MAX - Scrubs
advertisement

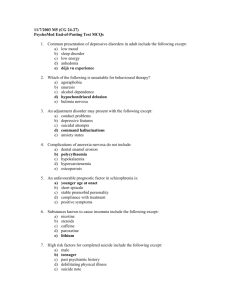
MAX 1. Action point: A prodromal phase often precedes the first presentation of schizophrenia. Max may have been experiencing this for the 9 months prior to this presentation. Describe the prodromal phase and how this impacts on a client’s recovery. A prodromal phase often precedes the first presentation of schizophrenia. Max may have been experiencing this for the 9 months prior to this presentation. Describe the prodromal phase and how this impacts on a client’s recovery. Prodromal Phase – earliest manifestation of a psychotic disorder which often develops in early adolescence: - Sleep/appetite disturbance - Marked unusual behavior - Feeling different to others (blunted or incongruent) - Speech difficult to follow - Marked pre occupation with unusual ideas - Ideas of reference things having special meaning - Persistent feeling of unreality - Changes in a way things appear, sound or smell Prodromal features in Schizophrenia are vague and not specific. Although when the illness becomes severe it can be diagnosed and prodromal features can be identified. 2. Action point: Educating clients and their families about the nature and process of the mental health act is an important role for the mental health nurse. Outline for Max’s parents, the criteria for a person to be under the Mental Health Act and give the family an overview of how antipsychotic /anxiolytic medications are used in the management of psychosis. Max’s parents also ask you about the interview taking place in the other room. Describe your response. Educating clients and their families about the nature and process of the mental health act is an important role for the mental health nurse. 722.724: 111A Semester 1, 2011 The Mental Health (Compulsory Assessment and Treatment) Act 1992 defines the circumstances in which a person may be required to undergo compulsory psychiatric assessment and treatment. The Act aims to ensure that both vulnerable individuals and the public are protected from harm with its rights of patients and proposed patients and aims to protect those rights. Under this act, the clients are entitled to: • To have their culture respected • To have an interpreter present • To be supported by whanau or friends • To have visitors and access to a phone • The company of others • Not to be video or audio taped • Access to a District Inspector • Full information on your status • Receive appropriate health care • To be informed of benefits of treatment • To be informed of possible side effects • To seek a second independent opinion • To have access to legal advice • To have a Judicial Review The Summary of the Procedure for Assessment and Treatment under the Mental Health Act 1992: • Section • Section • Section • Section • Section • Section • Section 8A Application for assessment 8B Medical certificate 9 Notice to attend an assessment 10 Certificate of preliminary assessment 11 Further assessment and treatment (5 days) 13 (2 weeks) 15 (4 weeks) Community Treatment Orders • Section 29 Can last up to 6 months Can be extended or made indefinite Can be converted to an inpatient order Must attend for treatment Inpatient Orders • Section 30 Provides for compulsory treatment Lasts for up to six months Can be extended or made indefinite Can be converted to a community treatment order • Section 31 Provides for conditional leave 722.724: 111A Semester 1, 2011 Revoked if conditions not adhered to Outline for Max’s parents, the criteria for a person to be under the Mental Health Act and give the family an overview of how antipsychotic /anxiolytic medications are used in the management of psychosis Mental Disorder Intermittent disorder – repeated or prolonged episodes of illness - Severe consequences during phases of illness; such as severe violence to self or others - Early loss of insight during an episodes of illness, with a pattern of failing to be able to take the necessary steps to halt the development of illness - Changeable insight consistent decision = inability to maintain o Degree of disorder – seriously diminishes the capacity of look after himself or herself i.e. failure to comply with meds (i.e. insulin); self-neglect such as inattention to cooking and high risk fire; a person in a manic state who overspends to such an extent that he or she finds himself or herself bankrupt when symptoms of mania are no longer present o Poses a serious danger to the health or safety of that person or others o Threshold for application for compulsory treatment o Abnormal state of mind o Disorders of volition and cognition (Volition: depression stupor; catatonic excitement/withdrawal;passisivity;lack of motivation) o Head injury resulting to disturbance in behavior o Personality disorder o Substance abuse 722.724: 111A Semester 1, 2011 Antipsychotics – previously referred to as major tranquilizers or neuroleptics are effective for the treatment of a variety of psychotic symptoms. All available antipsychotics antagonize dopamine (d2) receptors in vitro. Max’s parents also ask you about the interview taking place in the other room. Describe your response. Privacy Act 1993 3. Action point: Describe what needs to be undertaken for a holistic assessment of Max in a first assessment interview. Psychiatric Assessment The purpose of the psychiatric assessment is to develop an understanding of the person presenting for help. It involves taking a basic psychiatric history and a mental status assessment. The following information is required in conducting a comprehensive psychiatric assessment: 1. Identifying Information Includes; name, age, sex, present address, telephone number, languages spoken, general practitioner, marital status, occupation and next of kin. 2. Reason for Referral This should include; Who has asked for the client to be seen and why The nature of the problem Events that led to this presentation Any recent suicide attempts Any recent episodes of self-harm 3. Presenting Problem and/or precipitating factors Information needed include; Specific symptoms that are present and their duration Time relationships between the onset or exacerbation of symptoms and the presence of social stressors/physical illness Any disturbance in mood, appetite, sexual drive or sleep Any treatments given by other doctors or specialists for this problem The individual response to treatment 4. Mental Health/Medical/Drug History Information required includes the number of admissions to mental health inpatient units, number of episodes of self-harm, attempted suicide or occasions of assault, and an indication of any mental health treatments received. This information is usually obtained from the client, previous clinical notes, a letter from the doctor, or history provided by relatives or friends. 722.724: 111A Semester 1, 2011 5. Psychosocial/Relationship History This outlines circumstances that are significant for understanding current issues, and covers many aspects of the individual’s life, such as relationships, family background, work or school history and, possibility, developmental stages. 6. Determining Risk Factors Several risk factors need to be assessed for each client; Harm to others, harm to self, suicide, absconding, vulnerability to exploitation or abuse (sexual) Vulnerability to exploitation or abuse (violence) 7. Assessment of Strengths The focus on strengths of individuals and their opportunities rather than pathology creates opportunity for growth. The strengths identified in this conceptual framework include the individual’s interests, aspirations, skills, competencies and talents. 8. Mental State Examination (BATOMI) A semi- structured interview used mainly as a screening tool to assess a person’s current neurological and psychological status along several components. The exam involves observations as well as an interview. It involves; o Appearance and Behaviour o Speech, Mood and Affect o Form of Thought o Thought Content o Perception o Sensorium and Cognition 9. Physical Assessment Involves past and present health status, physical functions (elimination, activity and exercise, sleep, appetite and nutrition, hydration, self-care), Laboratory results 20. Spiritual Assessment It is important because it provides a deeper understanding of the client, their social setting and the possible origins of the problem. 21. Cultural Assessment Mental health nurses need to engage the client and the family so that appropriate care should be given. In New Zealand, the principle of Cultural Safety is applied to provide quality care that is also culturally sensitive to the patients. 22. Triage Assessment Refers to the decision-making process that occurs when alternatives for acute care are being considered 722.724: 111A Semester 1, 2011 ADAM SMITH 1. Action point: What information are you going to pass on to Agnes? Schizophrenia is a chronic, severe, and disabling brain disorder that has affected people throughout history. People with the disorder may hear voices other people hear. They may believe other people are reading minds, controlling their thoughts, or plotting to them. This can terrify people with the illness and them withdrawn or extremely agitated. People with schizophrenia may not make sense when they talk. They may sit for hours without moving or talking. Sometimes people with schizophrenia seem perfectly fine until they talk about what they are really thinking. The symptoms of schizophrenia categories: positive symptoms, cognitive symptoms don't their harm make fall into three broad negative symptoms, and Positive symptoms Positive symptoms are psychotic behaviours not seen in healthy people. People with positive symptoms often "lose touch" with reality. These symptoms can come and go. Sometimes they are severe and at other times hardly 722.724: 111A Semester 1, 2011 noticeable, depending on whether the individual receiving treatment. They include the following: is Hallucinations are things a person sees, hears, smells, or feels that no one else can see, hear, smell, or feel. "Voices" are the most common type of hallucination in schizophrenia. Many people with the disorder hear voices. The voices may talk to the person about his or her behaviour, orders the person to do things, or warn the person of danger. Sometimes the voices talk to each other. People with schizophrenia may hear voices for a long time before family and friends notice the problem. Other types of hallucinations include seeing people or objects that are not there, smelling odours that no one else detects, and feeling things like invisible fingers touching their bodies when no one is near. Delusions are false beliefs that are not part of the person's culture and do not change. The person believes delusions even after other people prove that the beliefs are not true or logical. People with schizophrenia can have delusions that seem bizarre, such as believing that neighbours can control their behaviour with magnetic waves. They may also believe that people on television are directing special messages to them, or that radio stations are broadcasting their thoughts aloud to others. Sometimes they believe they are someone else, such as a famous historical figure. They may have paranoid delusions and believe that others are trying to harm them, such as by cheating, harassing, poisoning, spying on, or plotting against them or the people they care about. These beliefs are called "delusions of persecution." Thought disorders are unusual or dysfunctional ways of thinking. One form of thought disorder is called "disorganized thinking." This is when a person has trouble organizing his or her thoughts or connecting them logically. They may talk in a garbled way that is hard to understand. Another form is called "thought blocking." This is when a person stops speaking abruptly in the middle of a thought. When asked why he or she stopped talking, the person may say that it felt as if the thought had been taken out of his or her head. Finally, a person with a thought disorder might make up meaningless words, or "neologisms." Movement disorders may appear as agitated body movements. A person with a movement disorder may repeat certain motions over and over. In the other extreme, a person may become catatonic. Catatonia is a state in which a person does not move and does not respond to others. Catatonia is rare today, but it was more common when treatment for 722.724: 111A Semester 1, 2011 schizophrenia was not available."Voices" are common type of hallucination in schizophrenia. the most Negative symptoms Negative symptoms are associated with disruptions to normal emotions and behaviours. These symptoms are harder to recognize as part of the disorder and can be mistaken for depression or other conditions. These symptoms include the following: Flat affect (a person's face does not move or he or she talks in a dull or monotonous voice) Lack of pleasure in everyday life Lack of ability to begin and sustain planned activities Speaking little, even when forced to interact. People with negative symptoms need help with everyday tasks. They often neglect basic personal hygiene. This may make them seem lazy or unwilling to help themselves, but the problems are symptoms caused by the schizophrenia. Cognitive symptoms Cognitive symptoms are subtle. Like negative symptoms, cognitive symptoms may be difficult to recognize as part of the disorder. Often, they are detected only when other tests are performed. Cognitive symptoms include the following: Poor "executive functioning" (the ability to understand information and use it to make decisions) Trouble focusing or paying attention Problems with "working memory" (the ability to use information immediately after learning it). How is schizophrenia treated? Because the causes of schizophrenia are still unknown, treatments focus on eliminating the symptoms of the disease. Treatments include antipsychotic medications and various psychosocial treatments. Antipsychotic medications Clozapine (Clozaril) is an effective medication that treats psychotic symptoms, hallucinations, and breaks with reality. But clozapine can sometimes cause a serious problem called agranulocytosis, which is a loss of the white blood cells that help a person fight infection. People who take clozapine must get their white blood cell counts checked every week or two. This problem and the cost of blood tests make treatment with clozapine difficult for many people. But clozapine is potentially helpful for 722.724: 111A Semester 1, 2011 people who do not respond to other antipsychotic medications. Other atypical antipsychotics were also developed. None cause agranulocytosis. Examples include: Risperidone (Risperdal) Olanzapine (Zyprexa) Quetiapine (Seroquel) Ziprasidone (Geodon) Aripiprazole (Abilify) Paliperidone (Invega). When a doctor says it is okay to stop taking a medication, it should be gradually tapered off, never stopped suddenly. What are the side effects? Some people have side effects when they start taking these medications. Most side effects go away after a few days and often can be managed successfully. People who are taking antipsychotics should not drive until they adjust to their new medication. Side effects of many antipsychotics include: Drowsiness Dizziness when changing positions Blurred vision Rapid heartbeat Sensitivity to the sun Skin rashes Menstrual problems for women. Atypical antipsychotic medications can cause major weight gain and changes in a person's metabolism. This may increase a person's risk of getting diabetes and high cholesterol. A person's weight, glucose levels, and lipid levels should be monitored regularly by a doctor while taking an atypical antipsychotic medication. Typical antipsychotic medications can cause side effects related to physical movement, such as: Rigidity Persistent muscle spasms Tremors Restlessness. Long-term use of typical antipsychotic medications may lead to a condition called tardive dyskinesia (TD). TD causes muscle movements a person can't control. The movements commonly happen around the mouth. TD can range from mild to severe, and in some people the problem cannot be cured. Sometimes people with TD recover partially or fully after they stop taking the medication. TD happens to fewer people who take the atypical antipsychotics, but some people may still get TD. People 722.724: 111A Semester 1, 2011 who think that they might have TD should check with their doctor before stopping their medication. How are antipsychotics taken and how do people respond to them? Antipsychotics are usually in pill or liquid form. Some anti-psychotics are shots that are given once or twice a month. Symptoms of schizophrenia, such as feeling agitated and having hallucinations, usually go away within days. Symptoms like delusions usually go away within a few weeks. After about six weeks, many people will see a lot of improvement. However, people respond in different ways to antipsychotic medications, and no one can tell beforehand how a person will respond. Sometimes a person needs to try several medications before finding the right one. Doctors and patients can work together to find the best medication or medication combination, as well as the right dose. Some people may have a relapse -- their symptoms come back or get worse. Usually, relapses happen when people stop taking their medication, or when they only take it sometimes. Some people stop taking the medication because they feel better or they may feel they don't need it anymore. But no one should stop taking an antipsychotic medication without talking to his or her doctor. When a doctor says it is okay to stop taking a medication, it should be gradually tapered off, never stopped suddenly Psychosocial treatments Psychosocial treatments can help people with schizophrenia that is already stabilized on antipsychotic medication. Psychosocial treatments help these patients deal with the everyday challenges of the illness, such as difficulty with communication, self-care, work, and forming and keeping relationships. Learning and using coping mechanisms to address these problems allow people with schizophrenia to socialize and attend school and work. Patients who receive regular psychosocial treatment also are more likely to keep taking their medication, and they are less likely to have relapses or be hospitalized. A therapist can help patients better understand and adjust to living with schizophrenia. The therapist can provide education about the disorder, common symptoms or problems patients may experience, and the importance of staying on medications. Illness management skills. People with schizophrenia can take an active role in managing their own illness. Once patients learn basic facts about schizophrenia and its 722.724: 111A Semester 1, 2011 treatment, they can make informed decisions about their care. If they know how to watch for the early warning signs of relapse and make a plan to respond, patients can learn to prevent relapses. Patients can also use coping skills to deal with persistent symptoms. Integrated treatment for co-occurring substance abuse. Substance abuse is the most common co-occurring disorder in people with schizophrenia. But ordinary substance abuse treatment programs usually do not address this population's special needs. When schizophrenia treatment programs and drug treatment programs are used together, patients get better results. Rehabilitation. Rehabilitation emphasizes social and vocational training to help people with schizophrenia function better in their communities. Because schizophrenia usually develops in people during the critical careerforming years of life (ages 18 to 35), and because the disease makes normal thinking and functioning difficult, most patients do not receive training in the skills needed for a job. Rehabilitation programs can include job counselling and training, money management counselling, help in learning to use public transportation, and opportunities to practice communication skills. Rehabilitation programs work well when they include both job training and specific therapy designed to improve cognitive or thinking skills. Programs like this help patients hold jobs, remember important details, and improve their functioning. Family education. People with schizophrenia are often discharged from the hospital into the care of their families. So it is important that family members know as much as possible about the disease. With the help of a therapist, family members can learn coping strategies and problem-solving skills. In this way the family can help make sure their loved one sticks with treatment and stays on his or her medication. Families should learn where to find outpatient and family services. Cognitive behavioural therapy. Cognitive behavioural therapy (CBT) is a type of psychotherapy that focuses on thinking and behaviour. CBT helps patients with symptoms that do not go away even when they take medication. The therapist teaches people with schizophrenia how to test the reality of their thoughts and perceptions, how to "not listen" to their voices, and how to manage their symptoms overall. CBT can help reduce the severity of symptoms and reduce the risk of relapse. 722.724: 111A Semester 1, 2011 Self-help groups. Self-help groups for people with schizophrenia and their families are becoming more common. Professional therapists usually are not involved, but group members support and comfort each other. People in self-help groups know that others are facing the same problems, which can help everyone feel less isolated. The networking that takes place in self-help groups can also prompt families to work together to advocate for research and more hospital and community treatment programs. Also, groups may be able to draw public attention to the discrimination many people with mental illnesses face. Short term in the inpatient setting Principles of treatment for the first episode Medication Proper treatment of the first psychotic episode is of the utmost importance. Inadequate management at this stage may foster the development of secondary Consequences which can snowball and lead to a substantial deterioration in long-term outcome. For instance, lack of insight (i.e. unawareness of illness) is A frequently encountered problem in schizophrenia. If the degree of insight is low after the first episode, it can lead to reduced compliance to treatment, which In turn can increase the relapse rate and worsen the longterm outcome. Likewise, residual psychotic symptoms after the first episode may affect social and occupational functioning of patients and indirectly predispose them to stressful experiences (eg relationship or occupational problems). Difficulties like these Lead to relapses and a poor long-term outcome. Hence, the thorough and vigorous treatment of the first episode is very important. Maintenance therapy One further issue is the length of maintenance therapy needed after a single episode of illness. Existing data suggests that a number of patients may not suffer a second episode even without maintenance treatment.44 Unfortunately, it is not yet possible to identify those who will relapse and those who will not.28 As yet, data from double-blind controlled studies that specifically address the optimal length of maintenance therapy are not available.28,45 It appears, however, that continuing medication after the first episode seems to reduce the relapse rate in the subsequent 12 months from approximately 70% to approximately 40%.46 Management of depressive symptoms and suicide risk 722.724: 111A Semester 1, 2011 Depression is common in first-episode schizophrenic patients, with prospective studies reporting rates of identifiable depressive syndrome of around 50% of First episode patients. The actual rate of depressive symptoms detected varied considerably between individual studies (from 20% to 80%), depending on The rating instruments used. In most cases, depressive symptoms are worse at the time of the acute episode and tend to subside as the psychosis comes under Control. If depressive symptoms persist, antidepressant therapy should be commenced. The risk of suicide occurring is substantially increased in first-episode schizophrenia, especially among male patients. Psychosocial intervention Apart from medication, psychosocial rehabilitation efforts are particularly important for managing negative symptoms. Negative symptoms can be substantially Present in the first episode. Vigorous rehabilitation directed at these symptoms is particularly important in minimising secondary disabilities. Competence in social skills is also important in sustaining a social support network and is a crucial element in long-term management. A further disability is the presence of Substantial neurocognitive deficits. By giving adequate medication treatment, some of these deficits may improve with time, but the improvement takes Longer than does the improvement in symptoms. The efficacy of cognitive remediation programmes in reducing neurocognitive deficits is still not established. In general, it is known that a high level of expressed emotion among carers of schizophrenics is predictive of more frequent relapses. Family behavioural therapy may be effective in modifying the amount of expressed motion and the lower relapse rate in selected patients. 722.724: 111A Semester 1, 2011 References: Elder, R., Evans, K. & Nizette, D. (2009). Psychiatric and mental health nursing (2nd ed.). Sydney: Mosby. Johannessen, J. O. (2001). Early recognition and intervention: The key to success in the treatment of schizophrenia?. Dis Manage Health Outcomes, 9(6), 317-327. 722.724: 111A Semester 1, 2011