Drug metabolism22010-10
advertisement

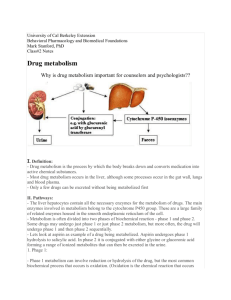
Drug Metabolism Dr.Abdul latif Mahesar 1 Drug metabolism (biotransformation) It is the type of chemical reactions which leads to modification of drugs Drugs are converted from one form to an other to make them more active ,less active and finally inactive and to leave the body 2 Sites of metabolism Hepatic: microsomes , mitochondria, cytoplasm Extrahepatic: lung ,blood ,skin , GIT, kidney. 3 Microsomes: Microsomal enzyme system→ mixed function oxidase → mono-oxygenases Its components include Cytochrome P450 Flavinoprotein (co-enzymes in redox reaction) NADPH Molecular oxygen, Drug + enzyme +oxygen molecule +NADPH +Flavoprotein 4 Mitochondria: mono-amine oxidase enzyme (MAO) Acetylation Cytoplasm: Alcohol dehydrogenase Blood (plasma) Estrases Amidases Catechol-o methyltransferases(COMT) Intestinal Mucosa and Lumen: GIT flora:Glucouronidase ,Asoreductases. GIT mucosa : Monoamime oxidase (MAO) , Sulphatase 5 Types of Reactions Metabolic Phase I reactions Phase II reactions 6 Phase-I Reactions Metabolism brings about a change in the molecule by oxidation ,reduction ,or hydrolysis and often introduces a chemically active site into it. The new metabolite may retain biological activity but have different pharmacokinetic properties e.g. short or long half life, they may become inactive or more toxic. Oxidation: The most important and main single group of reactions is the oxidations. 7 Characteristics of Phase I Products (Result of Drug Metabolism) 1. Inactivation (abolish the activity Oxidation of Phenobarbital and alcohol Hydrolysis of acetylcholine 2. conversion of active drug to another active one. Diazepam →oxydiazepam Codeine ,heroin → Morphine Phenylbutazone → oxyphenylbutazone Propranolol → 4-hydroxypropranolol 8 3. conversion of drug to toxic metabolites: Paracetamol → acetaminopen (hepatic toxicity) Halothane → metabolite hepatotoxicity 4. Activation of pro-drug Chloral hydrate → trichloroethanol Enalapril Enalaprilat 5. Product might undergo phase II 9 Phase-I Reactions : Make the drug more polar → more water soluble. (oxidation ,reduction, hydrolysis) Oxidation reaction: introduces functional group (OH,NH2,SH) Can be mirosomal or nonmicrosomal 10 Microsomal: Drug + O2 + NADPH + H→ changed drug + H2O + NADP e.g. 1. Aliphatic hydroxylation Phenobarbital → hydroxyphenobarbital 2. Aromatic hydroxylation Phenacetin→ 2-hydroxyphenacitin (paracetamol) 3. Oxidation of amine Aniline → nitrobenzene 4. sulphoxidation Parathione → paroxon 11 Reduction Reactions: Microsomal or non-microsomal Microsomal: nitrobenzene → aniline NO2 →NH2 Non-Microsomal: Chloral hydrate → trichloroethanol Hydrolysis: Non-microsomal ONLY Ester-C-O and amides-C-N Acetylcholine → choline +acetate(ester) Procainamide (lidocaine) (amide) 12 Non-microsomal: Oxidation by soluble enzyme in cytosol or mitochondria of cells e.g 1. dehydrogenases and oxidases Ethanol → acetaldehyde → acetic acid. Methanol → formaldehyde → formic acid CH3CH2OH→ CH3CHO→CH3COOH 2. monoamide oxidase(noradrenaline) 3. Hypoxanthine → xanthine → uric acid 13 Phase-II Metabolism It involves union of the drug with one of several polar(water soluble )endogenous molecules that are product of intermediatory metabolism to form water soluble conjugate which is readily eliminated by the kidney or if the molecular weight is more than 300 in the bile 14 Phase II Conjugation Reaction e.g. Morphine,paracetamol and salicylates form conjugates with glucuronic acid derived from glucose Oral contraceptive steroids form sulphates Phenalzine and dapsone are acetylated conjugation with more polar molecule is also a mechanism by which natural substances are eliminated eg.bilirubin as glucuronide and estrogen as sulphate. Phase –II reactions almost invariably terminates biological activity ALL is non-microsomal enzyme Except glucouronidation (catalyzed by glucouronyl transferase ) 15 Characteristics of Phase II Products Pharmacologically inactive More water soluble → to be excreted More readily excreted in urine 16 Modulation of Liver Microsomal Enzymes Induction Inhibition Liver Microsomal Inducers Alcohol Barbiturates Cigarette smoking Phenytoin Rifampicin Spironalactone Griseofulvin 17 Enzyme Induction results in Increase metabolism of the inducer Tolerance: decreased pharmacological action of the drug Increase the metabolism of co-administered drug (drug interaction) Barbiturate +Warfarin Phenytoin + Oral contraceptives Rifampicin + Hydrocortisone Increased metabolite- mediated tissue toxicity Paracetamol and phenacetin As therapy ( phenobarbitone + hyperbilirubinemia) 18 Liver Microsomal Inhibitors Cimetidine Erythromycin ketoconazole Metronidazole Probenecid Enzyme inhibition may Retard the metabolism and excretion of the inhibitor and coadministered drugs Prolong the action of the inhibitor and co-administered drugs→ increased pharmacological activity. 19 First Pass Metabolism A drug can be metabolized before the drug reaches the systemic circulation so the amount reaching systemic circulation is less than the amount absorbed Where ? Liver ,gut wall, lung Result: low bioavailability Short duration of action 20 Factors affecting drug metabolism Age: the enzyme system at birth especially in preterm baby are functionally imature and especially for oxidation and for conjugation with glucuronic acid. The drugs like chloramphenicol is unable to get conjugated can cause fatal grey baby syndrome in neonates . After first weeks of life the drug metabolic capacity increases rapidly 21 In elderly metabolism is reduced because liver mass and liver blood flow are decreased .Metabolic inactivation of drugs is slowed Drugs persist for longer time and in higher concentration the must be lowered e.g. tricyclic antidepressants , antidysrhythmic drugs. Enzyme induction process is also lessened 22 Pregnancy: Hepatic metabolism is increased This leads to increased clearance of drugs such as phenytoin and theophylline Disease: Acute inflammatory disease of liver (viral ,alcoholic) and cirrhosis affect function of hepatocytes and blood flow through the liver,this results in increased systemic availability of drugs such as propranolol ,labatolol especially which has normally high 1st pass metabolism, and exhibit prolong half life and reduced clearance. Drug metabolism is accelerated in hyperthyroidism 23 Food: some specific dietary factors induce drug metabolizing enzymes e.g. alcohol, charcoal grilled beef, cabbage. Protein malnutrition reduces hepatic metabolizing capacity. 24