize drugs Metabolism Physiological –if more than one drug is present in the body, the drugs may interact with one another either in a therapeutically beneficial way or in a way that can adversely affect the patient. Metabolism Environmental –current mood, stress, and past experience with drug can affect metabolism (and toxicity) ROLE OF CYP ENZYMES IN HEPATIC DRUG METABOLISM RELATIVE HEPATIC CONTENT OF CYP ENZYMES CYP2D6 2% % DRUGS METABOLIZED BY CYP ENZYMES CYP2E1 7% CYP 2C19 11% CYP 2C9 14% CYP2D6 23% CYP 2C 17% OTHER 36% CYP 1A2 12% CYP 3A4-5 26% CYP 1A2 14% CYP 3A4-5 33% CYP2E1 5% Participation of the CYP Enzymes in Metabolism of Some Clinically Important Drugs CYP Enzyme Examples of substrates 1A1 Caffeine, Testosterone, R-Warfarin 1A2 Acetaminophen, Caffeine, Phenacetin, R-Warfarin 2A6 17-Estradiol, Testosterone 2B6 Cyclophosphamide, Erythromycin, Testosterone 2C-family Acetaminophen, Tolbutamide (2C9); Hexobarbital, SWarfarin (2C9,19); Phenytoin, Testosterone, R- Warfarin, Zidovudine (2C8,9,19); 2E1 Acetaminophen, Caffeine, Chlorzoxazone, Halothane 2D6 Acetaminophen, Codeine, Debrisoquine 3A4 Acetaminophen, Caffeine, Carbamazepine, Codeine, Cortisol, Erythromycin, Cyclophosphamide, S- and RWarfarin, Phenytoin, Testosterone, Halothane, Zidovudine Adapted from: S. Rendic Drug Metab Rev 34: 83-448, 2002 Factors Influencing Activity and Level of CYP Enzymes Nutrition 1A1;1A2; 1B1, 2A6, 2B6, 2C8,9,19; 2D6, 3A4,5 Smoking 1A1;1A2, 2E1 Alcohol 2E1 1A1,1A2; 2A6; 2B6; 2C; 2D6; 3A3, 3A4,5 1A1,1A2; 2A6; 1B; 2E1; Environment 3A3, 3A4,5 Genetic 1A; 2A6; 2C9,19; 2D6; Polymorphism 2E1 Drugs Adapted from: S. Rendic Drug Metab Rev 34: 83-448, 2002 Pharmacokinetics Elimination –metabolic waste products are removed from the body Elimination Drugs leave the body through: Kidneys Lungs Bile Skin Elimination Drugs leave the body through: Kidneys: 1) Excrete most of the products of body metabolism 2) Closely regulate the levels of most of the substances found in body fluids • Psychoactive drugs are often reabsorbed out of the kidneys, so the liver has to enzymatically transform the drugs so with minimal reabsorption they can exit in urine. Elimination Drugs leave the body through: Bile After most psychoactive drugs are processed by the liver they are usually less fat soluble, less capable of being reabsorbed, and therefore capable of being excreted in urine. Elimination Drugs leave the body through: Lungs Only occurs with highly volatile or gaseous agents Elimination Drugs leave the body through: Skin Small amounts of a few drugs can pass through the skin and be excreted in sweat. Processes That Determine Urinary Excretion of Drug 1. Glomerular filtration 2. Tubular secretion 3. Tubular reabsorption Drug excretion: Role of the Kidneys Drug excretion: Role of the Kidneys Glomerular clearance filtration (GFR) = fraction unbound (FU) * GFR if TOTAL renal clearance = the above, then the drug is principally excreted by filtration (e.g. gentamicin) AND clearance is proportional to GFR Drug excretion: Role of the Kidneys Passive tubular reabsorption clearance is less than FU * GFR (due to reabsorption) e.g. aspirin and amphetamine (effect of pH of urine) Active tubular secretion (ATS) clearance is greater than FU * GFR (due to secretion) e.g. penicillin (inhibited by probenecid), digoxin (inhibited by quinidine) Renal Factors that Affect Urinary Drug excretion Glomerular filtration rate Tubular fluid pH Extent of back-diffusion of unionized form Extent of active tubular secretion of the compound Extent of tubular reabsorption ADME - Summary CLINICAL PHARMACOKINETICS CLEARANCE CLP =___rate of elimination (mg/min)______ plasma concentration of drug (mg/ml) Clearance First Order Kinetic – constant fraction of the drug in the body is eliminated Saturation Kinetics – constant amount of drug is eliminated per unit time CLEARANCE: Clinical Utility Determines the maintenance dose (DM) required to achieve the target plasma conc at steady state DM(mg/h) = Tconcn (mg/L) x Clearance (L/h) Volume of Distribution Actual volume in which drug molecules are distributed within the body Vd = D/CO Co = D/Vd VOLUME OF DISTRIBUTION: Clinical Utility Used to determine the loading dose (LD) LD = Css x (mg) (mg/L) Vd (L) HALF-LIFE Time it takes for plasma concentration or the amount of drug in the body to be reduced by 50% t1/2 = (0.693 x Vd) / Cl HALF-LIFE: Clinical Utility Determines how long it takes to reach steady state after multiple dosing STEADY STATE CONCENTRATION CSS = Bioavailability x Dose Interval x Cl Initial Concentration Initial concentration = Loading Dose Vd Dosing Rate Dosing rate = Target conc’n x Cl / F Oral Digoxin is to be used as maintenance dose to gradually digitalize a 69 kg patient with congestive heart failure. A steady state plasma concentration of 1.5 ng/ml is selected as an appropriate target. Based on the patient’s renal function, the clearance of digoxin is computed at 1.6/ml/min/kg or 110ml/min. How should the drug be given in this patient? Given: Cl – 1.6ml/min/kg F – 70% Target conc’n = 1.5ng/ml Dosing rate = 1.5ng/ml x 1.6ml.min/kg/0.7