Aseptic Meningitis
Bacterial and Non-Bacterial CNS
Infections
EMERGENCY NEUROLOGY LECTURE
SERIES
JULY 7, 2010
Dr. Abdullah Al-Salti R3
CNS INFECTIONS
Overview
Life-threatening problems with high associated mortality and morbidity.
Presentation may be acute, subacute, or chronic.
Clinical findings determined by anatomic site(s) of involvement, infecting pathogen, and host response.
Vulnerability of CNS to the effects of inflammation & edema mandates prompt diagnosis with appropriate therapy if consequences to be minimized.
CNS INFECTIONS
OUT LINE
3.
4.
1.
2.
Bacterial meningitis
Aseptic Meningitis
Viral Meningitis
Viral encephalitis
CNS Infections
Meningitis
• Bacterial, viral, fungal, chemical, carcinomatous
Encephalitis
• Bacterial, viral
Meningoencephalitis
Abscess
• Parenchymal, subdural, epidural
INFECTIONS
4 routes which infectious agents can enter the CNS a) hematogenous spread i) most common
- usually via arterial route
- can enter retrogradely (veins) b) direct implantation i) most often is traumatic ii) iatrogenic (rare) via lumbar puncture iii) congenital (meningomyelocele) c) local extension (secondary to established infections) i) most often from mastoid, frontal sinuses, infected tooth, etc.
d) PNS into CNS i) viruses
- rabies
- herpes zoster
BACTERIAL MENINGITIS
Meningitis refers to an inflammatory process of leptomeninges and CSF.
Meningoencephalitis refers to inflammation to meninges and brain parenchyma.
Meningitis classified: a) acute pyogenic i) usually bacterial meningitis b) aseptic i) usually acute viral meningitis c) chronic i) usually TB, spirochetes, cryptococcus.
Incidence of 3 cases/100,000 population/yr (~25,000 total cases).
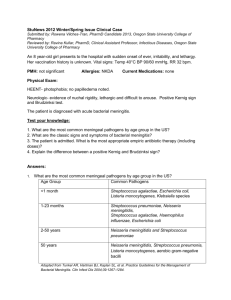
COMMON BACTERIAL PATHOGENS BASED ON
PREDISPOSING FACTOR IN PATIENTS WITH
MENINGITIS
Common Bacterial Pathogens
Predisposing Factor
Age
0-4 wk Streptococcus agalactiae, Escherichia coli,
Listeria monocytogenes, Klebsiella pneumoniae, Enterococcus spp .,
Salmonella spp .
4-12 wk
S. agalactiae, E. coli, L. monocytogenes,
Haemophilus influenzae, Streptococcus pneumoniae, Neisseria meningitidis
3 mo to 18 yr
18-50 yr
>50 yr
H. influenzae, N. meningitidis, S. pneumoniae
S. pneumoniae, N. meningitidis
S. pneumoniae, N. meningitidis, L . monocytogenes , aerobic gram-negative bacilli
Clinical Features
Signs and symptoms:
rapid onset of fever
headache photophobia nuchal rigidity lethargy, malaise
altered mentation seizure vomiting.
van de Beek D, de Gans J, Tunkel AR, et al.
Community-acquired bacterial meningitis in adults. N Engl J Med 2006;354(1):44 – 53.
Clinical Features
Study of 493 adult patients with bacterial meningitis, the presence of the ‘‘ classic triad ’’ of fever , neck stiffness , and altered mental status was present in two-thirds of patients.
fever WAS the most common element, in 95%.
( N Engl J Med 1993;328(1):21 – 8 . )
Older patients with S. pneumoniae meningitis are more likely to have the classic triad.
Weisfelt M, van de Beek D, Spanjaard L, et al. Community-acquired bacterial meningitis in older people. J Am Geriatr Soc
2006;54(10):1500 – 7.
Other studies have shown the classic triad to be less common, with estimates ranging from 21% to 51%.
All cases studied had at least one of the three signs; the absence of the all components of the classic triad excludes the diagnosis in immunocompetent individuals.
Physical examination
A careful neurological examination is important to evaluate for :
• focal deficits
• increased intracranial pressure (ICP).
Examination should include assessment for meningeal irritation
• Brudzinski ’ s sign
• Kernig ’ s sign
findings include purpura or petechia of the skin, which may occur with meningococcemia.
Bacterial meningitis
Investigations
LP
Single most impt diagnostic test.
Mandatory, esp if bacterial meningitis suspected.
Tube #1 – glucose and protein
Tube #2 – cell count and differential
Tube #3 – gram stain and rountine culture, cyrptococcal antigen, AFB stain and culture
Tube #4 – VDRL, or viral studies (PCR)
Opening
Pressure
Glc
Pro
Rbcs
Wbcs
(c/mm3)
Diff
CSF Characteristics
Bacterial Viral Fungal TB
Elevated Slight elevated
Normal or High
Usually high
Low
Very high
Few
>200
Normal Low Low
Normal High High
None
<200
None None
<50 20-30
PMNs Mono Mono Mono
CT Before LP in Patients with
Suspected Meningitis
301 pts with suspected meningitis; 235
(78%) had CT prior to LP
CT abnormal in 56/235 (24%); 11 pts (5%) had evidence of mass effect
Features associated with abnl. CT were:
• age >60,
• immunocompromise,
• H/O CNS dz,
• H/O seizure w/in 7d, &
• selected neuro abnls
Hasbun, NEJM
2001;345:1727
CT head Before LP
(Cont.)
Neuro abnls included altered MS, inability to answer 2 consecutive questions or follow 2
consecutive commands, gaze palsy, abnl visual
fields, facial palsy, arm or leg drift, & abnl language
96/235 pts (41%) who underwent CT had none of features present at baseline
CT normal in 93 of these 96 pts (NPV 97%).
Of the 3 remaining patients, only 1 had mild mass effect on CT, and all 3 underwent lumbar puncture with no evidence of brain herniation
Hasbun, NEJM 2001;345:1727
Consideration for lumbar puncture without neuroimaging
David Somand, MDa,WilliamMeurer, MD
Department of Emergency Medicine, University of Michigan, Taubman Center B1354
SPC #5303, 1500 East Medical Center Drive, Ann Arbor, MI 48109-5303, USA
Department of Neurology, University of Michigan, Taubman Center 1914 SPC #5316, 1500 E.
Medical Center Drive, Ann Arbor, MI 48109-5316, USA
Age less than 60
Immunocompetent
No history of CNS disease
No recent seizure (less than 1 week)
Normal sensorium and cognition
No papilledema
No focal neurologic defecits
Acute bacterail meninigits
MRI
Not generally useful in acute diagnosis
(Pt cooperation; logistics).
Very helpful in investigating potential complications developing later in clinical course such as venous sinus thrombosis or subdural empyema.
Laboratory Testing Helpful in Distinguishing
Bacterial from Viral Meningitis.
CSF lactate .
Elevated CSF lactate concentrations may be useful in differentiating bacterial from nonbacterial meningitis in patients who have not received prior antimicrobial therapy.
study of 78 patients with acute meningitis in which CSF lactate concentrations of >4.2mmol/L were considered to be a positive discriminative factor for bacterial meningitis .
Sens Spec PPV NPV
96%, 100%, 100%, 97%.
Furthermore, other factors (e.g., cerebralhypoxia/ischemia, anaerobic glycolysis,vascular compromise,and metabolism of
CSF leukocytes) also may elevateCSF lactate concentrations.
Therefore, measurement of CSF lactate concentrations is not recommended for patients with suspected communityacquired bacterial meningitis.
Practice Guidelines for the Management of Bacterial Meningitis
Allan R. Tunkel,1 Barry J. Hartman,2 Sheldon L. Kaplan,3 Bruce A. Kaufman,4 Karen
L. Roos,5 W. Michael Scheld,6and Richard J. Whitley7
Laboratory Testing Helpful in Distinguishing
Bacterial from Viral Meningitis.
C-reactive protein (CRP).
Serum CRP concentrations were capable of distinguishing Gram stain – negative bacterial meningitis, with a sensitivity of 96%, a specificity of
93%, and a negative predictive value of 99%.
Measurement of serum CRP concentration may be helpful in considering withholding antimicrobial therapy, on the basis of the data showing that a normal CRP has a high negative predictive value in the diagnosis of bacterial meningitis. Provided the
CSF Gram stain result is negative.
Practice Guidelines for the Management of Bacterial Meningitis
Allan R. Tunkel,1 Barry J. Hartman,2 Sheldon L. Kaplan,3 Bruce A.
Kaufman,4 Karen L. Roos,5 W. Michael Scheld,6and Richard J. Whitley7
Laboratory Testing Helpful in Distinguishing
Bacterial from Viral Meningitis.
procalcitonin concentration.
Elevated serum concentrations of the polypeptide procalcitonin, which are observed in patients with severe bacterial infection, were shown to be useful in differentiating between bacterial and viral meningitis .
In a study of 59 consecutive children hospitalized for meningitis , the sensitivity of measurements of the serum procalcitonin concentration (using a cutoff of 15.0 mg/L) for the diagnosis of bacterial meningitis was 94%, and the specificity was 100%.
In adults, serum concentrations 10.2 ng/mL had a sensitivity and specificity of up to 100% for the diagnosis of bacterial meningitis .
At present, because measurement of serum procalcitonin concentrations is not readily available in clinical laboratories, recommendations on its use cannot be made at this time.
Practice Guidelines for the Management of Bacterial Meningitis
Allan R. Tunkel,1 Barry J. Hartman,2 Sheldon L. Kaplan,3 Bruce A. Kaufman,4 Karen L. Roos,5 W.
Michael Scheld,6and Richard J. Whitley7
Laboratory Testing Helpful in Distinguishing
Bacterial from Viral Meningitis.
PCR.
In patients who present with acute meningitis, an important diagnostic consideration is whether the patient has enteroviral meningitis.
Enteroviral RT-PCR has been tested in clinical settings by numerous investigators and has been found to be more sensitive than viral culture for the detection of enterovirus, with a sensitivity and specificity of 86% – 100% and 92% – 100%, respectively.
lead to shortened patient hospitalization, decreased use of antimicrobial therapy for treatment of bacterial meningitis, and reduced need for ancillary diagnostic tests .
Practice Guidelines for the Management of Bacterial Meningitis
Allan R. Tunkel,1 Barry J. Hartman,2 Sheldon L. Kaplan,3 Bruce A. Kaufman,4 Karen L. Roos,5 W.
Michael Scheld,6and Richard J. Whitley7
BACTERIAL MENINGITIS
Managements
APPROACH TO THE PATIENT WITH SUSPECTED
MENINGITIS
Decision-Making Within the First 30 Minutes
Clinical Assessment
Mode of presentation
Acute (< 24 hrs)
Subacute (< 7 days)
Chronic (> 4 wks)
Historical/physical exam clues
Clinical status of the patient (ABCD)
Integrity of host defenses
Management algorithm for adults with suspected bacterial meningitis.
Practice Guidelines for the Management of Bacterial Meningitis
Overall Goals in Management
1. To promptly recognize the patient with an acute CNS infection syndrome
2. To rapidly initiate appropriate empiric therapy
3. To rapidly and specifically identify the etiologic agent, adjusting therapies as indicated
4. To optimize management of complicating features
BACTERIAL MENINGITIS
Antimicrobial Rx
Therapy is generally IV, high dose, & bolus.
Dosing intervals should be appropriate for drug being administered.
Utilize “ cidal ” therapy whenever possible.
Initiate therapy promptly (ie, within 30 mins)
THE THERAPY OF MENINGITIS
CNS Penetration
Good Diffusion
• Penicillins
• 3 rd & 4th Gen Cephs
• Chloramphenicol
• Rifampin
• TSX
Poor Diffusion
• Early Gen Cephs
• Clindamycin
• AMGs
• Tetracyclines
• Macrolides
EMPIRIC THERAPY OF MENINGITIS IN THE
ADULT
Clinical Setting Likely Pathogens Therapy
Community-acquired S. pneumoniae
N. meningitidis
[Listeria]
[H. influenzae]
Closed head trauma S. pneumoniae
Streptococci q12h
Ceftriaxone
2 gm q12h
+
Vancomycin 1-2 gm 12h
+/-
Ampicillin 2 gm q4h
Pen G 3-4 mu q4h
+
Vancomycin 1-2 gm
EMPIRIC THERAPY OF MENINGITIS IN THE
ADULT
Clinical Setting Likely Pathogens Therapy
High risk patients S. aureus
Compromised hosts Gram negative
Neurosurgical or
Open head injury
Nosocomial
Elderly bacilli
Listeria
Vancomycin 2-3 gm/d
+
Ceftazidime 2 gm q8h
Cefepime 2 gm q8h
[Ceftriaxone 2 gm q12h]
[Cefotaxime 2 gm q4h]
+/-
Ampicillin 2 gm q4h
SPECIFIC THERAPY FOR KNOWN PATHOGENS
Pathogen
S. pneumoniae*
N. meningitidis
Streptococci
H. influenzae
Group B strep
Recommended Therapy
Pen G 18-24 mu/d or
Ampicillin 12 gm/d
[Chloro 75-100 mg/kg/d]
[Ceftriaxone 2-4 gm/d]
Cefotaxime 12 gm/d
[Ceftriaxone 2-4 gm/d]
Pen G 18-24 mu/d or
Ampicillin 12 gm/d
[plus aminoglycoside]
S. aureus
Listeria
SPECIFIC THERAPY FOR KNOWN PATHOGENS
(continued)
Gram negative bacilli
Pseudomonas
Nafcillin 12 gm/d
[Vancomycin 2-3 gm/d]
Ampicillin 12 gm/d or
Pen G 18-24 mu/d
[plus aminoglycoside]
Cefotaxime 12 gm/d
[Ceftriaxone 2-4 gm/d]
Ceftazidime 6-8 gm/d or
Cefepime 6 gm/d
[plus aminoglycoside]
BACTERIAL MENINGITIS
Duration of ATB Rx
Pathogen Duration of Rx (d)
H. influenzae 7
N. meningitidis 7
S. pneumoniae 10-14
L. monocytogenes 14-21
Group B strep 14-21
GNRs 21
NEJ1997;336:708
CORTICOSTEROIDS AND MENINGITIS
Role of steroids still somewhat uncertain.
Recent European study in adults suggested that Rx with dexa associated with ↓ in risk of unfavorable outcome (25% → 15%, RR 0.59)
& in mortality (15% → 7%, RR for death 0.48).
Benefit primarily pts w/S. pneumo.
Dose of dex was 10mg IV q6h X 4d; per protocol, dex given concurrent with or 15-20 mins before 1 st dose of ATBs.
CORTICOSTEROIDS AND MENINGITIS
(Cont)
Only pts with cloudy CSF, + CSF GmS, or CSF WBC count >1000 were enrolled
Accompanying editorial raised concerns about use of steroids in pts with DRSP who are being Rx ’ ed with vanc b/o ↓ in
CNS conc of vanc with concurrent steroid use.
Practically speaking, almost all pts with presumed bacterial meningitis are candidates for at least 1 dose of dexa
NEJM 2002;347:1549
Acute bacterial meningitis
Antibiotic prophylaxis
Is recommended for high-risk exposures to patients with Neisseria or Hib meningitis.(potentially share secretions).
Regimens include :
single-dose ciprofloxacin or ceftriaxone.
rifampin 600 mg every 12 hours for five doses.
There is no indication for prophylaxis for exposure to pneumococcal meningitis.
Quinolone resistance has been reported to Neisseria, and this class of antibiotics is no longer recommended for prophylaxis in parts of the
United States.
David Somand, MDa,WilliamMeurer, MD
Department of Emergency Medicine, University of Michigan, Taubman Center B1354
SPC #5303, 1500 East Medical Center Drive, Ann Arbor, MI 48109-5303, USA
Department of Neurology, University of Michigan, Taubman Center 1914 SPC #5316, 1500 E.
Medical Center Drive, Ann Arbor, MI 48109-5316, USA
PREDICTORS OF ADVERSE CLINICAL OUTCOMES IN
PTS WITH COMMUNITY-ACQUIRED BACTERIAL
MENINGITIS
Retrospecitve study; 269 pts (84% culture +).
Adverse clinical outcome in 36% of pts(Death 27%, neuro deficit
9%).
↓ BP, altered MS, and seizures on presentation all independently associated with adverse clinical outcome.
Adverse outcomes in 5% of low risk pts (0 features), 37% of intermediate risk pts (1 feature), and 63% of high risk pts
(2-3 features).
Delay in administration of appropriate ATB Rx also associated with adverse clinical outcome.
Aronin et al, AIM1998;129:862
Aseptic Meningitis
Aseptic Meningitis
All non-bacterial causes of meningitis
Typically less ill appearing than bacterial meningitis
Most common cause is viral
• HSV
Consider especially in infants presenting with seizure
Usually HSV type II
Treat with acyclovir
• Enterovirus (coxsackie, echovirus)
Typically occurs during late summer and fall
Spread via respiratory secretions and fecal-oral
Affects all ages
Generally self-limited illness
Aseptic Meningitis
Other Viral
• HIV
• Lymphocytic choriomeningitis virus
• Arbovirus
• Mumps
• CMV
• EBV
• VZV
• Adenovirus
• Measles
• Rubella
• Rotavirus
• Influenza and parainfluenza
Aseptic Meningitis
Other infectious
• Borrelia burgdorferi
• Mycobacterium tuberculosis
• Treponema pallidum
• Mycoplasma pneumoniae
• Rickettsia, erlichia, brucella
• Chlamydia
Aseptic Meningitis
Fungal
• Cryptococcus
• Coccidiodes
• Histoplasmosis
Parasitic
• Angiostrongylus
• Toxoplasmosis
Aseptic Meningitis
Medication
• NSAID ’ s
• Bactrim
• Pyridium
Malignancy
• Lymphoma and leukemia
• Metastatic carcinoma
Autoimmune
• Sarcoid
• Behcet ’ s
• SLE
Viral Meningitis
•
Very common clinical course is less fulminant compared to bacterial
Often caused by enteroviruses
Polioviruses
Coxsackieviruses
Echoviruses
Treatment is supportive
VIRAL ENCEPHALITIS
Introduction
Encephalitis is an acute inflammatory process affecting the brain
Viral infection is the most common and important cause, with over 100 viruses implicated worldwide
Symptoms
• Fever
• Headache
• Behavioral changes
• Altered level of consciousness
• Focal neurologic deficits
• Seizures
Incidence of 3.5-7.4 per 100,000 persons per year
Herpesviruses
Herpes simplex
Varicella-zoster
Epstein Barr
Cytomegalovirus
Myxo/paramyxoviruses
Influenza/parainfluenzae
Mumps
Measles
Miscellaneous
Adenoviruses
LCM
Rabies
HIV
VIRAL ENCEPHALITIS
Enteroviruses
Polioviruses
Coxsackieviruses
Echoviruses
Togaviruses
Eastern equine
Western equine
Venezuelan equine
St. Louis
Powasson
California
West Nile
Patient History
Detailed history critical to determine the likely cause of encephalitis.
Prodromal illness, recent vaccination, development of few days → Acute Disseminated Encephalomyelitis
(ADEM) .
Biphasic onset: systemic illness then CNS disease →
Enterovirus encephalitis.
Abrupt onset, rapid progression over few days → HSE.
Recent travel and the geographical context:
• Africa → Cerebral malaria
• Asia → Japanese encephalitis
• High risk regions of Europe and USA → Lyme disease
Recent animal bites → Tick borne encephalitis or
Rabies.
Occupation
• Forest worker, exposed to tick bites
• Medical personnel, possible exposure to infectious diseases.
History cont.
Season
• Japanese encephalitis is more common during the rainy season.
• Arbovirus infections are more frequent during summer and fall.
Predisposing factors:
• Immunosuppression caused by disease and/or drug treatment.
• Organ transplant → Opportunistic infections
• HIV → CNS infections
• HSV-2 encephalitis and Cytomegalovirus infection (CMV)
Drug ingestion and/or abuse
Trauma
Initial Signs
Headache
Malaise
Anorexia
Nausea and Vomiting
Abdominal pain
Developing Signs
Altered LOC – mild lethargy to deep coma.
AMS – confused, delirious, disoriented.
Mental aberrations:
• hallucinations
• agitation
• personality change
• behavioral disorders
• occasionally frank psychosis
Focal or general seizures in >50% severe cases.
Severe focused neurologic deficits.
Neurologic Signs
Virtually every possible focal neurological disturbance has been reported.
Most Common
• Aphasia
• Ataxia
• Hemiparesis.
• Involuntary movements
• Cranial nerve deficits (ocular palsies, facial weakness)
Other Causes of
Encephalopathy
Anoxic/Ischemic conditions
Metabolic disorders
Nutritional deficiency
Toxic (Accidental & Intentional)
Systemic infections
Critical illness
Malignant hypertension
Mitochondrial cytopathy (Reye ’ s and MELAS syndromes)
Hashimoto ’ s encephalopathy
Traumatic brain injury
Epileptic (non-convulsive status)
CJD (Mad Cow)
Differential Diagnosis
Distinguish Etiology
• (1) Bacterial infection and other infectious conditions
• (2) Parameningeal infections or partially treated bacterial meningitis
• (3) Nonviral infectious meningitides where cultures may be negative (e.g., fungal, tuberculous, parasitic, or syphilitic disease)
• (4) Meningitis secondary to noninfectious inflammatory diseases
VIRAL ENCEPHALITIS
DIAGNOSIS.
LP:
CSF usually colorless
- slightly pressure
- initially a neutrophilic pleocytosis, which rapidly converts to lymphocytes
- proteins are
- glucose is normal
PCR for HSE and other viral infection is diagnostic .
VIRAL ENCEPHALITIS
DIAGNOSIS.
MRI:
May show temporal or orbitofrontal cortex enhancement or
edema in HSE.
In most other acute viral encephalities , neuroimaging finding are nonspecific.
Can exclude subdural bleeds, tumor, and sinus thrombosis.
EEG:
• Non specific
• Diffuse slowing .
• Focal abnormalities in the temporal region . HSV
Brain biopsy :
Reserved for patients who are worsening, have an undiagnosed lesion after scan, or a poor response to acyclovir.
Treatment.
Only HSV disease has specific therapy available. Acyclovir is capable of improving patient outcome.
•
• dose : 10 mg/kg intravenously every 8 hours.
Duration 14-21 days.
ganciclovir can be used in CMV infections.
pleconaril has shown promise in enteroviral.
Outcomes
Outcomes are variable depending on etiology.
EEE and St. Louis encephalitis generally have high mortality rates and Severe neurologic sequelae among survivors.
WNV is associated with significant morbidity and morality.
Mortality of HSV encephalitis before acyclovir was 60% to 70%, and with treatment approximately 30%.
Cognitive disability,seizures, and motor deficits are common sequelae seen among survivors
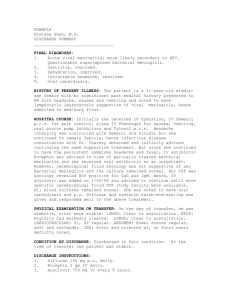
Bacterial and Non-Bacterial CNS
Infections
EMERGENCY NEUROLOGY LECTURE
SERIES
JULY 7, 2010
Dr. Abdullah Al-Salti R3